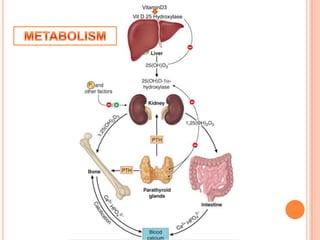
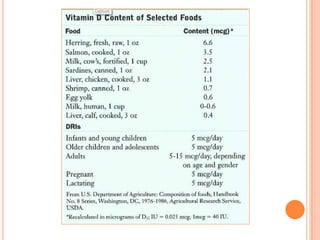
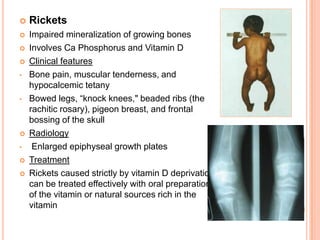
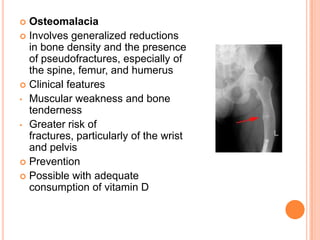
Vitamin D, also known as the sunshine vitamin, can be produced in the skin upon exposure to UVB light or obtained in the diet. It plays an important role in calcium and phosphorus homeostasis. Dietary requirements are minimal as the body can produce vitamin D3 in the skin, but certain groups like the elderly are at higher risk of deficiency. Deficiency can lead to rickets in children and osteomalacia in adults, characterized by soft, weak bones and bone pain.