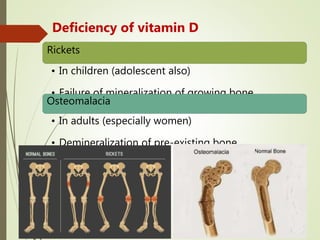
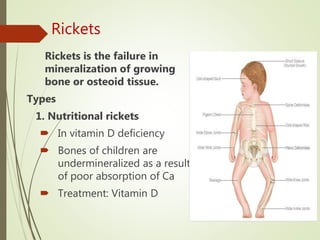
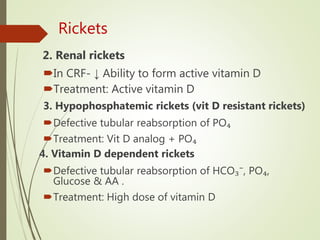
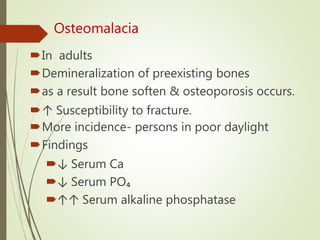
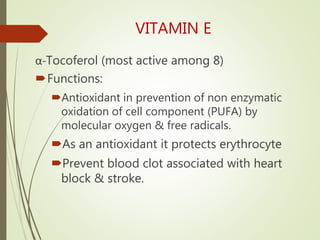
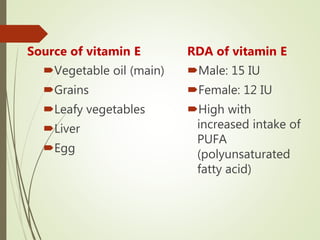
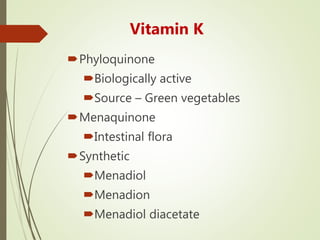
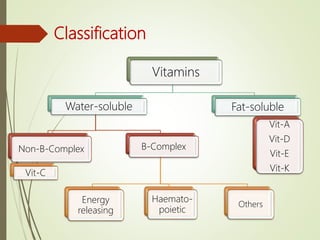
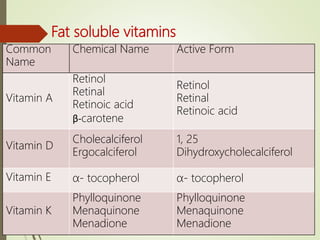
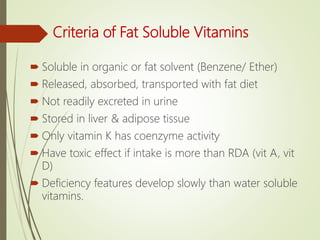
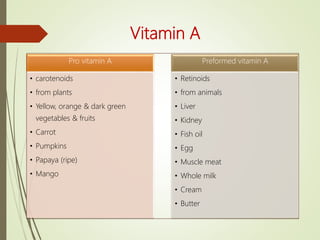
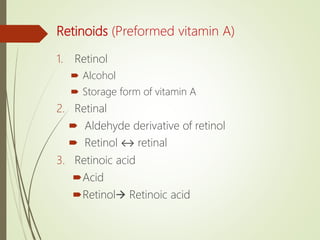
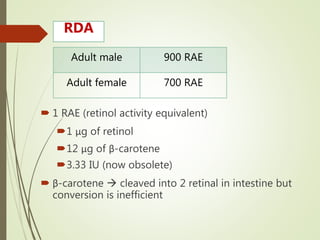
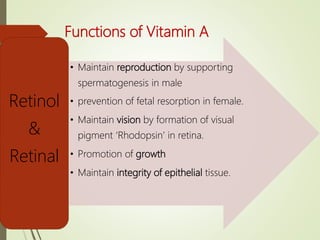
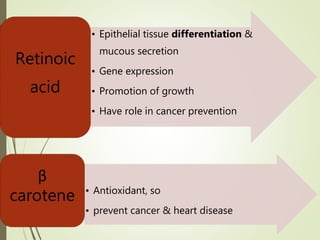
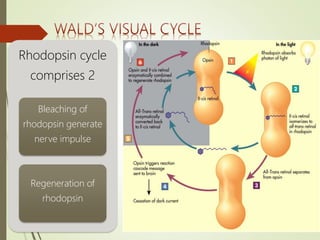
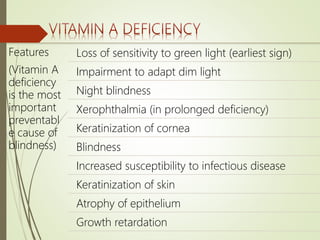
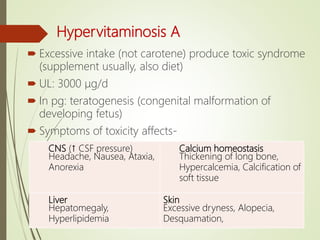
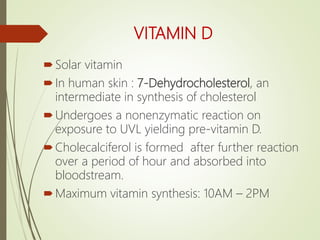
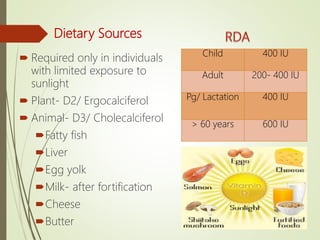
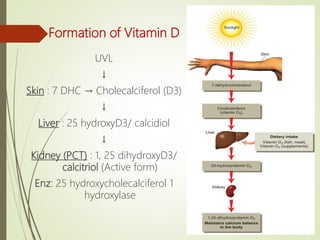
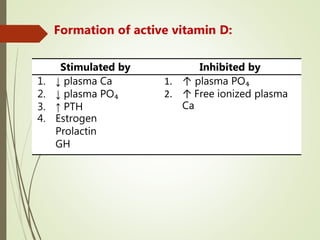
This document discusses fat-soluble vitamins, including their classifications, functions, dietary sources, deficiency signs, and toxicity. Specifically, it details vitamins A, D, E, and K, highlighting their biochemical roles, importance for health, and consequences of deficiency or overdose. It emphasizes the distinct storage and absorption characteristics of fat-soluble vitamins compared to water-soluble vitamins.
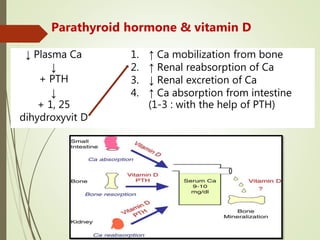
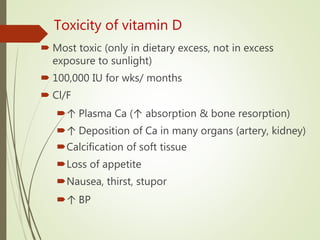
![Vitamin D & Ca Homeostasis
Condition GIT Bone Kidney
↓ [Ca]
↑ Ca
absorption
↑ mobilization Active vit D formation
↑ [Ca]
↓ Ca
absorption
[+] Calcitonin
[-] Ca mobilization
↑ excretion (calcitonin)
↓ reabsorption (PTH)
Inactive vit D formation
↓ vit D
No
absorption
[+] Ca mobilization
(PTH)
↓ excretion (PTH)
↑ reabsorption (PTH)
↑ vit D ↑ absorption
↑↑ mobilization
↑ accumulation
↑ excretion (calcitonin)
Inactive vit D formation](https://image.slidesharecdn.com/fatsolublevitamin-200411051152/85/Fat-soluble-vitamins-20-320.jpg)