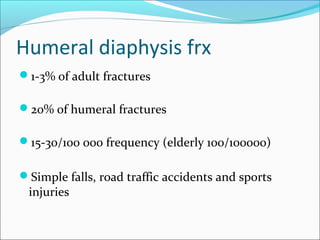
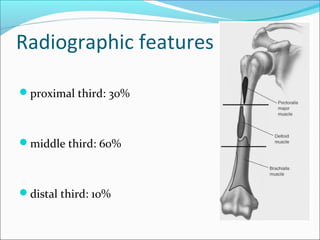
1) Humeral shaft fractures make up 1-3% of adult fractures and are most commonly caused by falls or accidents. They can be classified based on location and features on x-rays.
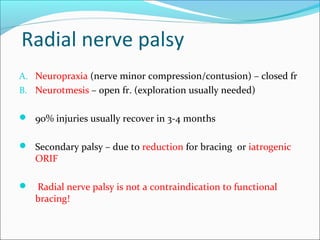
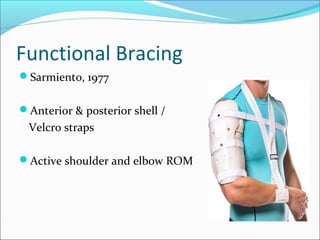
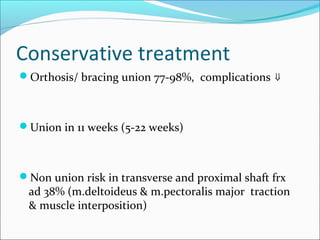
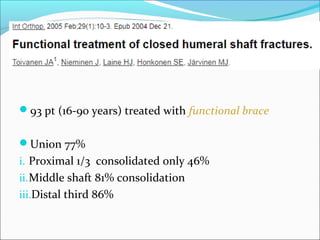
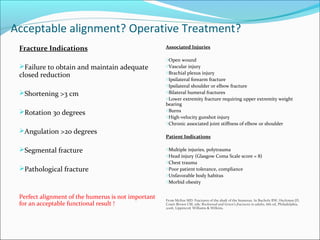
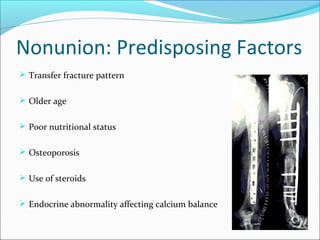
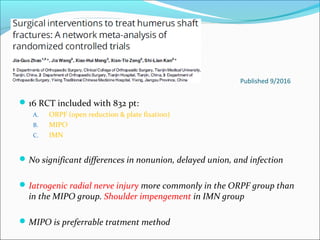
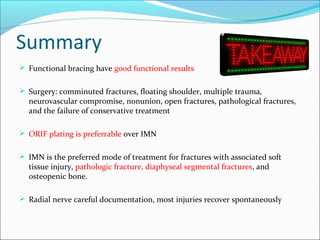
2) Treatment depends on factors like patient age, fracture pattern, and stability. Conservative treatment with bracing has union rates of 77-98% but risks shoulder and elbow stiffness. Surgery is preferred for unstable or complex fractures.
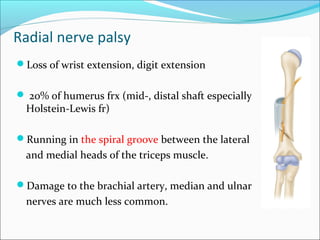
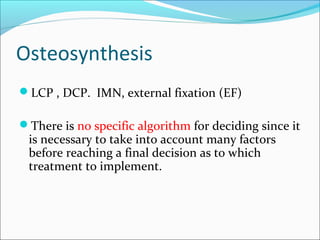
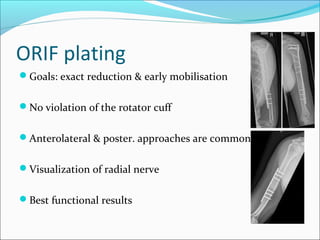
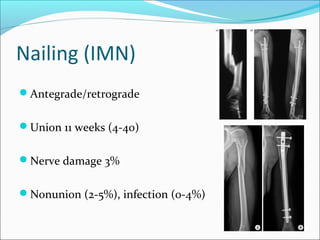
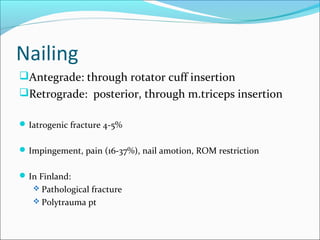
3) For surgery, plating provides the best visualization and stability but risks radial nerve injury. Intramedullary nailing risks impingement issues but is preferred for fractures with soft tissue injury. Minimally invasive plate osteosynthesis balances risks between methods.