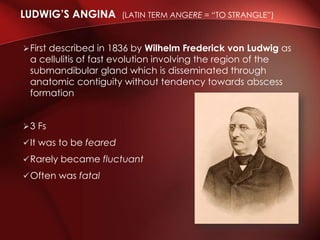
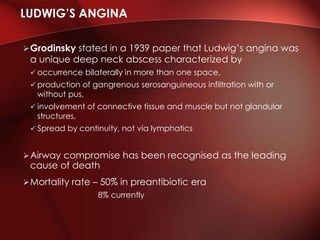
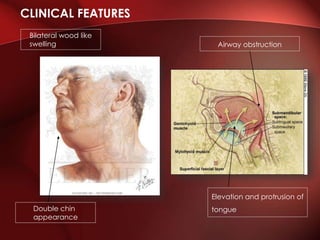
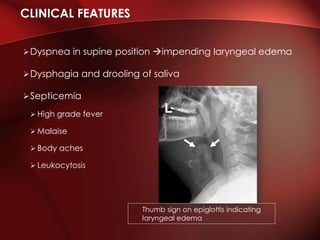
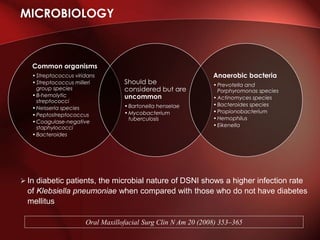
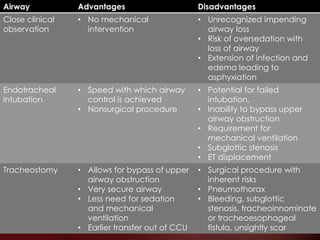
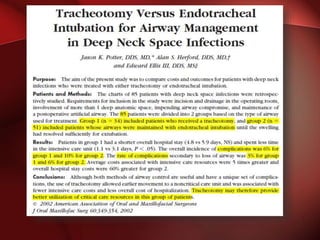
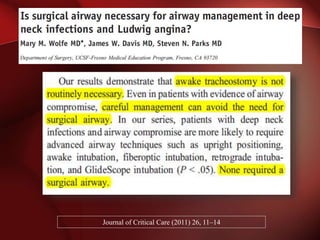
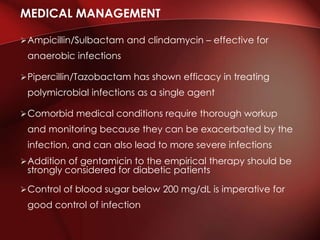
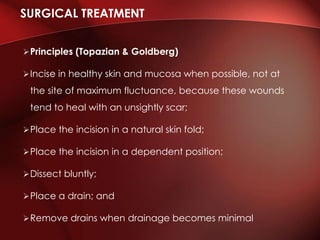
The document discusses Ludwig's angina, a serious cellulitis of the submandibular region with potential for airway compromise and high mortality rates if untreated. It covers etiology, clinical presentation, microbiology, investigations, treatment options, and the importance of early diagnosis and aggressive management to ensure patient safety. Treatment strategies include empirical antibiotic therapy, airway management techniques, and surgical intervention when necessary.