The document provides tips for using a PowerPoint presentation on gastroesophageal reflux disease (GERD). It suggests:
1. Using blank slides to elicit what students already know about each topic before presenting new information
2. Repeating this process of blank slide then information slide three times for active learning
3. The presentation can be used for self-study as well by reviewing the notes and bibliography
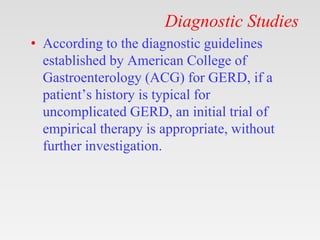
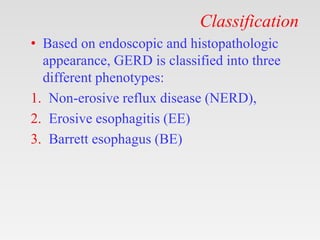
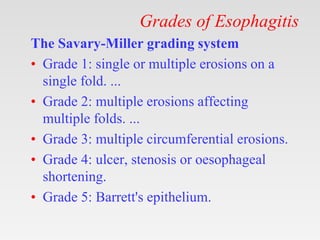
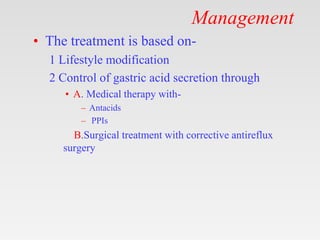
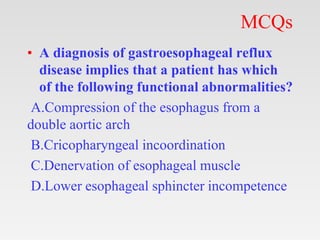
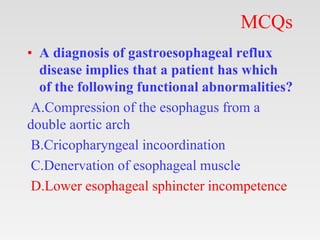
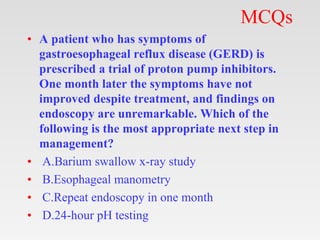
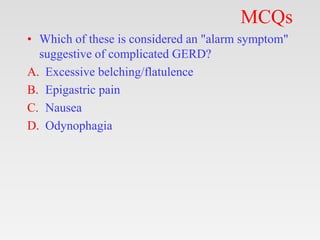
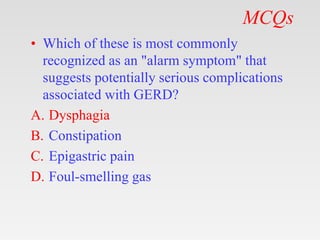
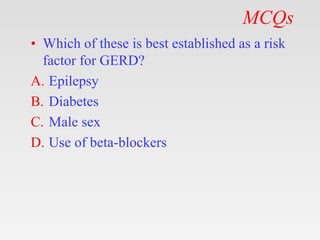
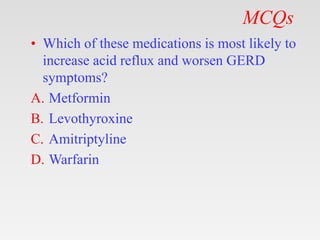
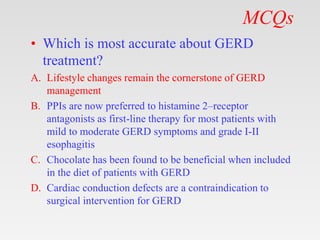
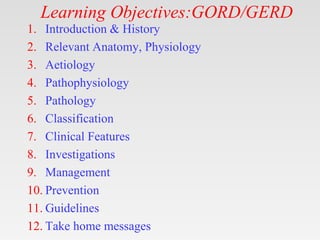
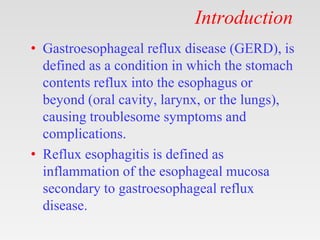
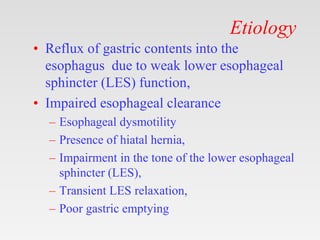
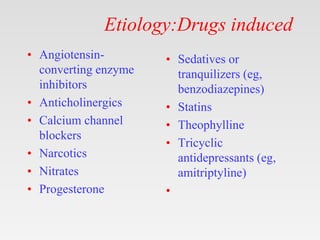
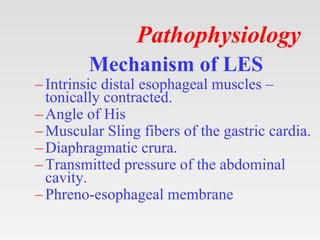
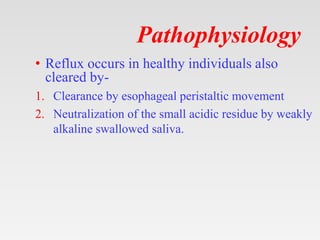
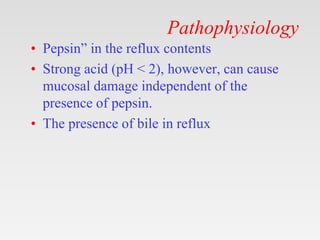
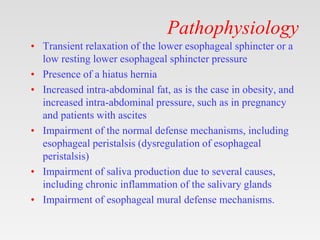
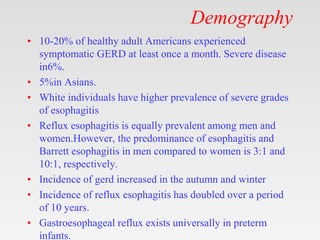
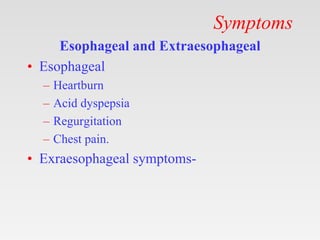
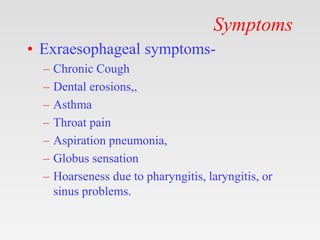
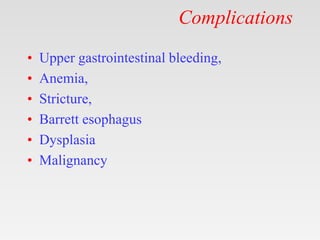
The presentation covers learning objectives and sections on introduction/history, etiology, pathophysiology, clinical features, investigations, management, and multiple choice questions. It provides detailed information on each topic in an engaging format designed for teaching.











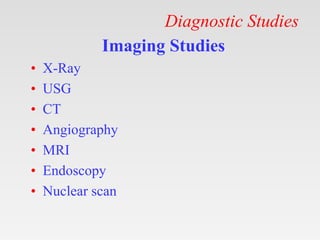
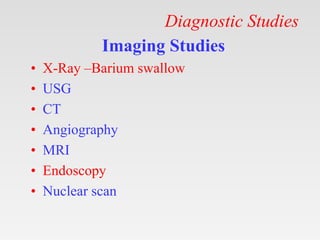
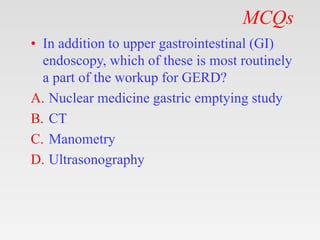
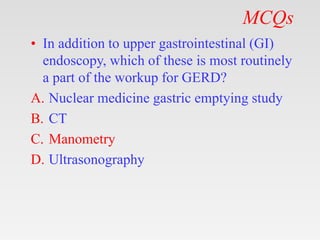
![Diagnostic Studies
• Esophagogastroduodenoscopy (EGD) (or,
upper gastrointestinal [GI] endoscopy) with
biopsy,
• 24-hour ambulatory pH study,
• Manometry,
• Barium contrast study,
• Gastric emptying study.](https://image.slidesharecdn.com/gerdrefluxoesophagitis-230514164922-73d90401/85/GERD-Reflux-Oesophagitis-pptx-31-320.jpg)