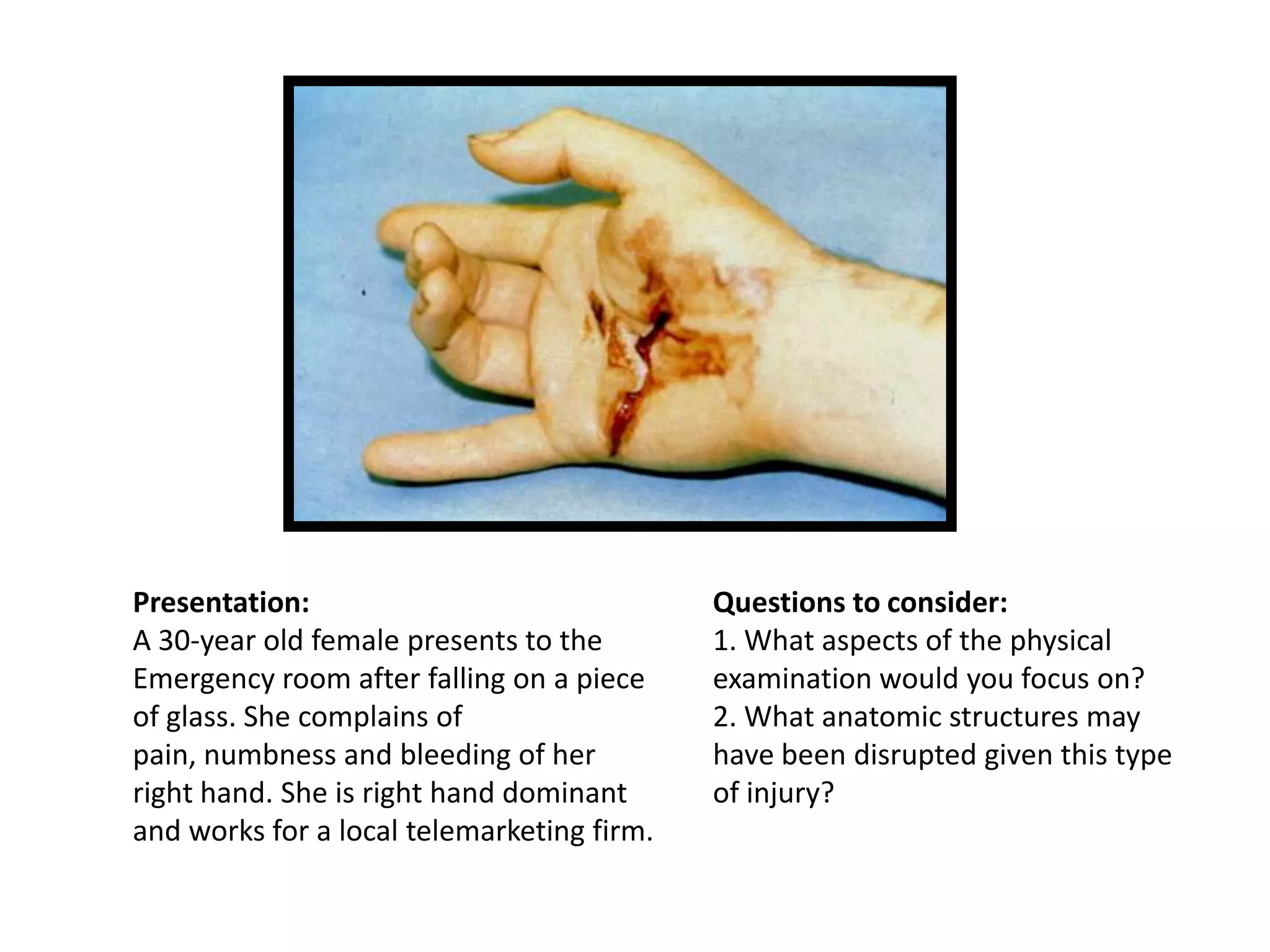
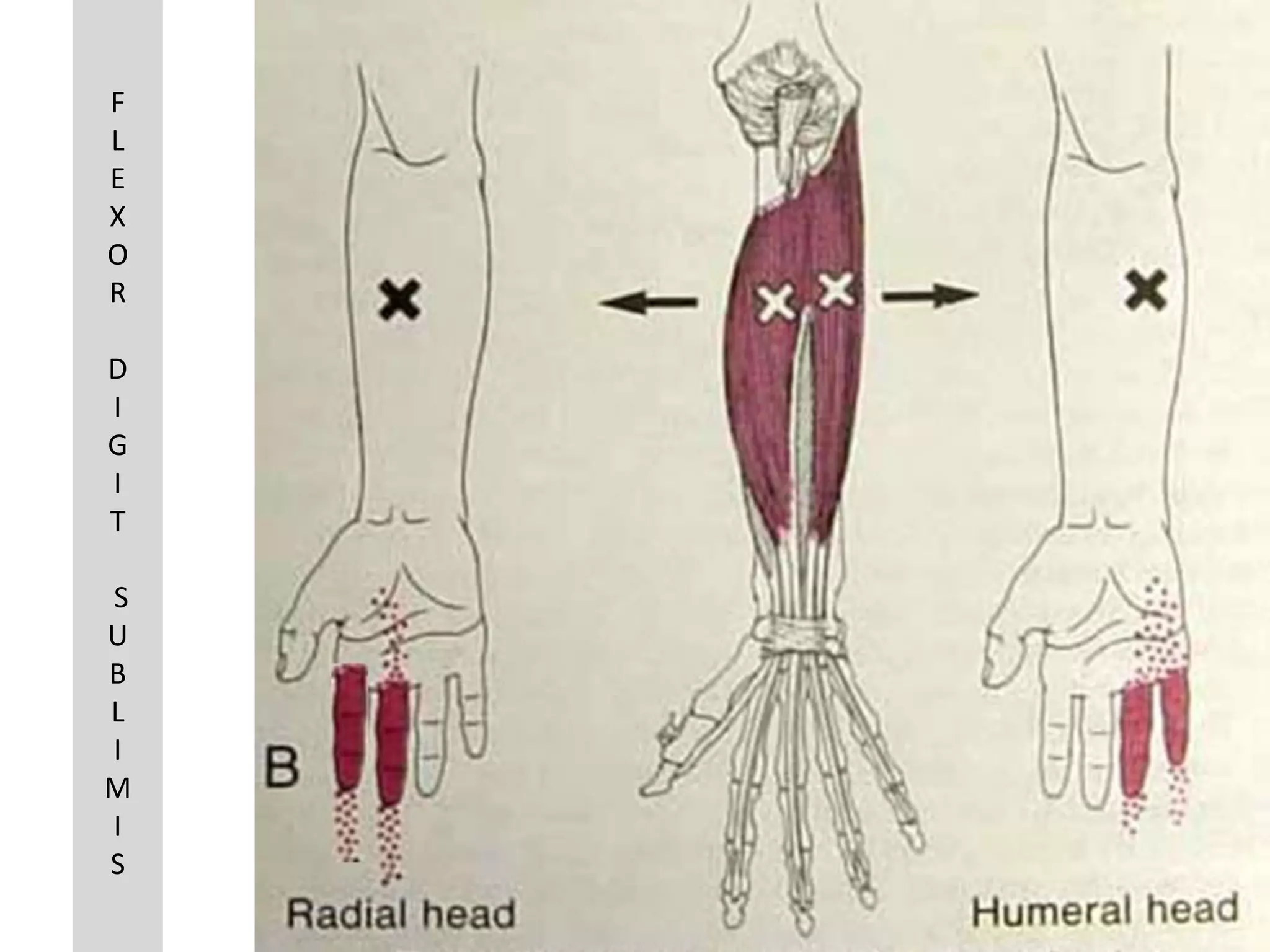
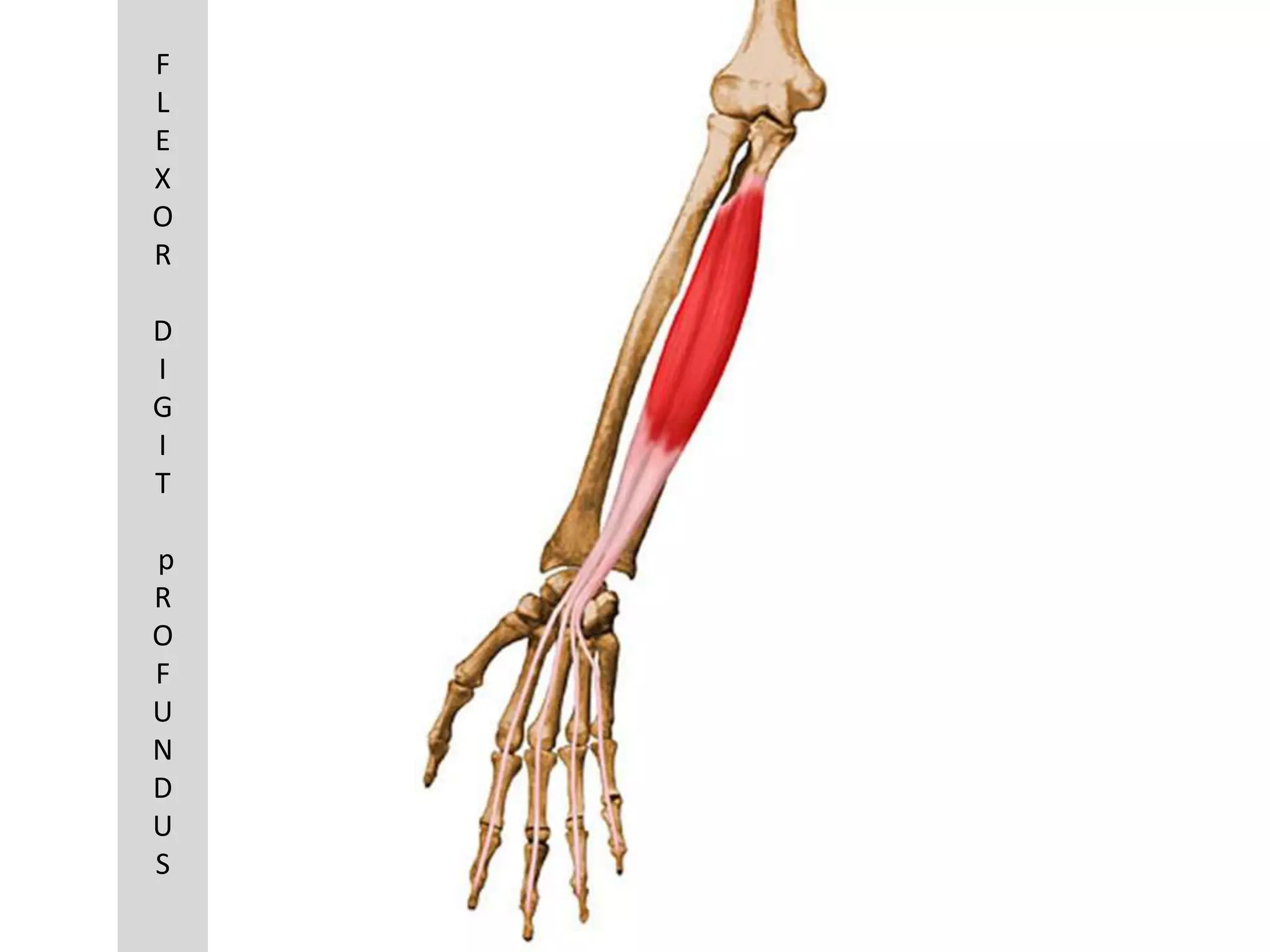
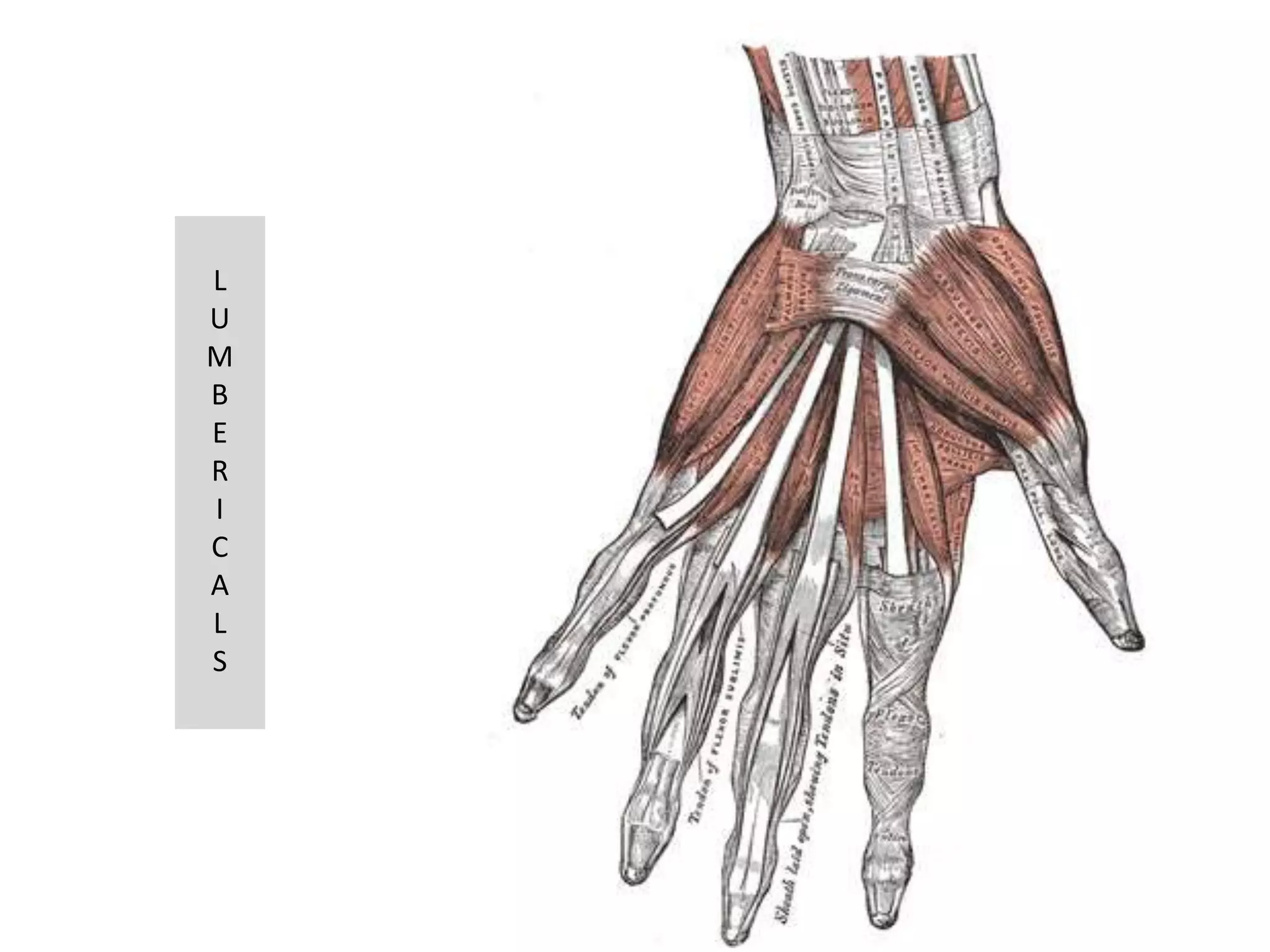
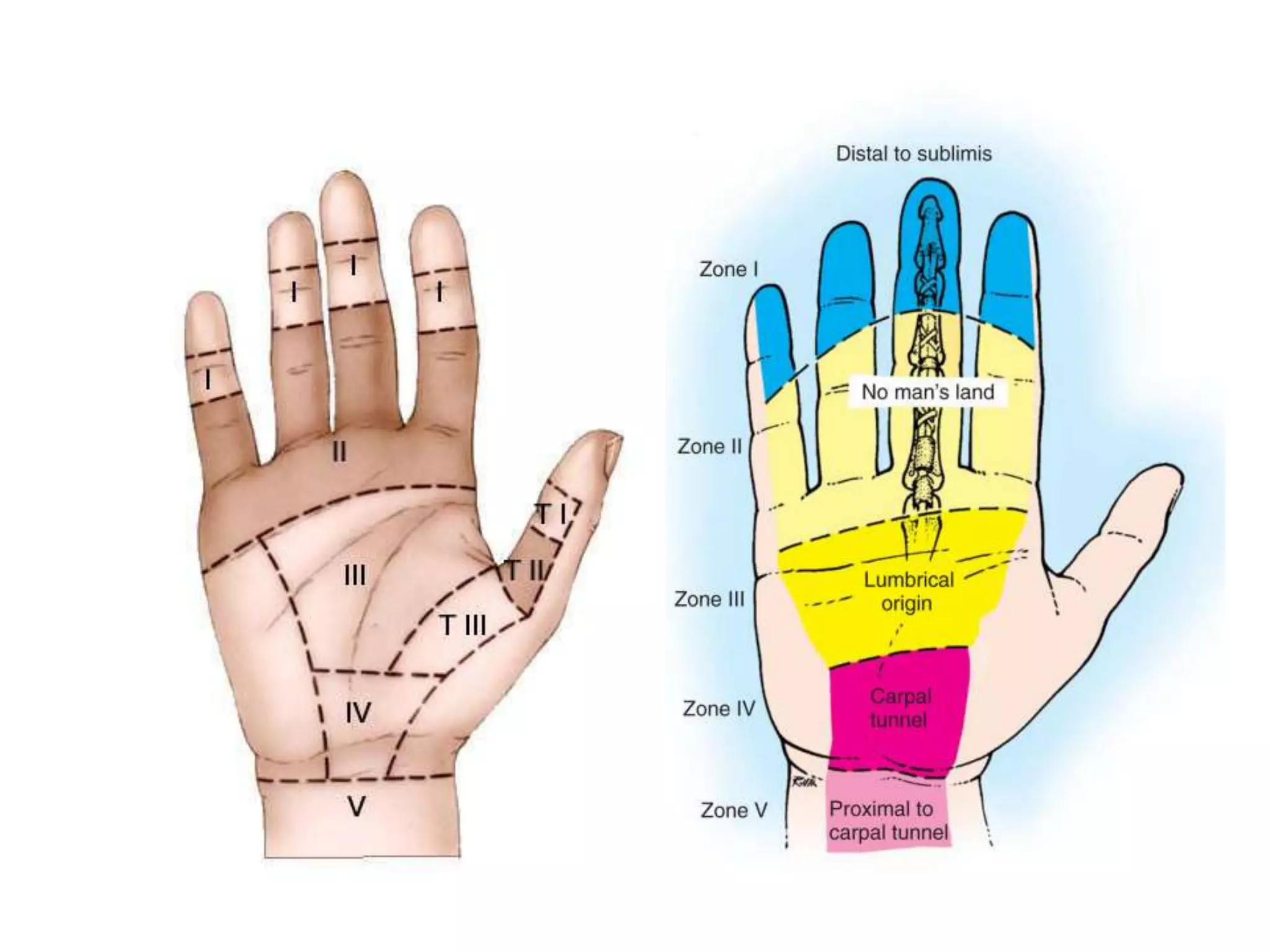
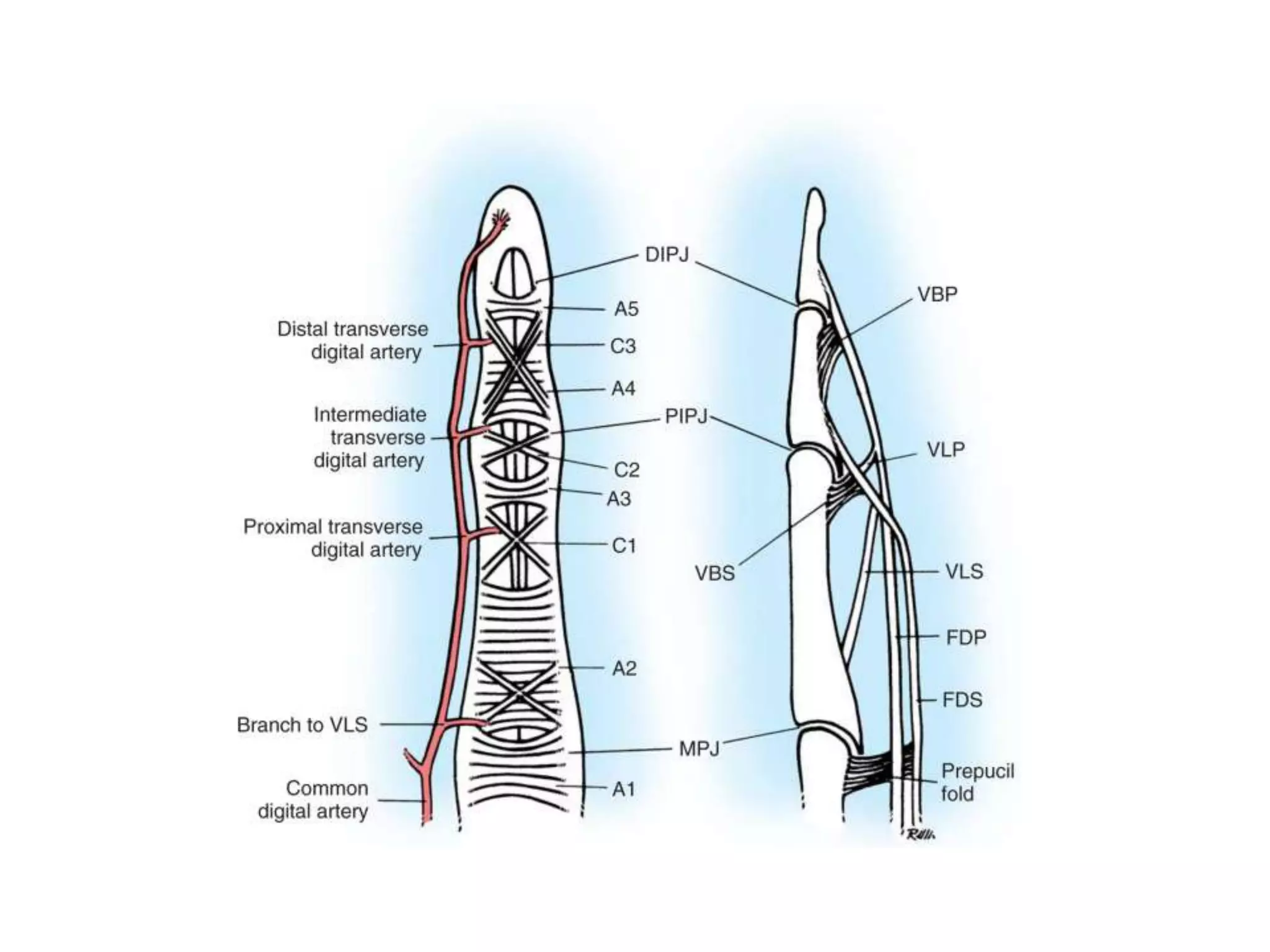
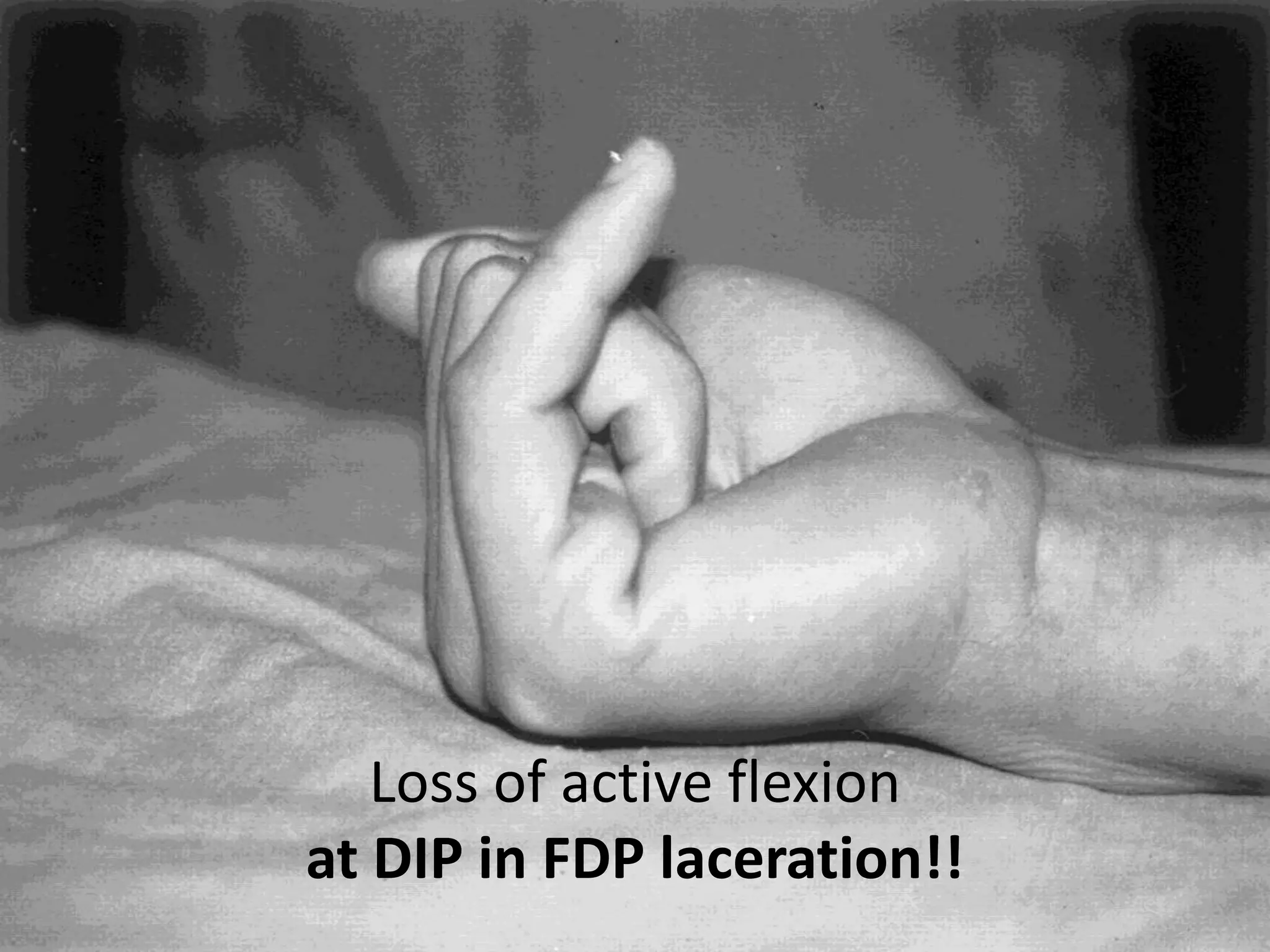
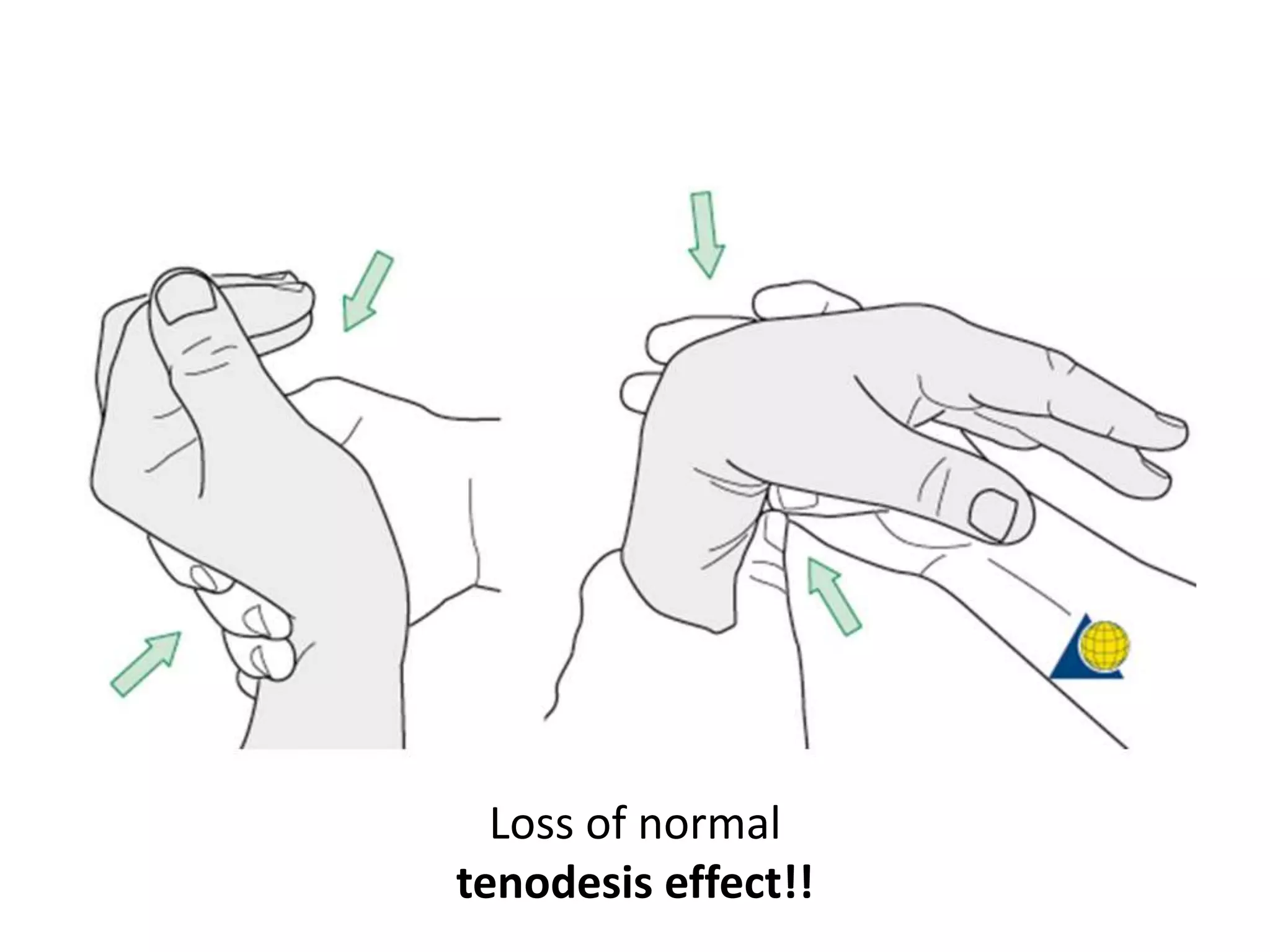
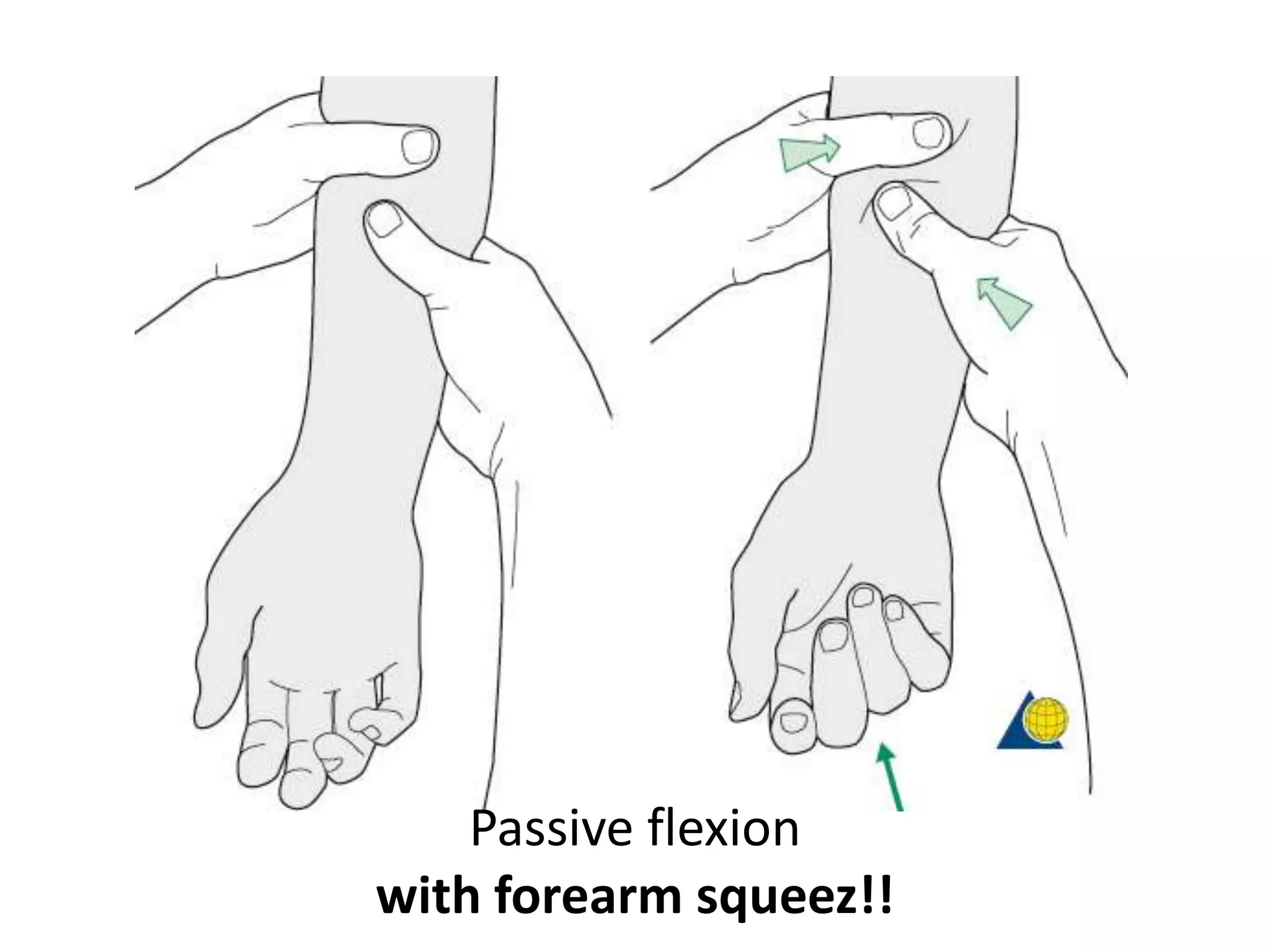
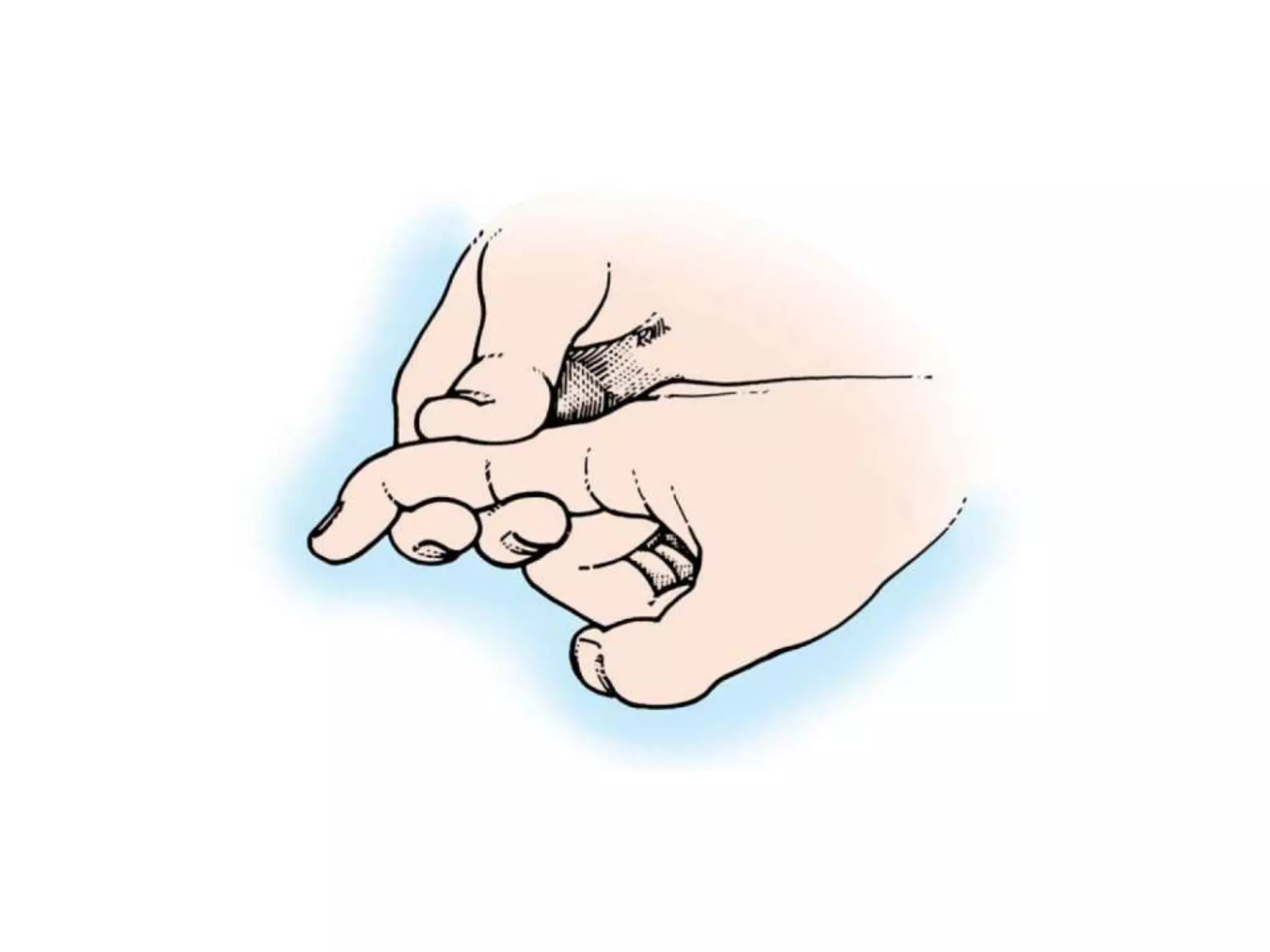
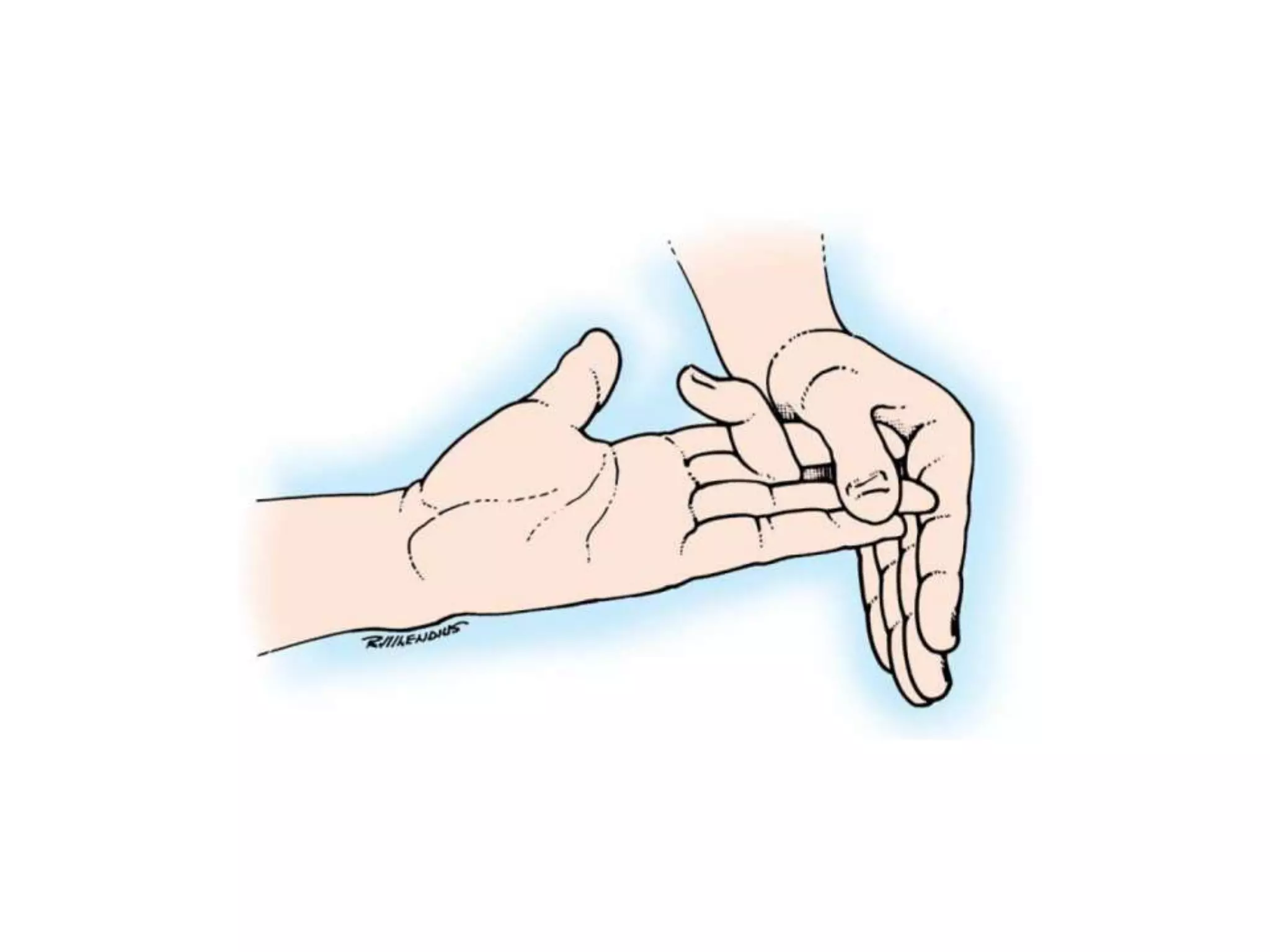
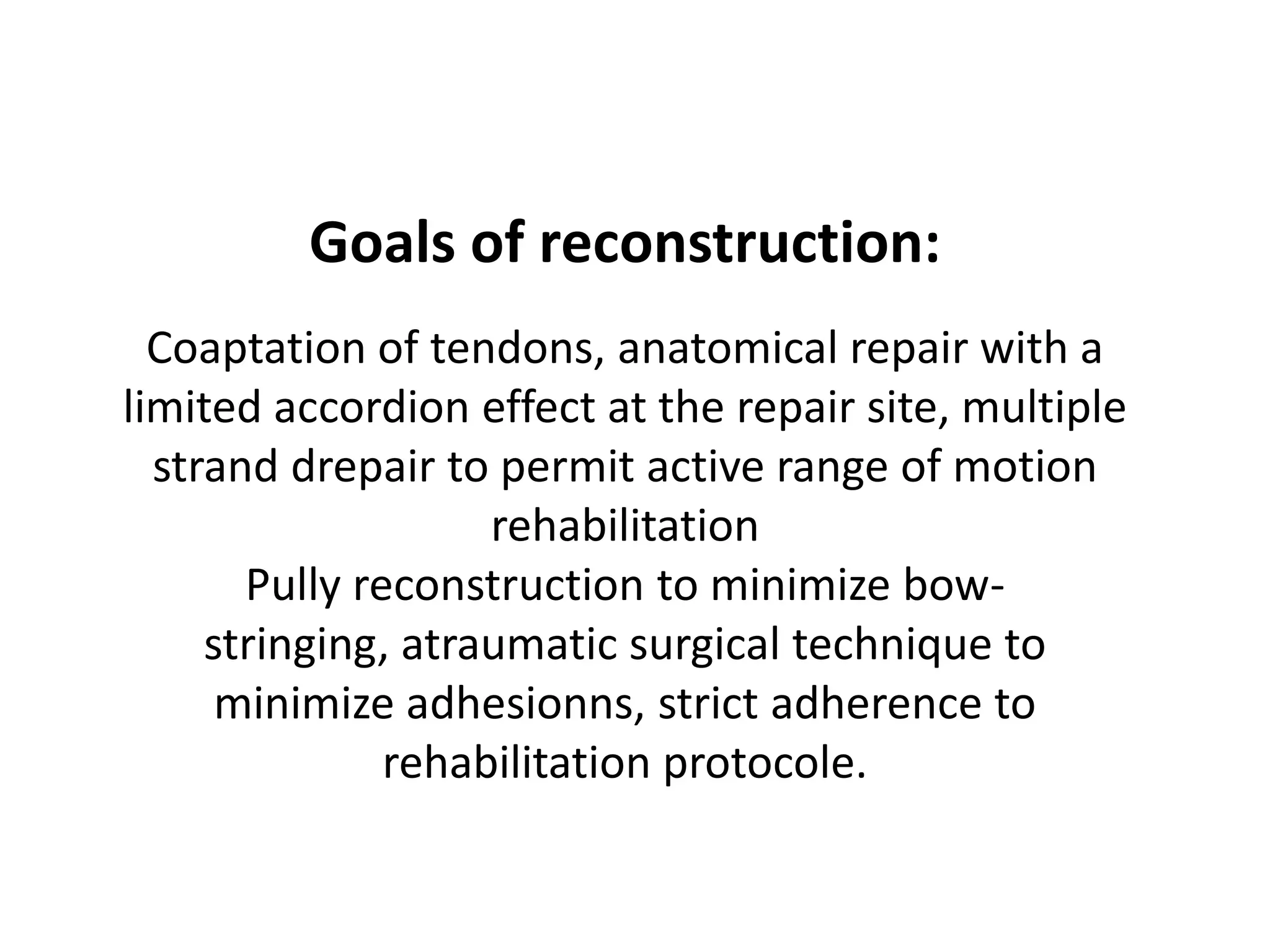
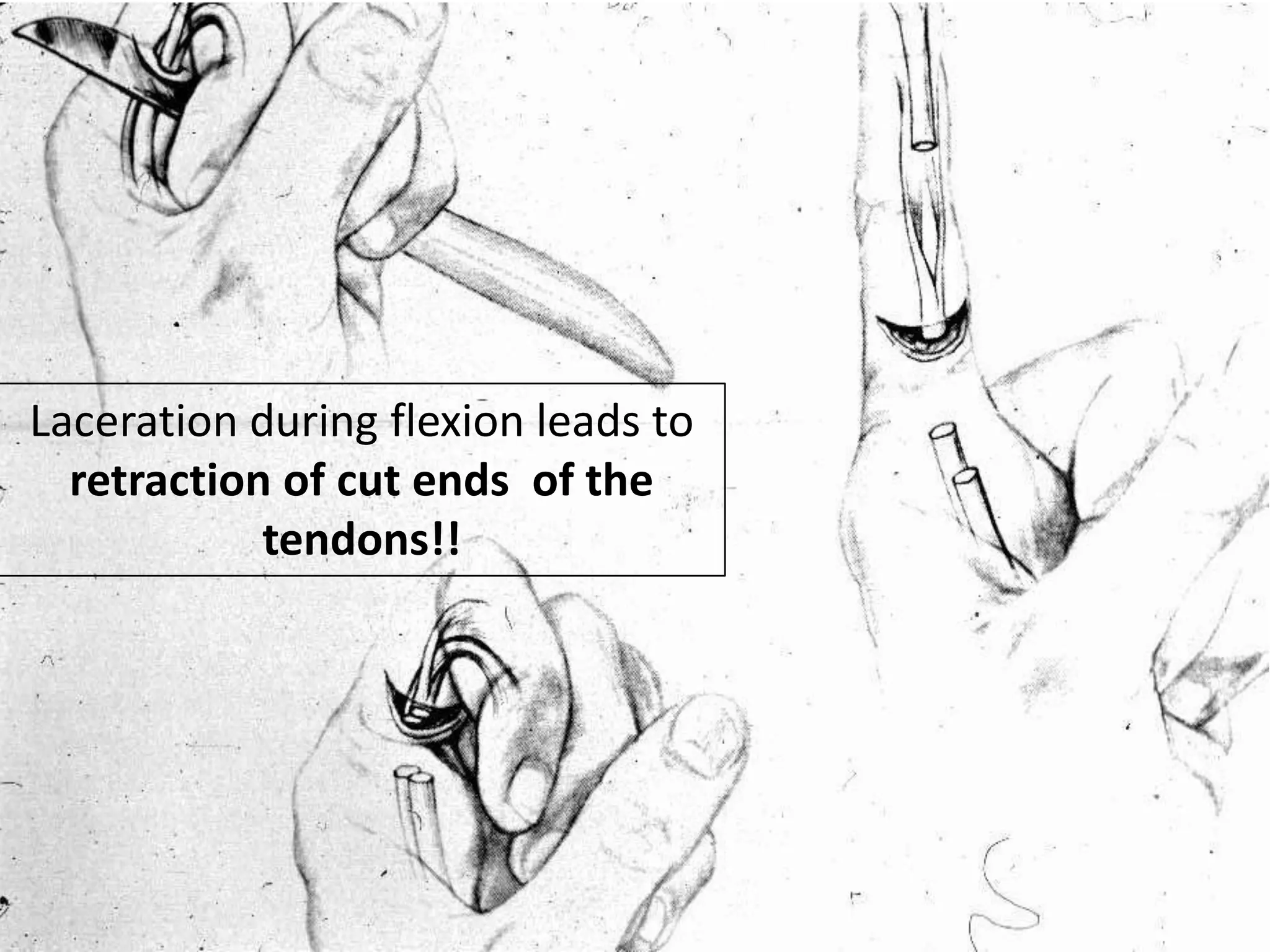
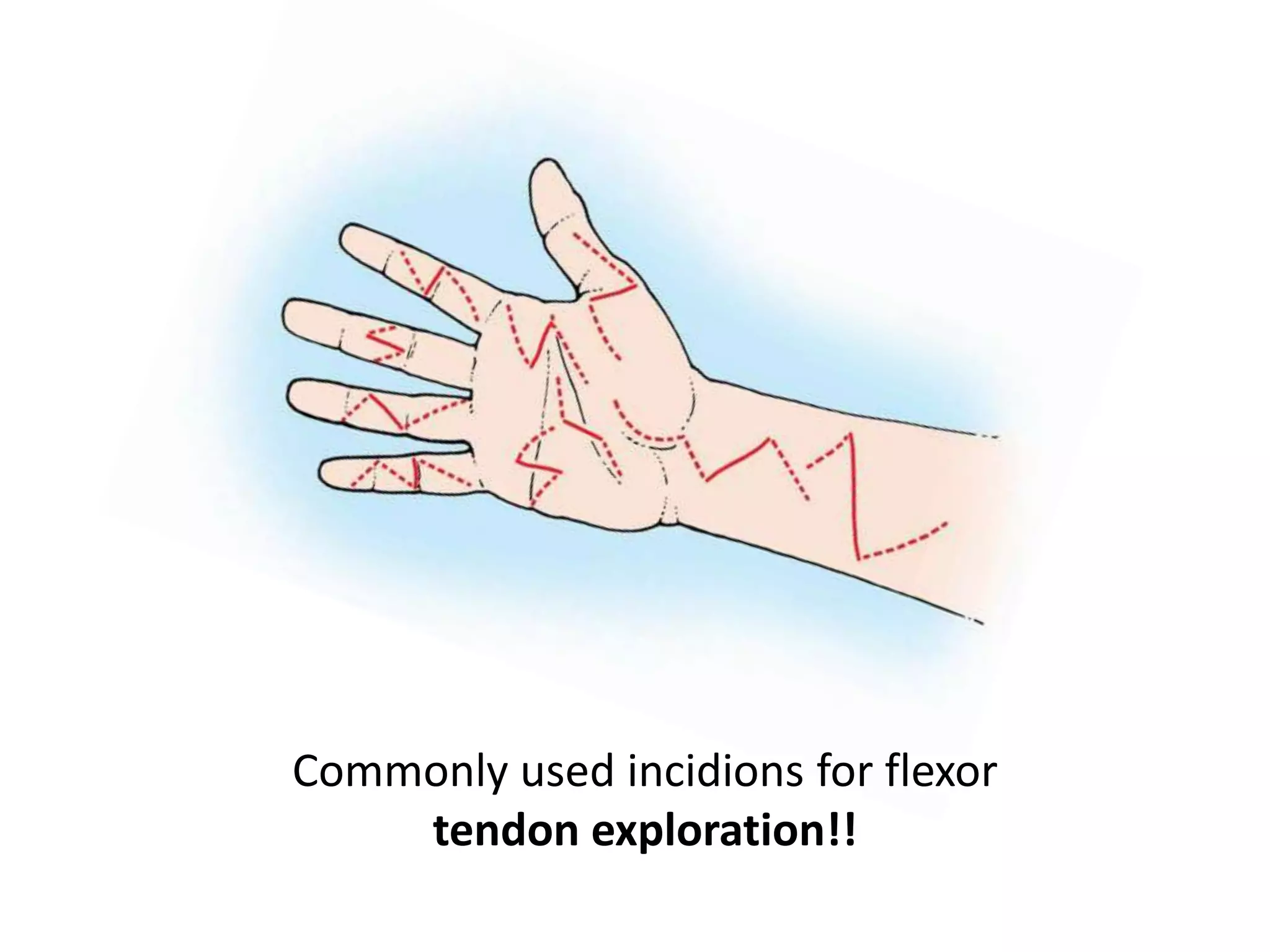
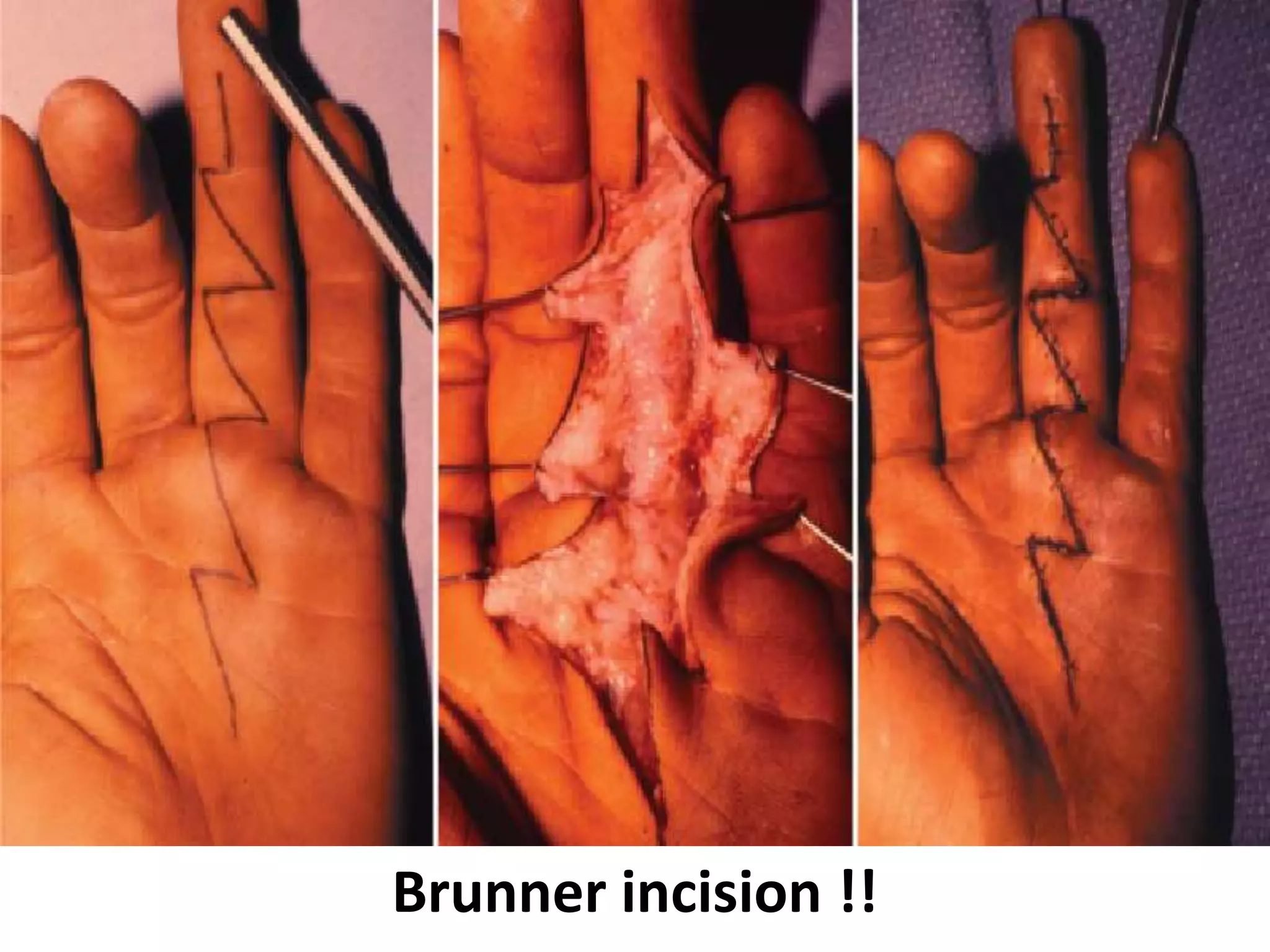
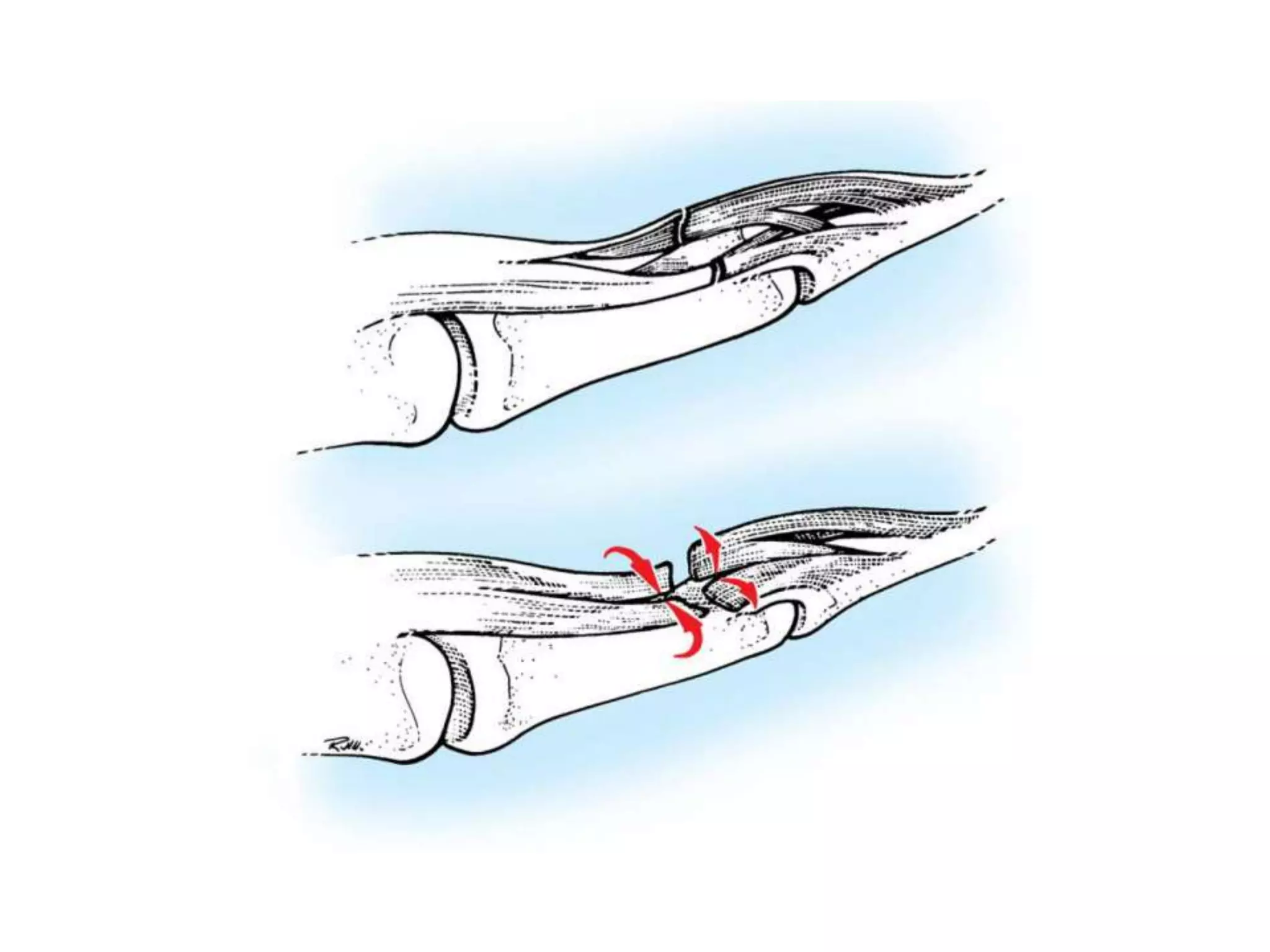
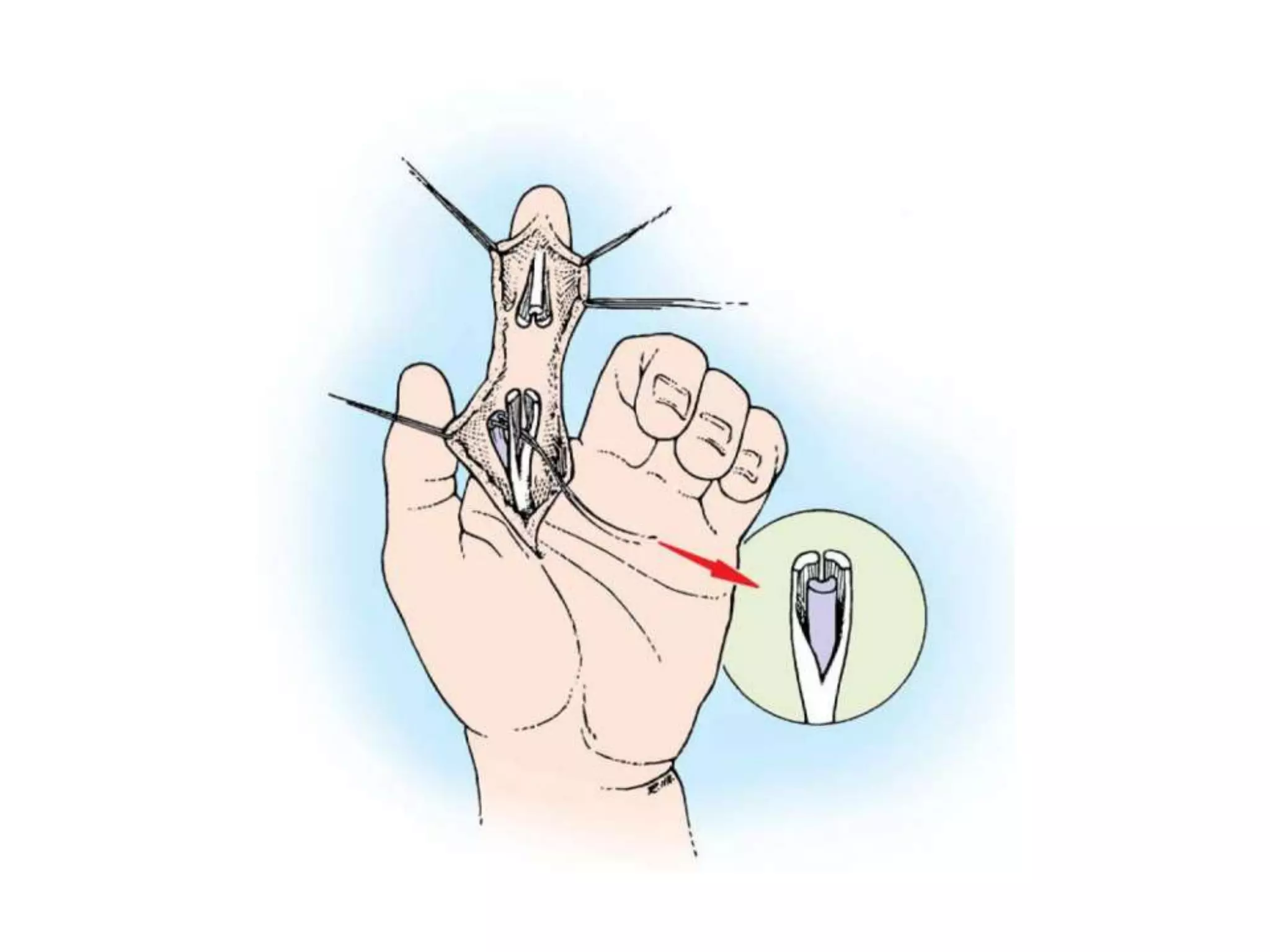
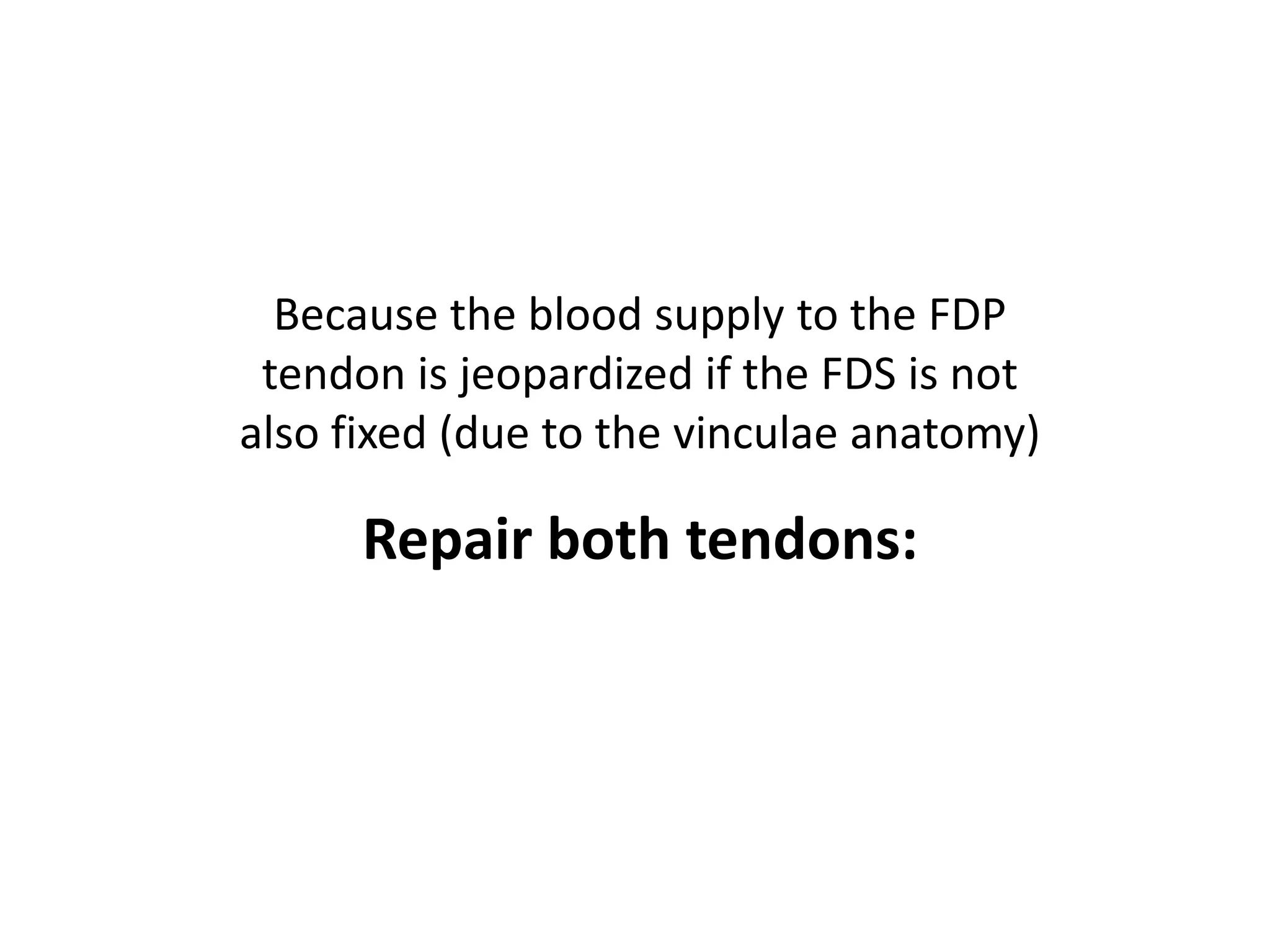
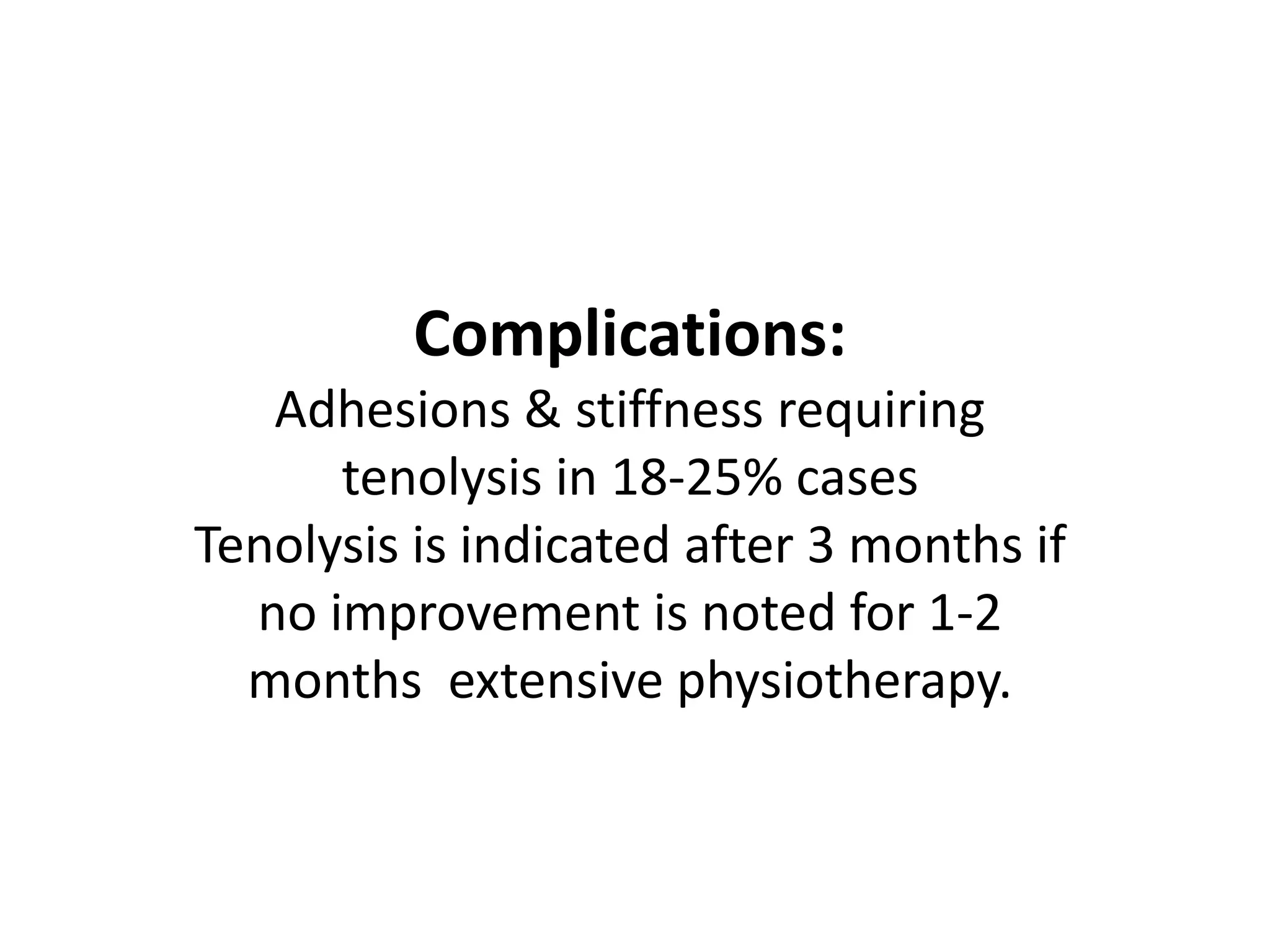
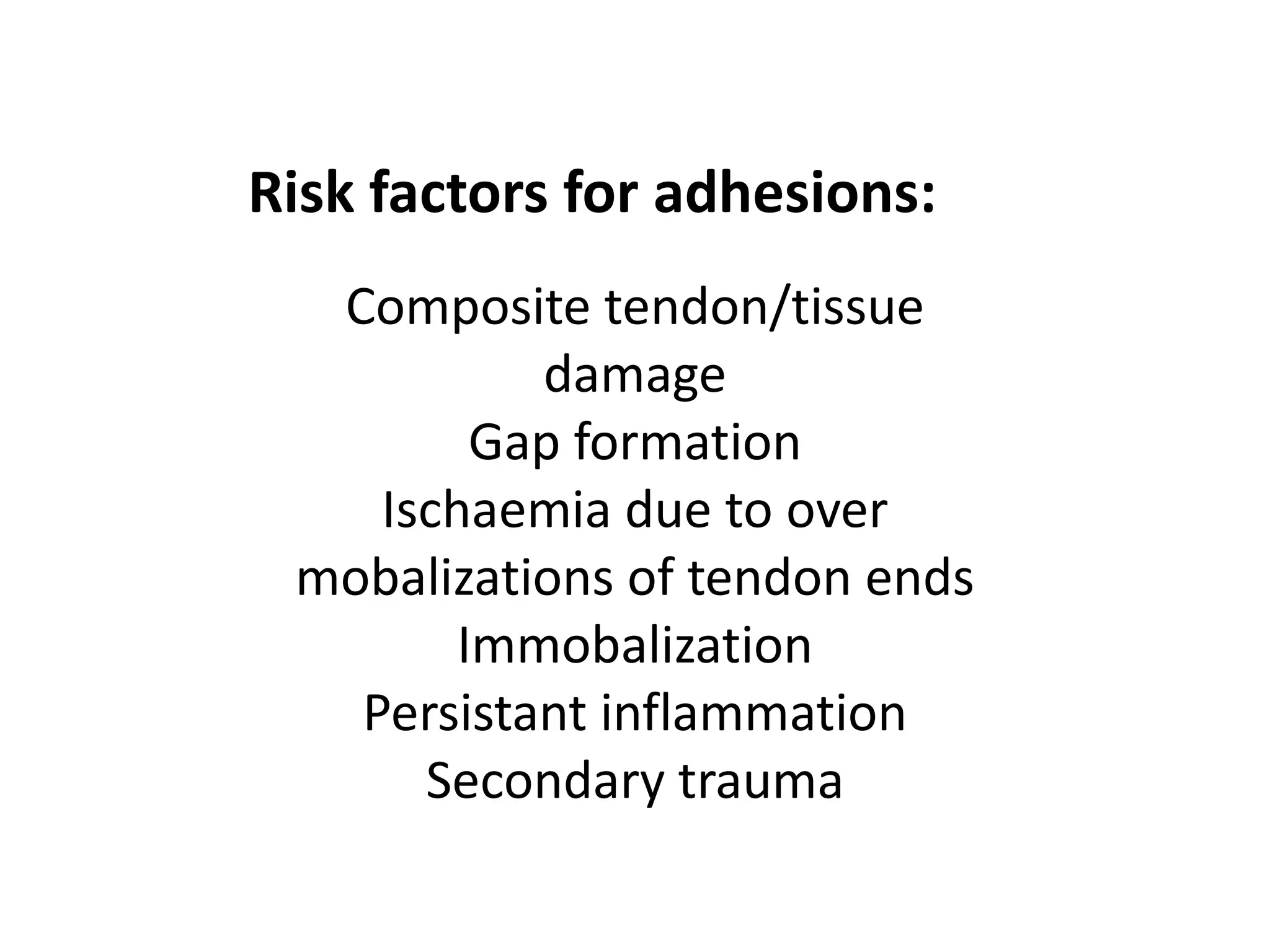
A 30-year old female presented to the emergency room with a laceration and bleeding in her right hand after falling on glass. She was right hand dominant and worked in telemarketing. Physical examination would focus on the extent of the laceration and potential injury to flexor tendons and nerves. Flexor tendon injuries can lead to loss of finger flexion and grip strength if not repaired properly. The goals of reconstruction are to anatomically repair the tendons with limited motion restrictions and adhere to post-operative rehabilitation to regain function and prevent complications like adhesions.