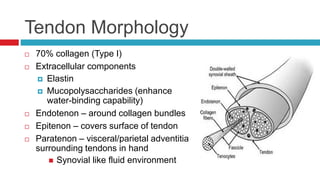
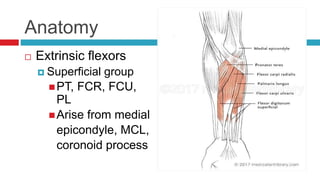
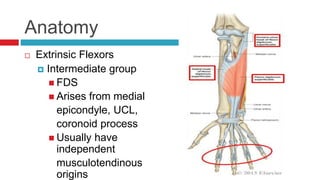
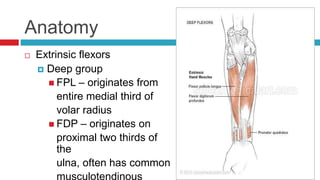
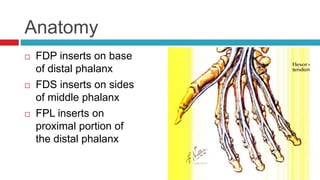
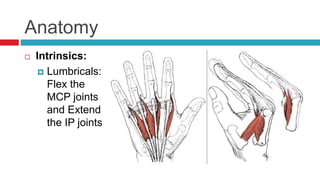
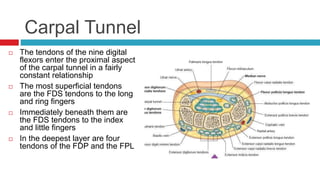
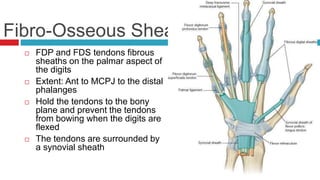
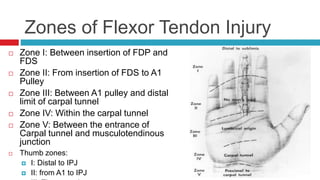
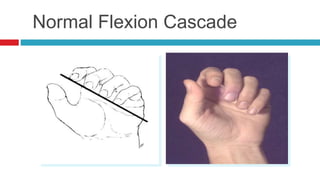
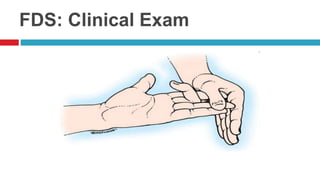
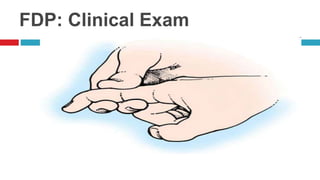
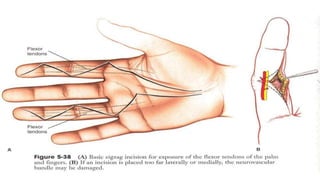
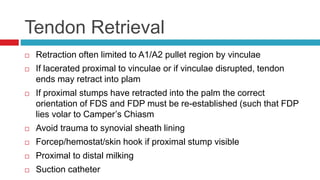
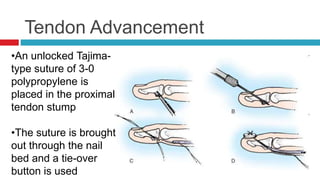
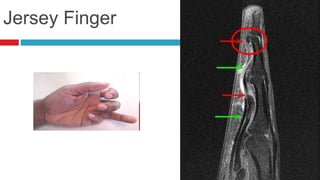
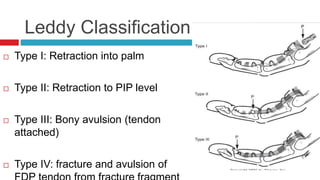
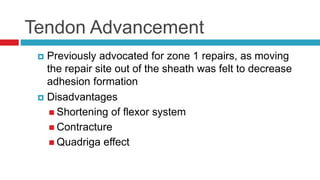
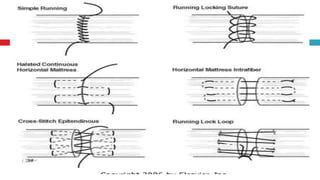
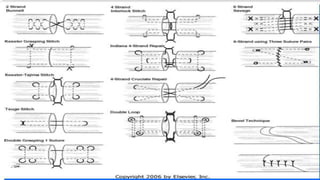
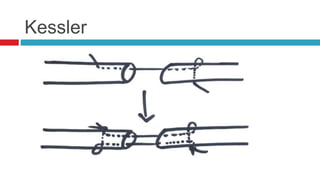
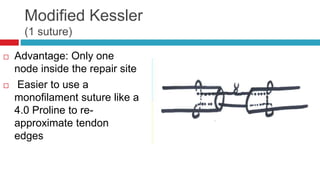
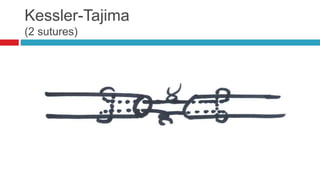
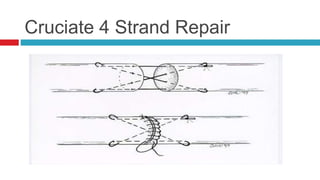
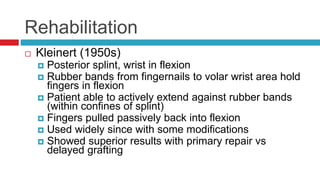
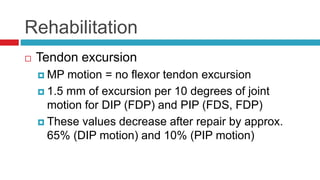
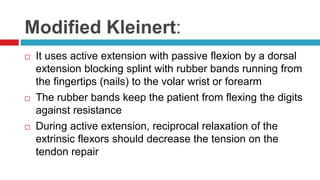
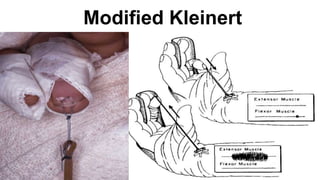
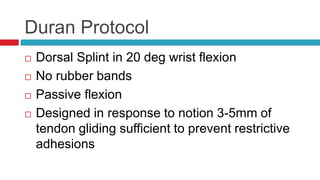
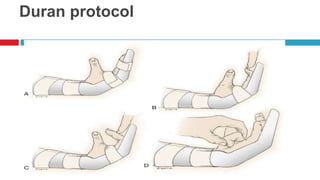
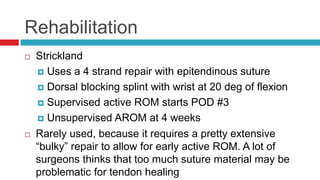
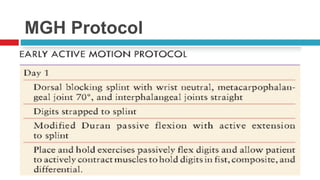
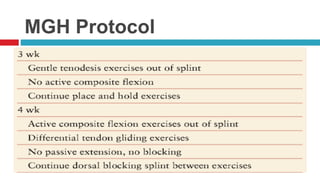
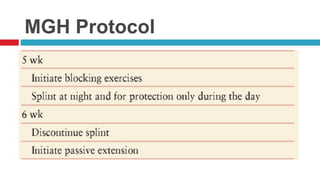
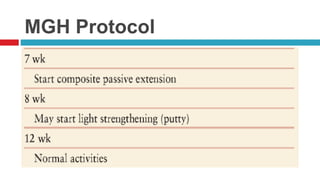
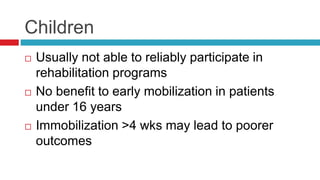
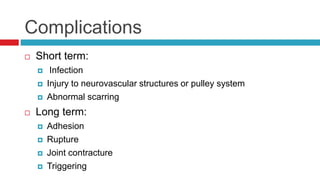
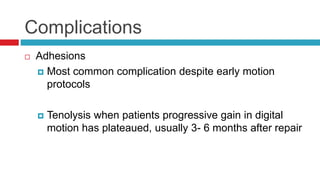
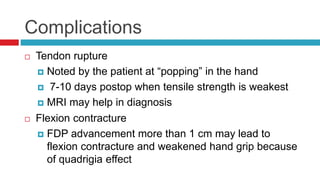
This document discusses flexor tendon injuries and their treatment. It begins with an overview of flexor tendon anatomy, morphology, zones of injury, and the challenges of repair. It then describes techniques for clinical evaluation, including testing of the flexor digitorum profundus and superficialis tendons. Principles of flexor tendon repair are outlined, including approaches for zone 1 and zone 2 injuries. Core suture techniques like the Kessler and Tajima methods are explained. Post-repair management considers risks of adhesion formation and importance of early motion.