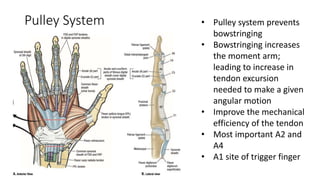
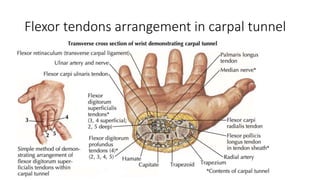
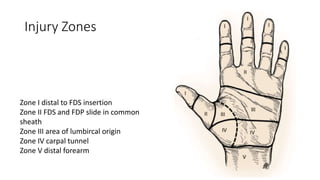
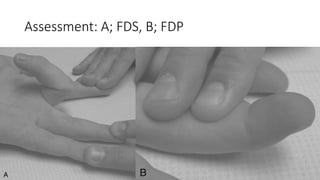
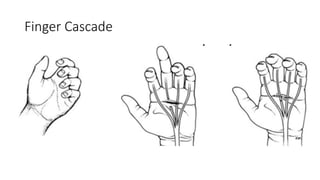
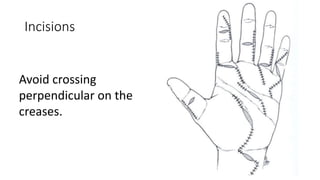
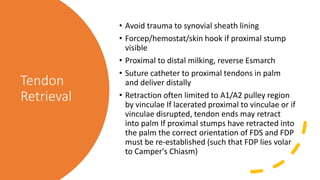
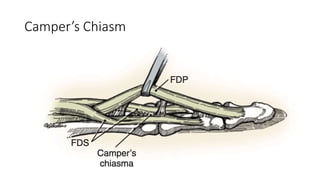
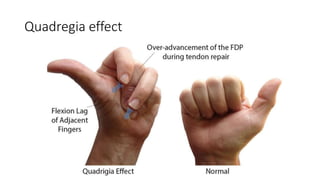
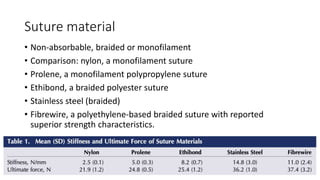
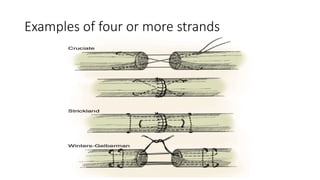
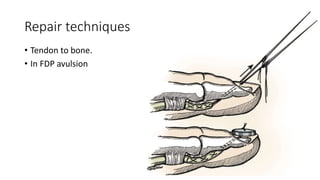
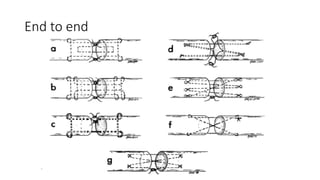
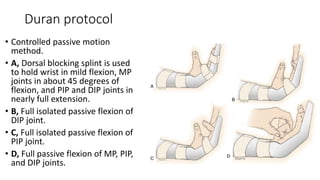
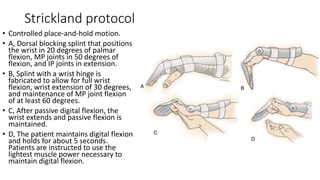
Flexor tendons injuries are complex and require careful management. There are 5 zones of injury along the finger. Pulleys help the tendons glide efficiently. The biological healing is weak initially. Assessment involves identifying the injured flexor digitorum profundus and superficialis tendons. Various repair techniques aim to provide strength for early motion while minimizing bulk and adhesions. Post-operative rehabilitation protocols like Duran and Strickland use controlled motion to promote longitudinal scar formation and intrinsic healing over extrinsic healing.