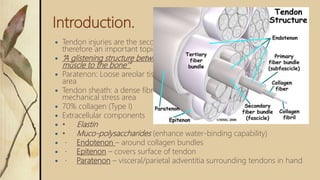
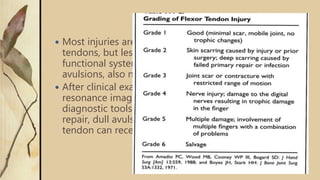
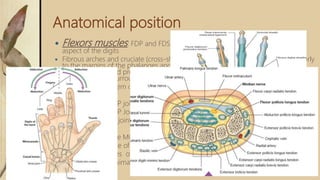
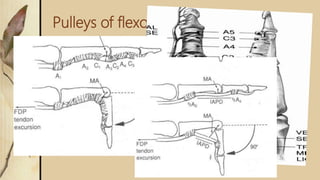
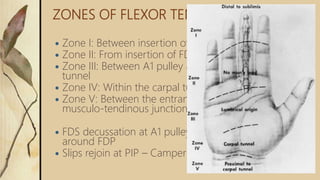
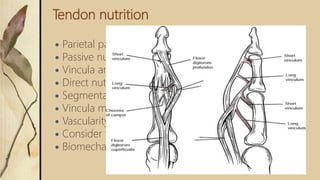
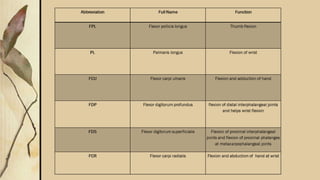
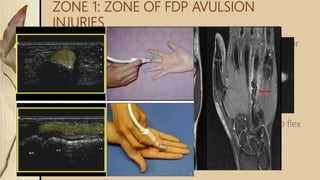
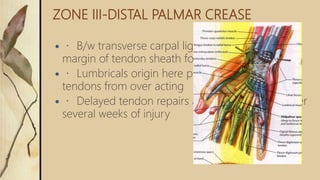
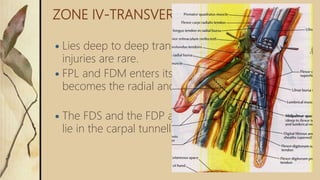
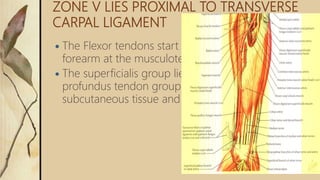
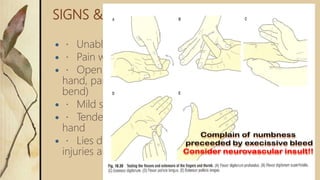
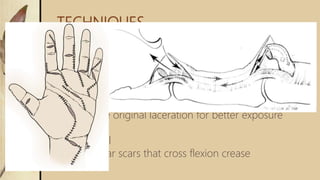
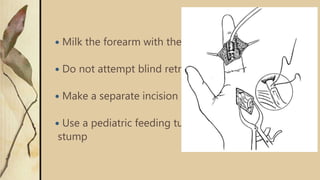
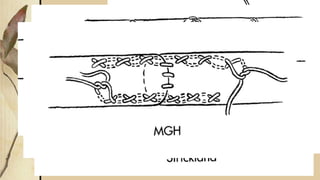
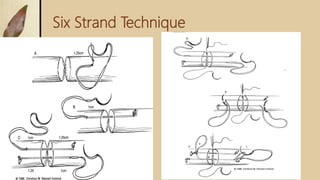
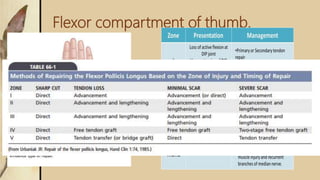
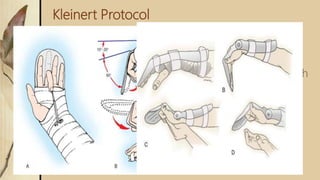
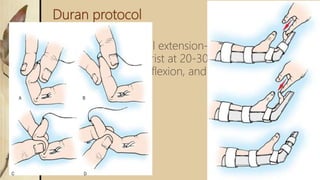
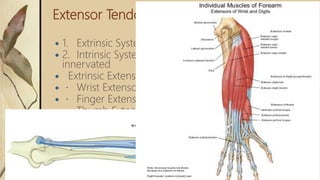
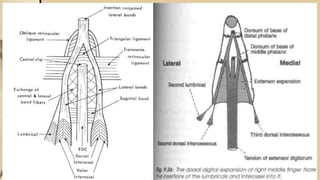
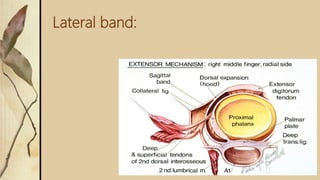
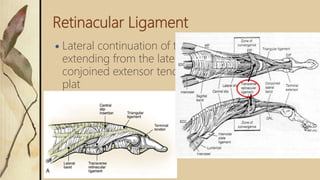
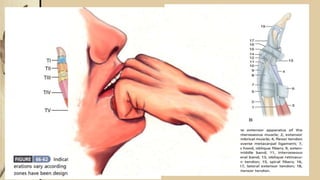
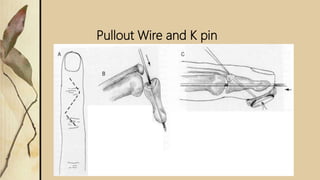
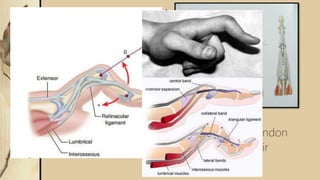
This document summarizes a seminar on flexor and extensor tendon injuries of the hand. The seminar was chaired by Prof. Dr. Kiran Kalaiah and presented by Dr. Yashavardhan.T.M. It provided an overview of tendon anatomy, classification of tendon injuries by zone, surgical techniques for repair, and postoperative rehabilitation protocols. Key points included the pulley system that guides tendon movement, zones of injury from I to V, and techniques like the six strand repair that aim to minimize complications like adhesion formation.