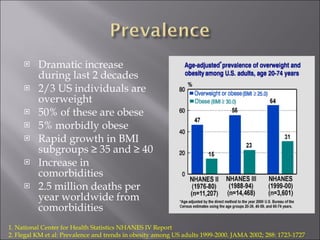
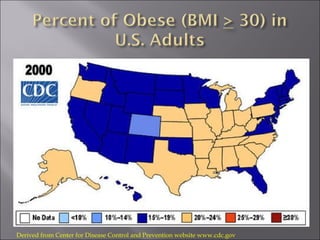
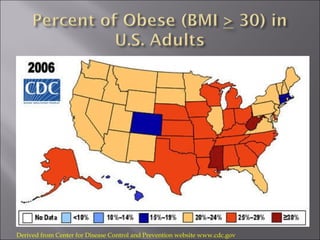
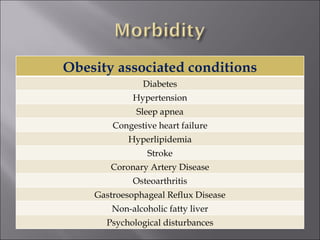
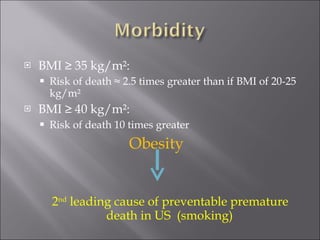
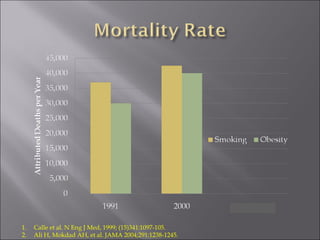
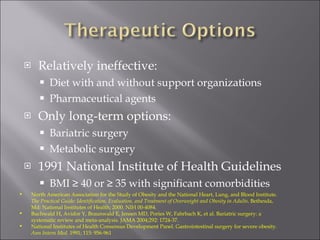
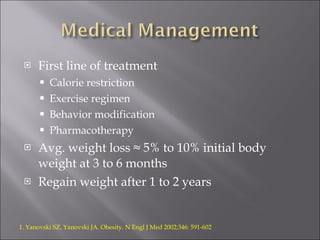
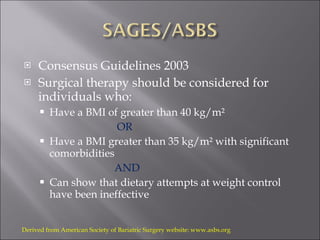
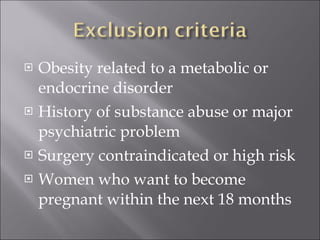
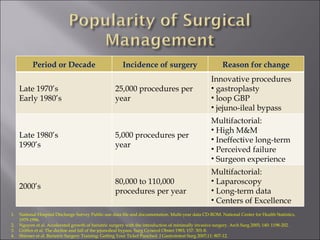
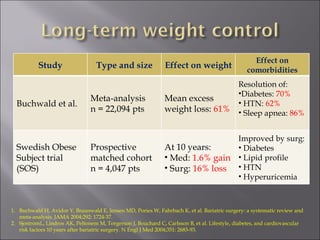
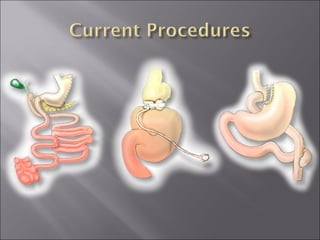
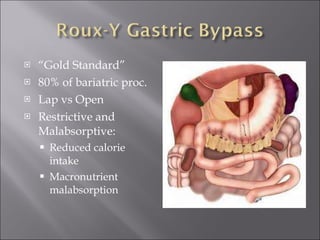
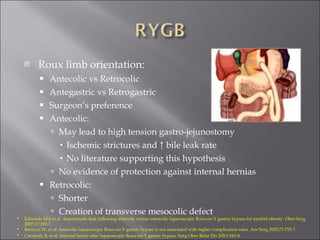
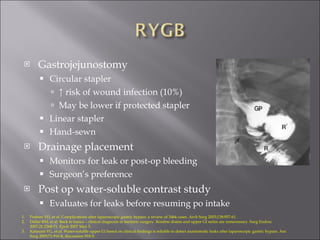
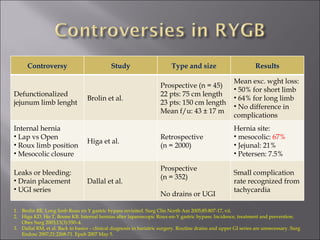
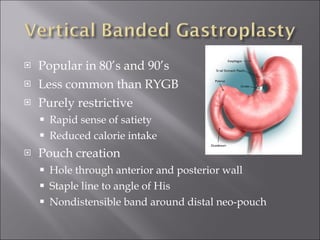
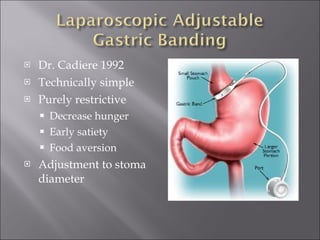
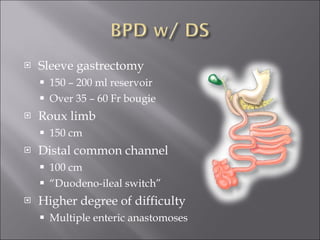
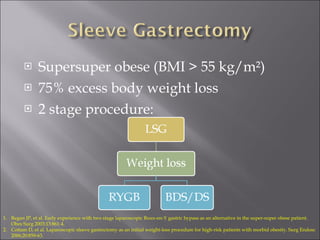
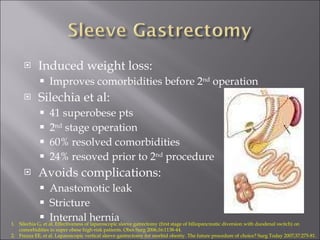
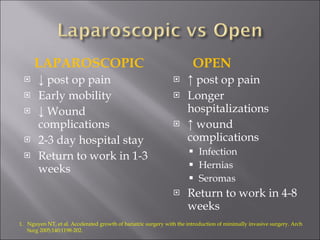
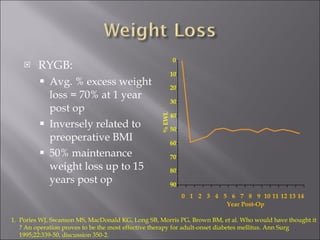
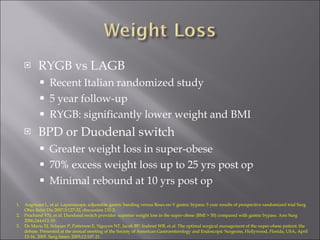
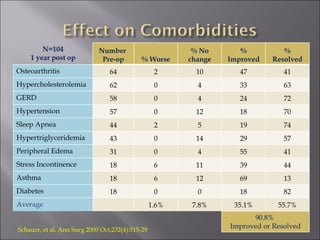
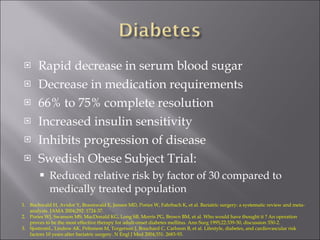
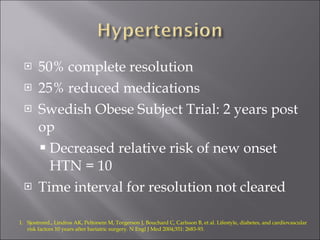
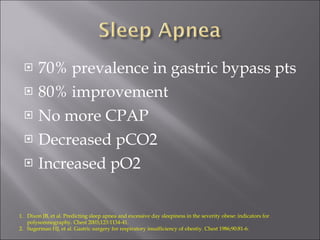
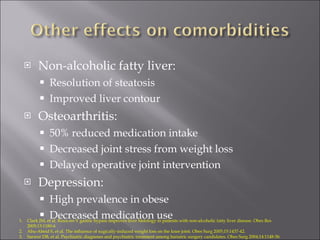
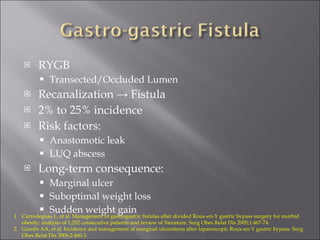
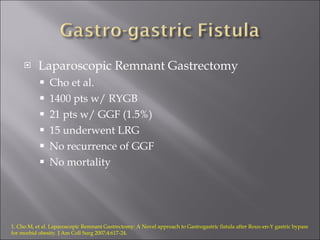
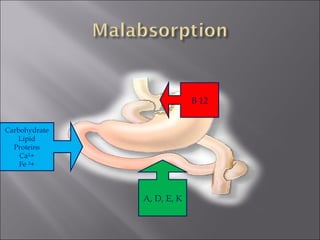
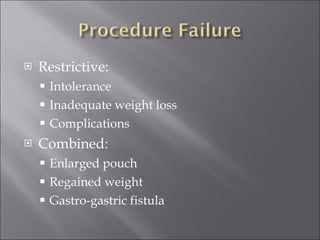
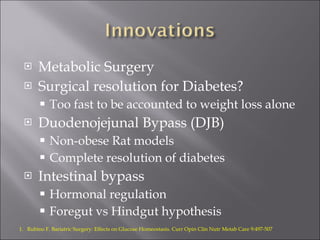
The document summarizes research on the rise of obesity in the United States and treatment options. It finds that over the last two decades, about two-thirds of Americans are overweight or obese. While diet and medication are often ineffective long-term, bariatric surgery has been shown to significantly help with weight loss and resolution of related health conditions like diabetes and hypertension. The risks and outcomes of different bariatric procedures like Roux-en-Y gastric bypass and sleeve gastrectomy are discussed.