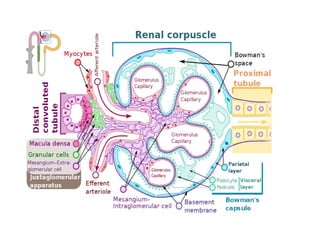
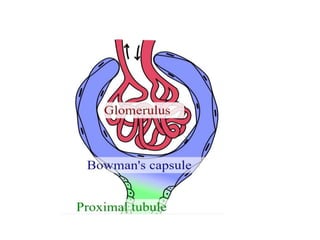
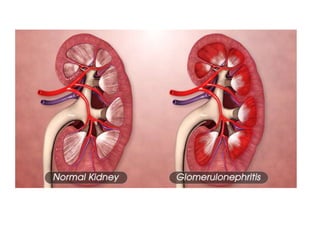
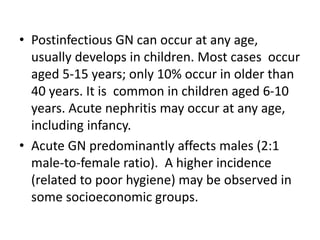
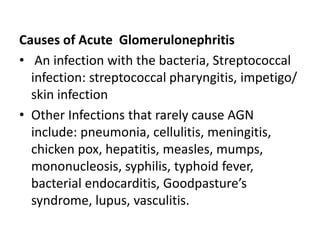
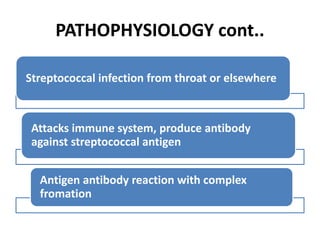
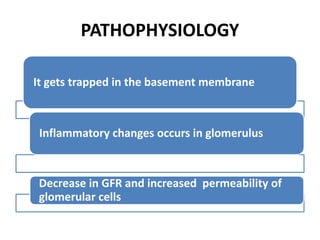
Primary glomerular diseases include various forms of glomerulonephritis and nephrotic syndrome. Acute glomerulonephritis is defined by the sudden onset of hematuria, proteinuria, and red blood cell casts. It is caused by an immunological reaction, often due to a streptococcal infection, that results in inflammation and proliferation in the glomerulus. Symptoms include edema, hypertension, and decreased kidney function. Treatment involves a low sodium diet, fluid restriction, antibiotics, corticosteroids, diuretics, and dialysis if needed. With treatment, most cases of acute glomerulonephritis resolve though some may progress to chronic kidney disease.