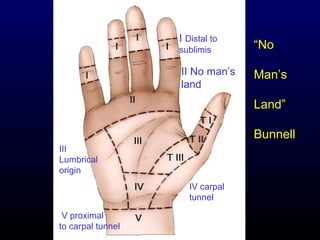
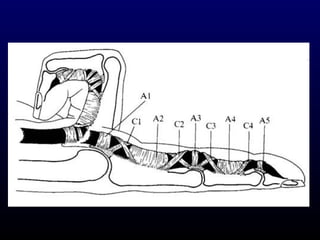
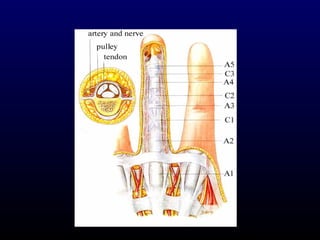
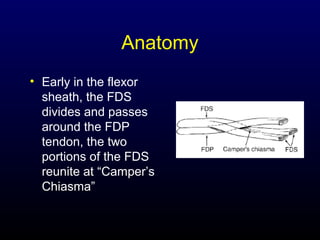
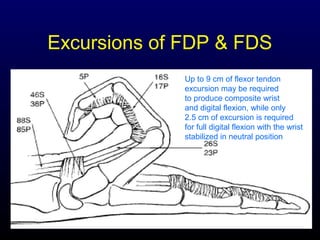
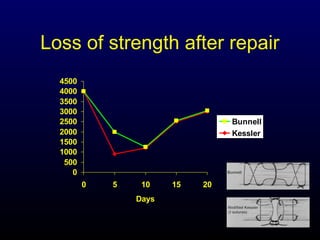
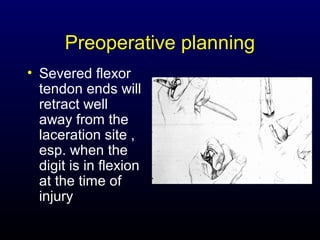
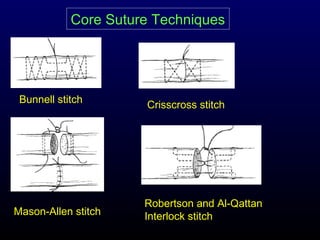
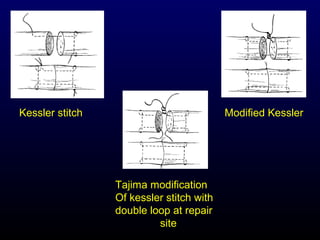
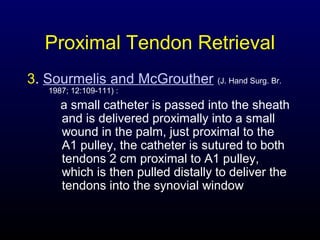
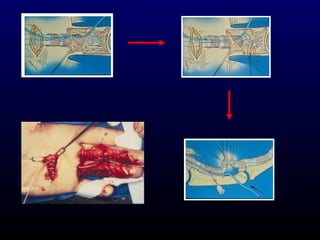
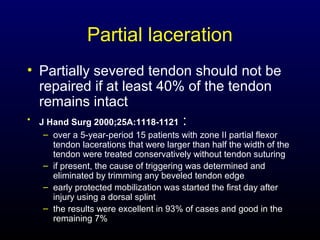
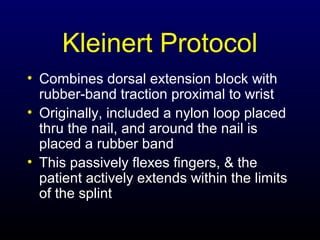
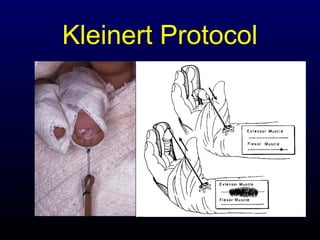
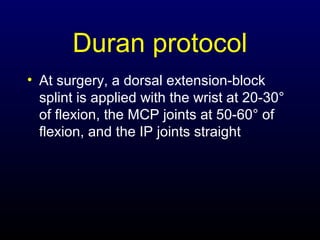
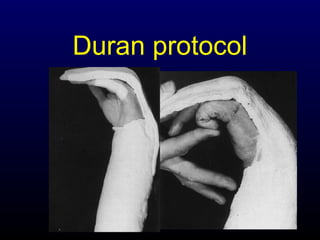
This document discusses flexor tendon injuries, including anatomy, healing, diagnosis, repair techniques, and postoperative rehabilitation. It describes the five zones of the hand where flexor tendon injuries can occur and techniques for primary repair or tendon advancement depending on the zone and extent of the injury. Various suture methods and postoperative protocols like Kleinert and Duran are presented. Complications of repairs like adhesion formation and joint contracture are also reviewed.