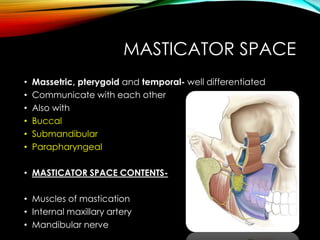
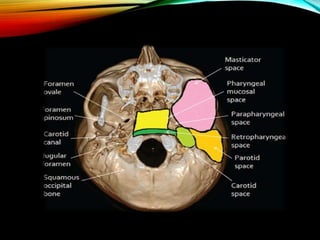
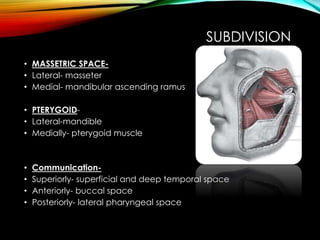
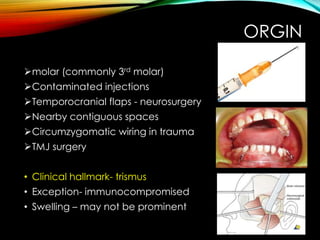
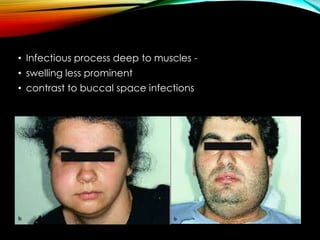
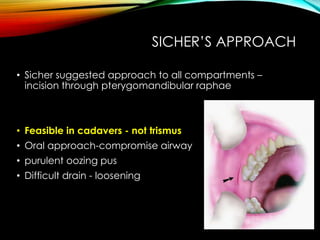
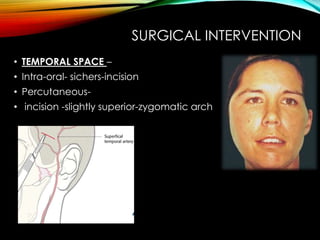
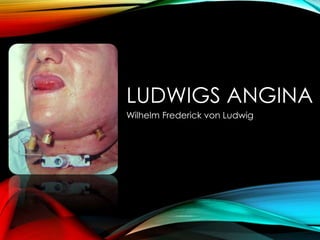
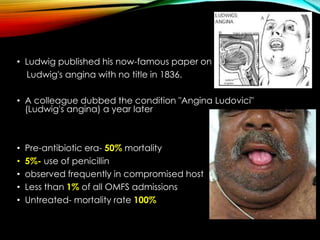
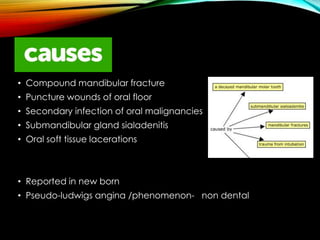
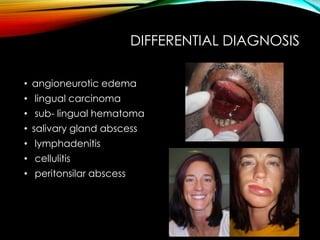
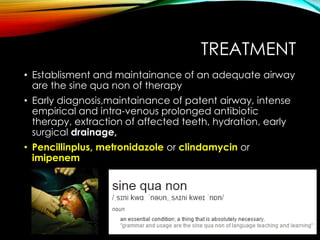
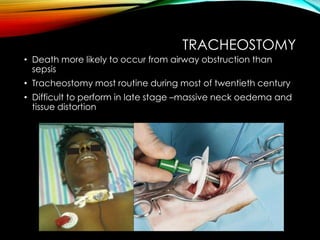
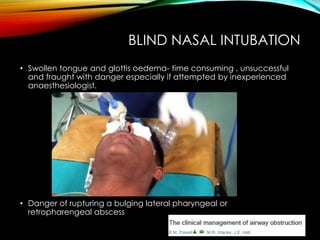
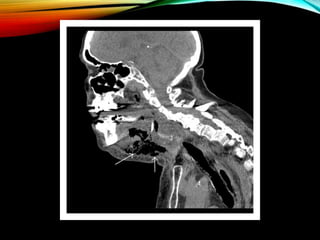
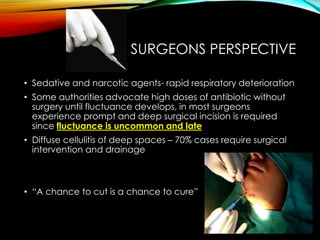
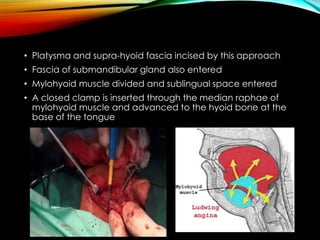
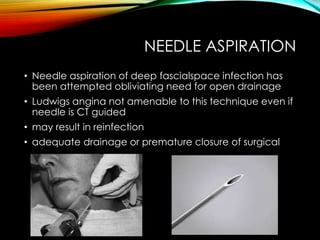
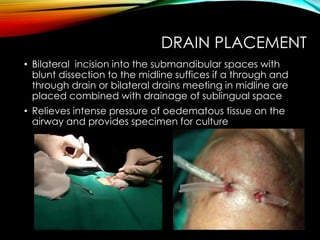
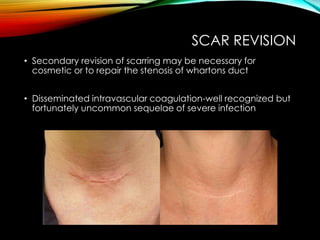
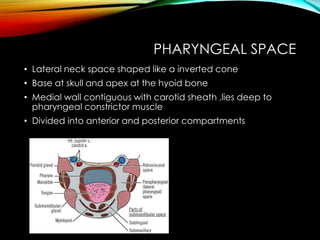
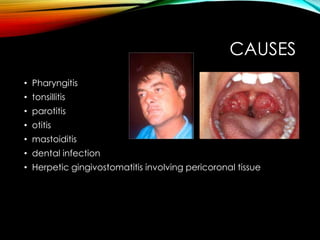
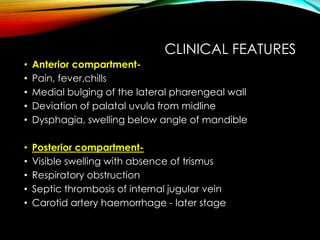
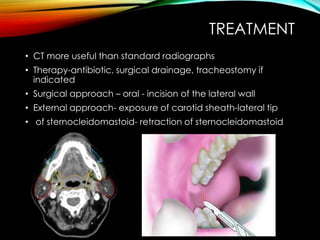
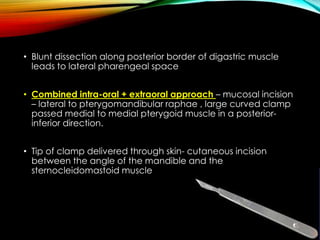
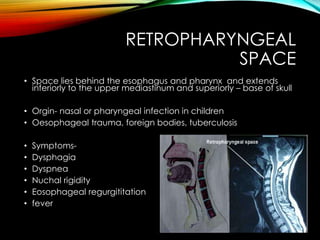
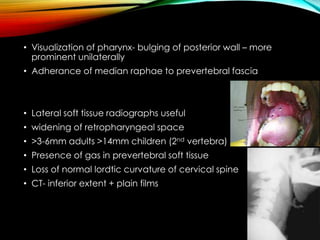
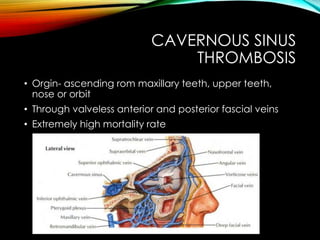
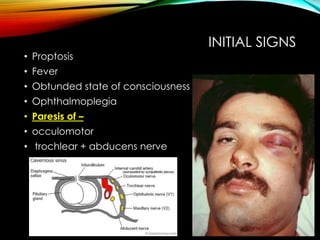
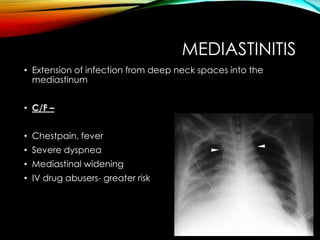
The document provides a comprehensive overview of deep fascial space infections, including specifics about the masticatory space, Ludwig's angina, pharyngeal infections, and cavernous sinus thrombosis. It highlights clinical features, microbiology, diagnostic approaches, and treatment strategies for various infections, emphasizing the importance of early recognition and intervention. Attention is drawn to significant historical aspects and contemporary practices in managing these serious infections within oral and maxillofacial surgery.