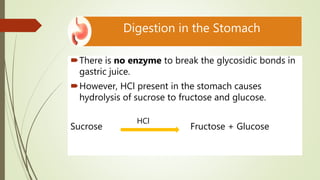
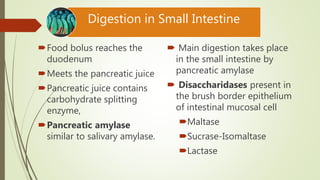
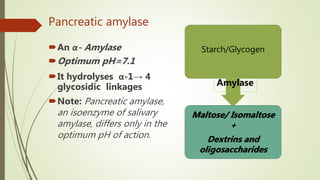
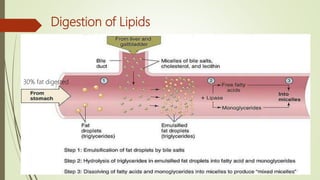
The document provides a comprehensive overview of digestion and absorption processes, including the roles of digestive juices, enzymes, and hormones involved in breaking down carbohydrates, proteins, and lipids. It details the specific composition and functions of various digestive fluids such as saliva, gastric juice, pancreatic juice, and bile, as well as the mechanisms of nutrient absorption in the intestines. Key points include the importance of enzymatic activity and the physiological processes necessary for effective digestion and assimilation of nutrients into the body.

![Absorption of carbohydrates
Glucose transporter
1. Na+ dependent
transporter [SGLT]
2. Na+ independent
transporter [GLUT]](https://image.slidesharecdn.com/digestionabsorption2020-210210111329/85/Digestion-and-absorption-29-320.jpg)
![Lactose intolerance
Inability to digest lactose due to the deficiency of Lactase
enzyme.
Presents as abdominal cramps, distensions, diarrhea,
constipation, flatulence upon ingestion of milk or dairy
products
Undigested lactose in intestine is converted to CO2, H2, 2 &
3 carbon compounds [by bacteria]
CO2 & H2 causes distensions and flatulence
Lactose + 2C + 3C are osmotically active
Cause osmotic diarrhea or constipation because of
undigested bulk](https://image.slidesharecdn.com/digestionabsorption2020-210210111329/85/Digestion-and-absorption-30-320.jpg)
![Carbohydrate Lipid Protein
In diet Starch
Lactose
Sucrose
Cellulose
TAG (90%)
Cholesterol
Cholesterol ester
Phospholipids
Free fatty acid
Protein
Mouth [Salivary α-amylase]
Starch
Dextrins
Isomaltose
Maltose
Maltotriose
Lactose
Sucrose
Cellulose](https://image.slidesharecdn.com/digestionabsorption2020-210210111329/85/Digestion-and-absorption-42-320.jpg)
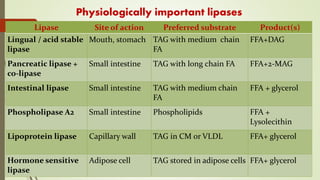
![Carbohydrate Lipid Protein
Stomach Low pH stop enzyme
action
[Lingual lipase]
[Gastric lipase]
TAG with short & medium
chain fatty acid
[HCl]+[Pepsin]
Denaturation
Polypeptides
Amino acids
Small
intestine
[Pancreatic α-amylase]
Isomaltose
Maltose
Maltotriose
Lactose
Sucrose
Cellulose
[Disaccharidase]
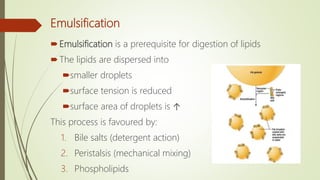
Emulsification
[Pancreatic lipase]
[Colipase]
[Cholesterol esterase]
[Phospholipase A2]
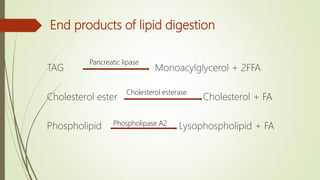
TAG
Cholesterol ester
Phospholipid
[Trypsin]
[Chymotrypsin]
[Elastase]
[Carboxypeptidase]
Oligopeptides
Amino acids
[Aminopeptidase]
[Di & tripeptidase]](https://image.slidesharecdn.com/digestionabsorption2020-210210111329/85/Digestion-and-absorption-43-320.jpg)
![Carbohydrate Lipid Protein
End
products
Glucose
Fructose
Galactose
Cellulose colon &
excreted
FFA
2-Monoacyl glycerol
Cholesterol
Lysophospholipid not
absorbed
Amino acids
Absorption Glucose
Galactose
[SGLT1]
↓
Enterocyte
[GLUT2]
↓
Portal blood
Fructose
[GLUT5]
↓
Enterocyte
[GLUT2]
↓
Portal
blood
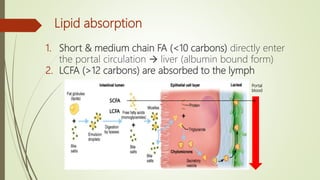
SCFA(12)
↓
Portal blood
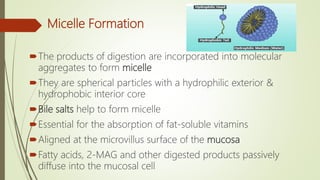
LCFA
Micelle(+bile salt
+ FSV)
↓
enterocyte
Chylomicron
↓
Lymphatics
↓
Blood
Seven different
active transport
process](https://image.slidesharecdn.com/digestionabsorption2020-210210111329/85/Digestion-and-absorption-44-320.jpg)
