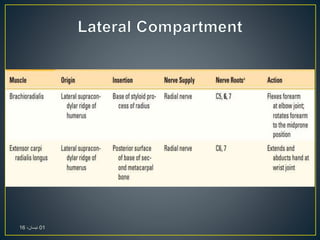
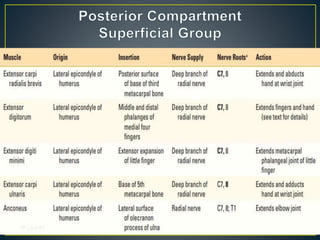
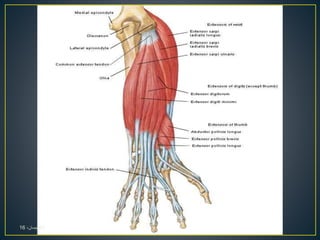
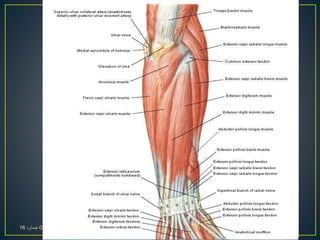
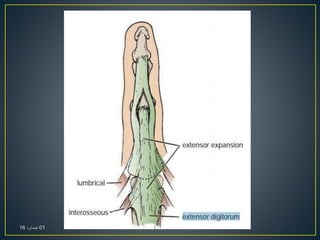
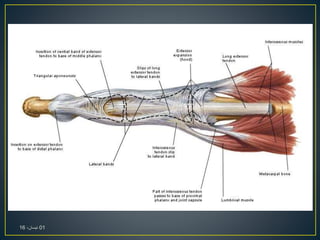
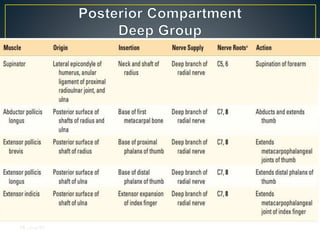
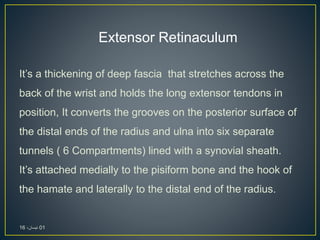
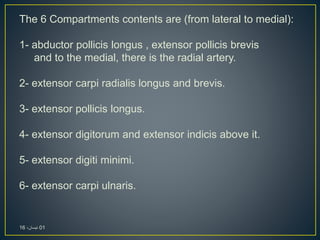
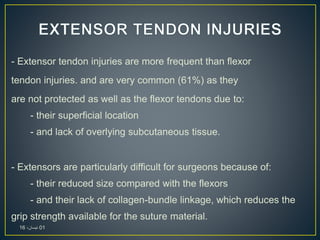
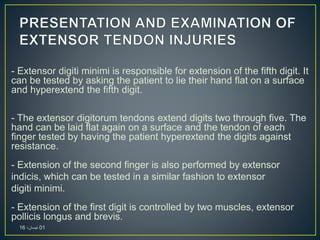
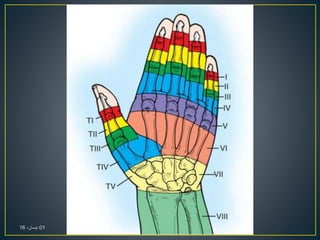
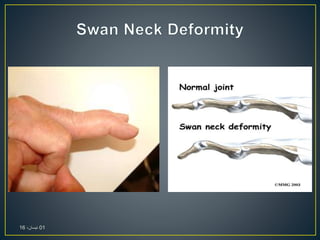
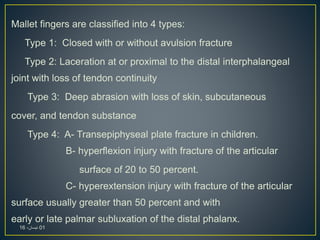
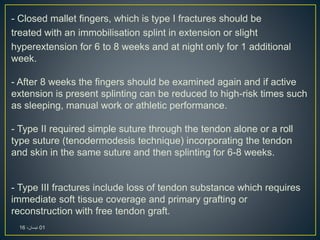
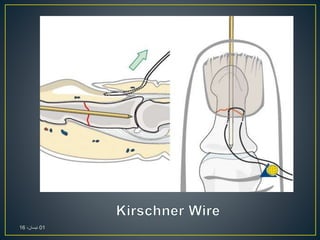
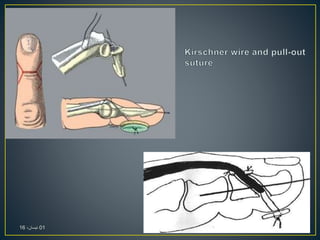
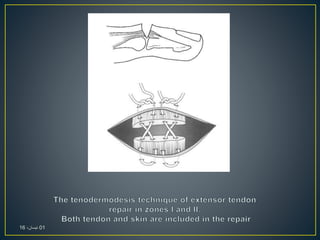
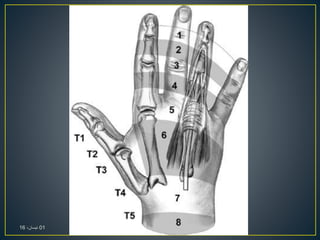
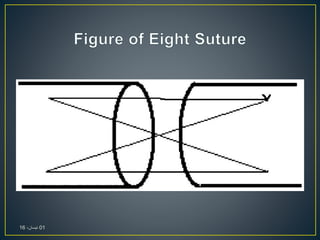
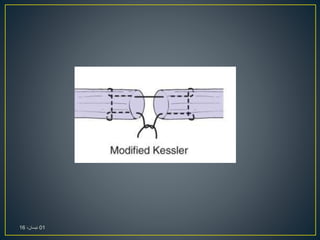
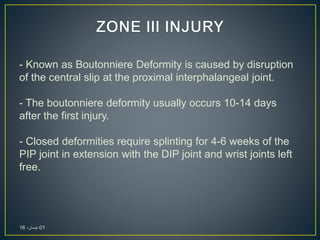
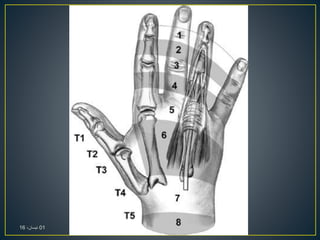
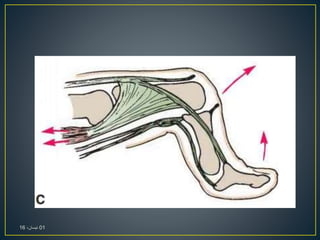
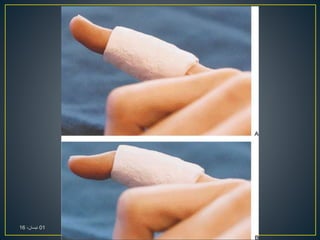
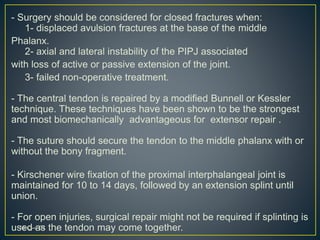
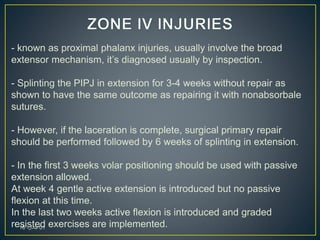
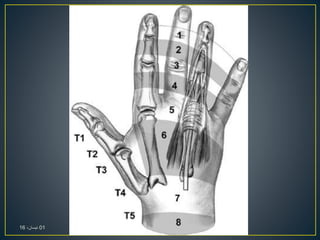
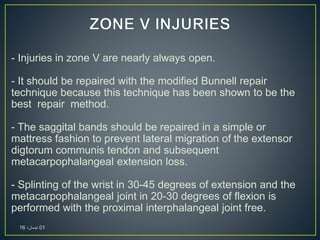
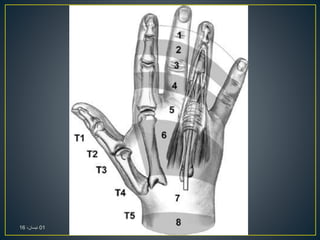
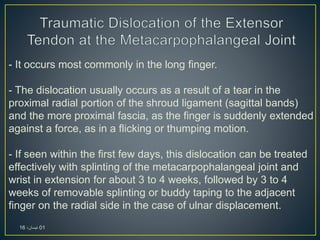
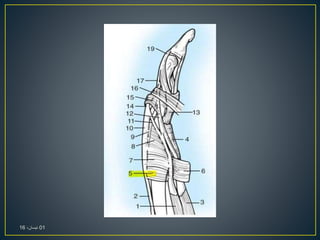
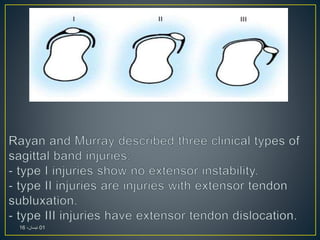
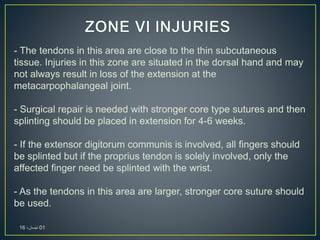
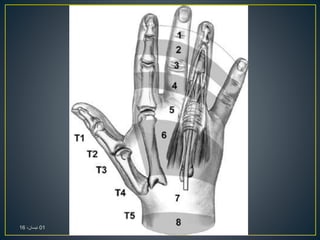
The document provides an overview of the anatomy and function of the forearm's extensor tendons, detailing their compartments, common injuries, and specific clinical tests for thumb and finger extension. It discusses the types of extensor tendon injuries, classifications, surgical repair techniques, and rehabilitation protocols for optimal recovery. Key complications and treatment methodologies for conditions like mallet finger and boutonniere deformity are also outlined.