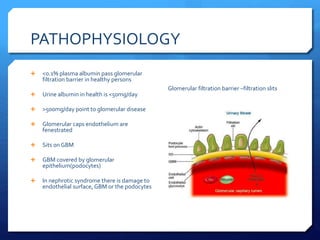
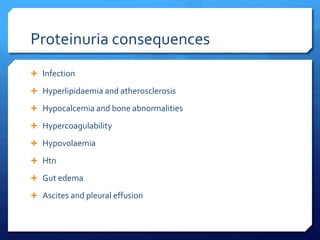
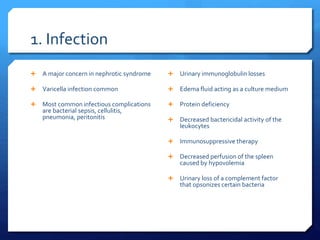
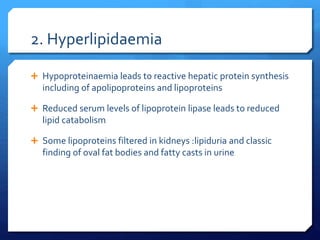
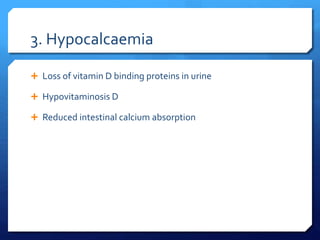
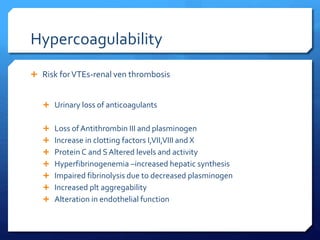
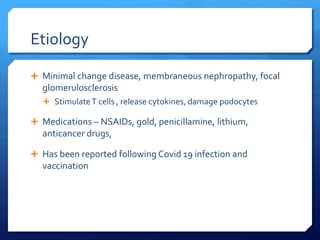
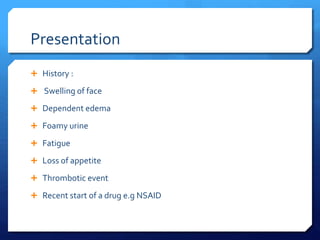
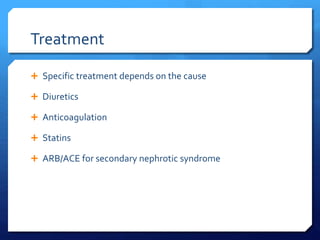
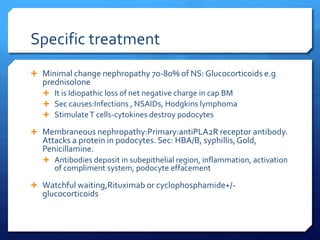
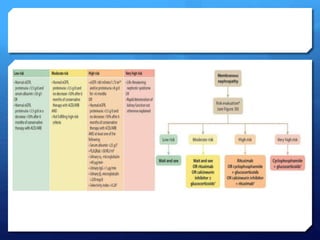
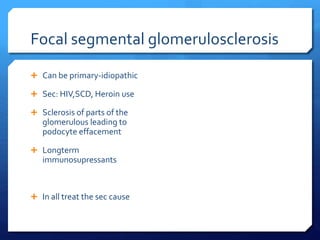
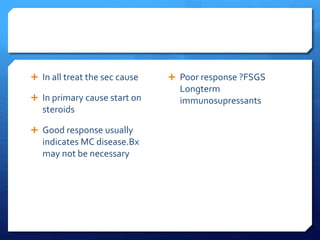
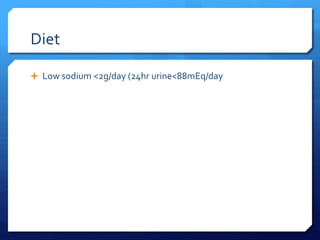
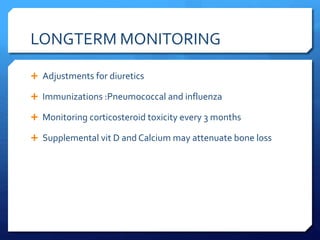
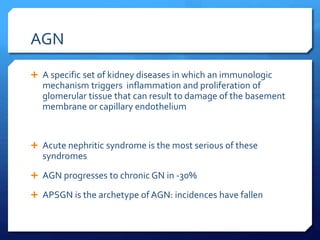
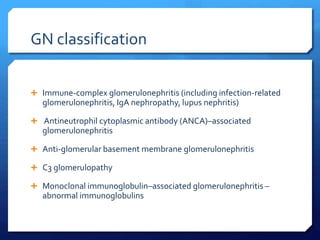
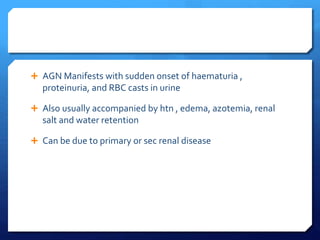
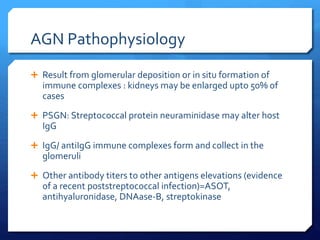
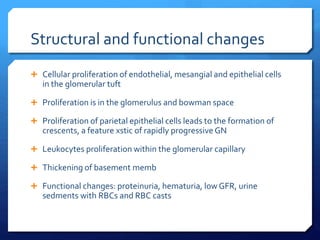
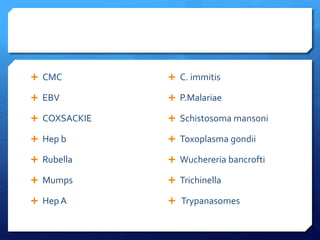
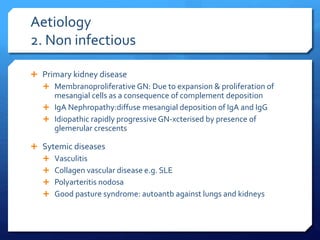
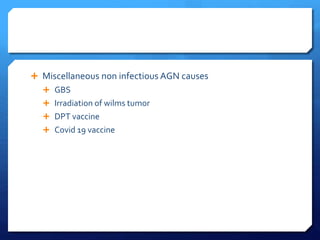
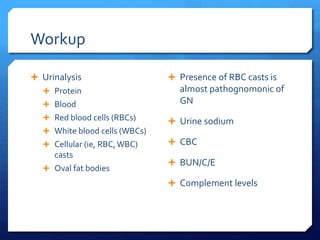
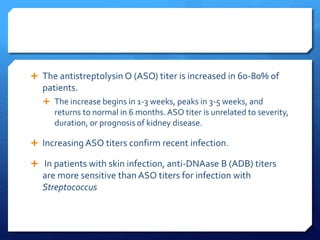
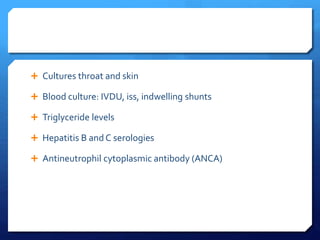
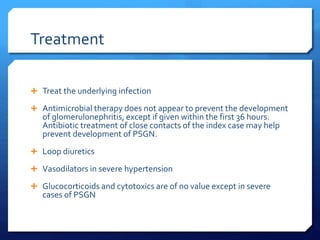
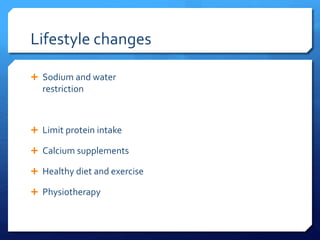
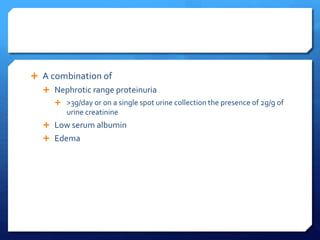
This document discusses glomerulonephritis (GN) and nephrotic syndrome. It begins by defining acute glomerulonephritis (AGN) as a set of kidney diseases caused by immunological inflammation and proliferation in the glomeruli. It then covers the classification, etiology, pathophysiology, presentation, workup, treatment and prognosis of AGN. Nephrotic syndrome is defined as proteinuria, hypoalbuminemia, edema and low serum albumin. The pathophysiology, causes, complications and treatment of nephrotic syndrome are also outlined.



![ May occur in typical form or
in association with nephritic
syndrome
Classification
Primary
Minimal-change
nephropathy
Focal glomerulosclerosis
Membranous nephropathy
Hereditary nephropathies
secondary
Diabetes mellitus
Lupus erythematosus
Viral infections (eg,
hepatitis B, hepatitis C,
human immunodeficiency
virus [HIV] )
Amyloidosis and
paraproteinemias
Preeclampsia
Allo-antibodies from
enzyme replacement
therapy](https://image.slidesharecdn.com/glomerulonephritis-240405024803-911b2a8d/85/GLOMERULONEPHRITIS-disease-description-pptx-28-320.jpg)