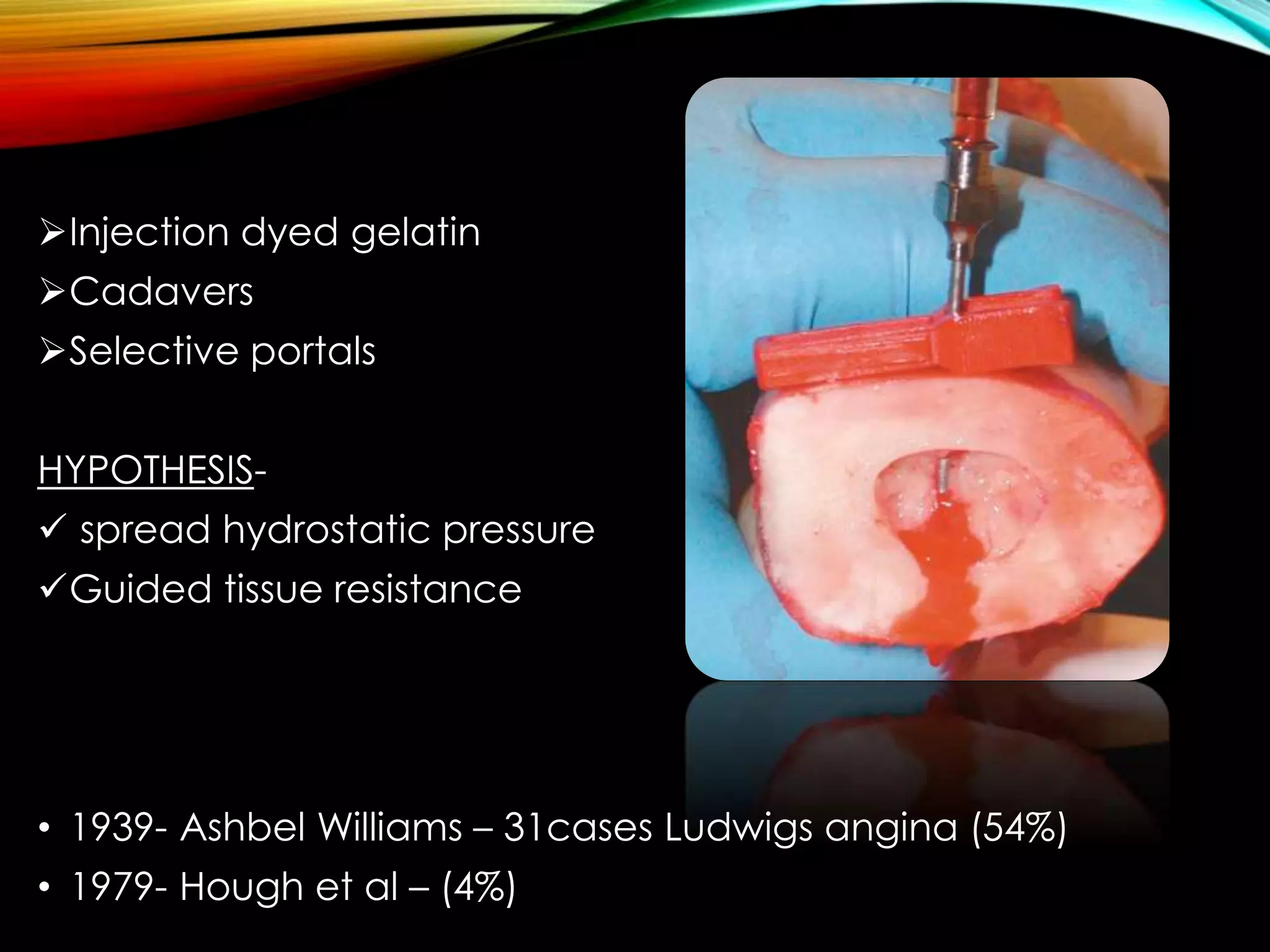
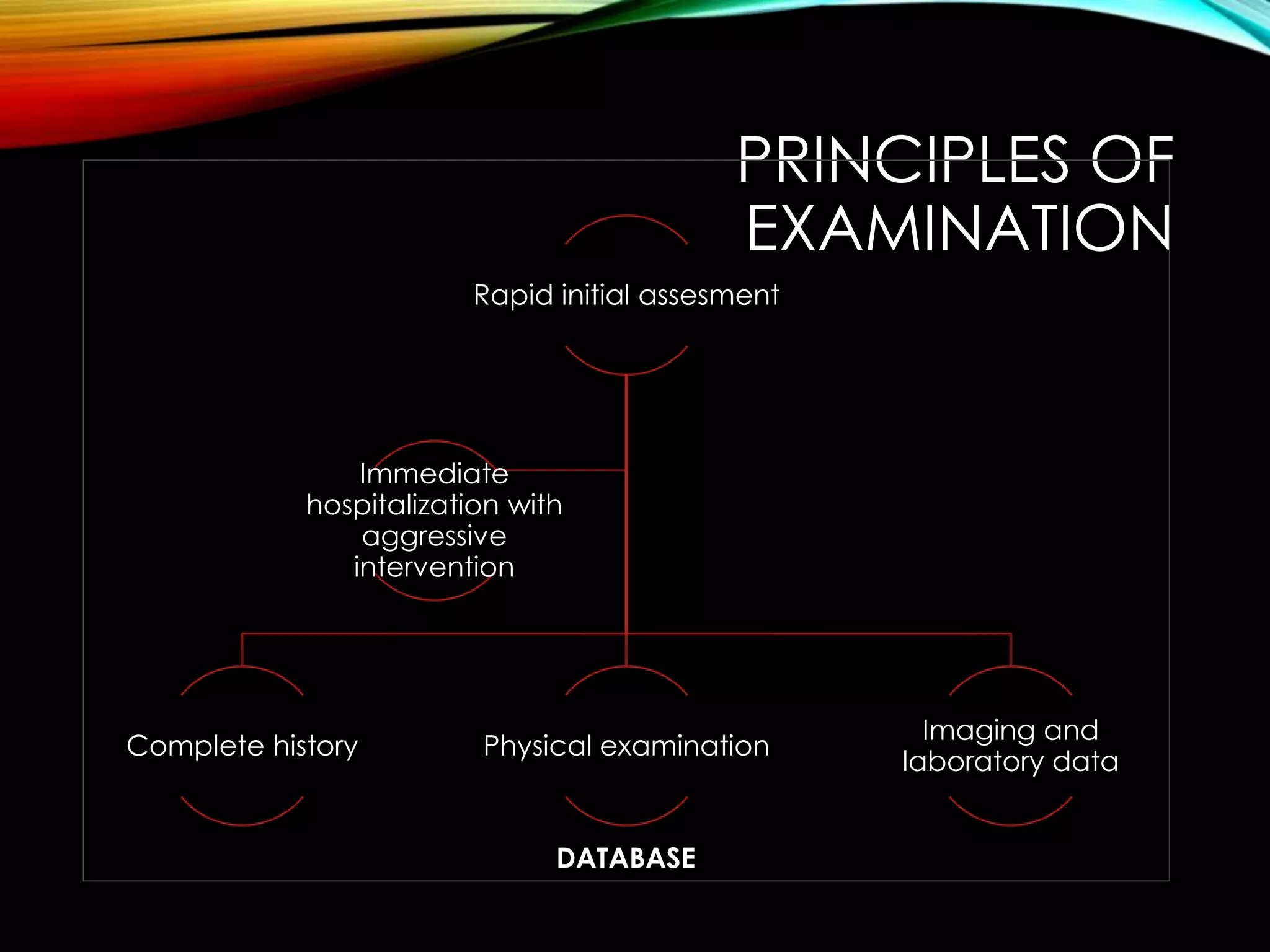
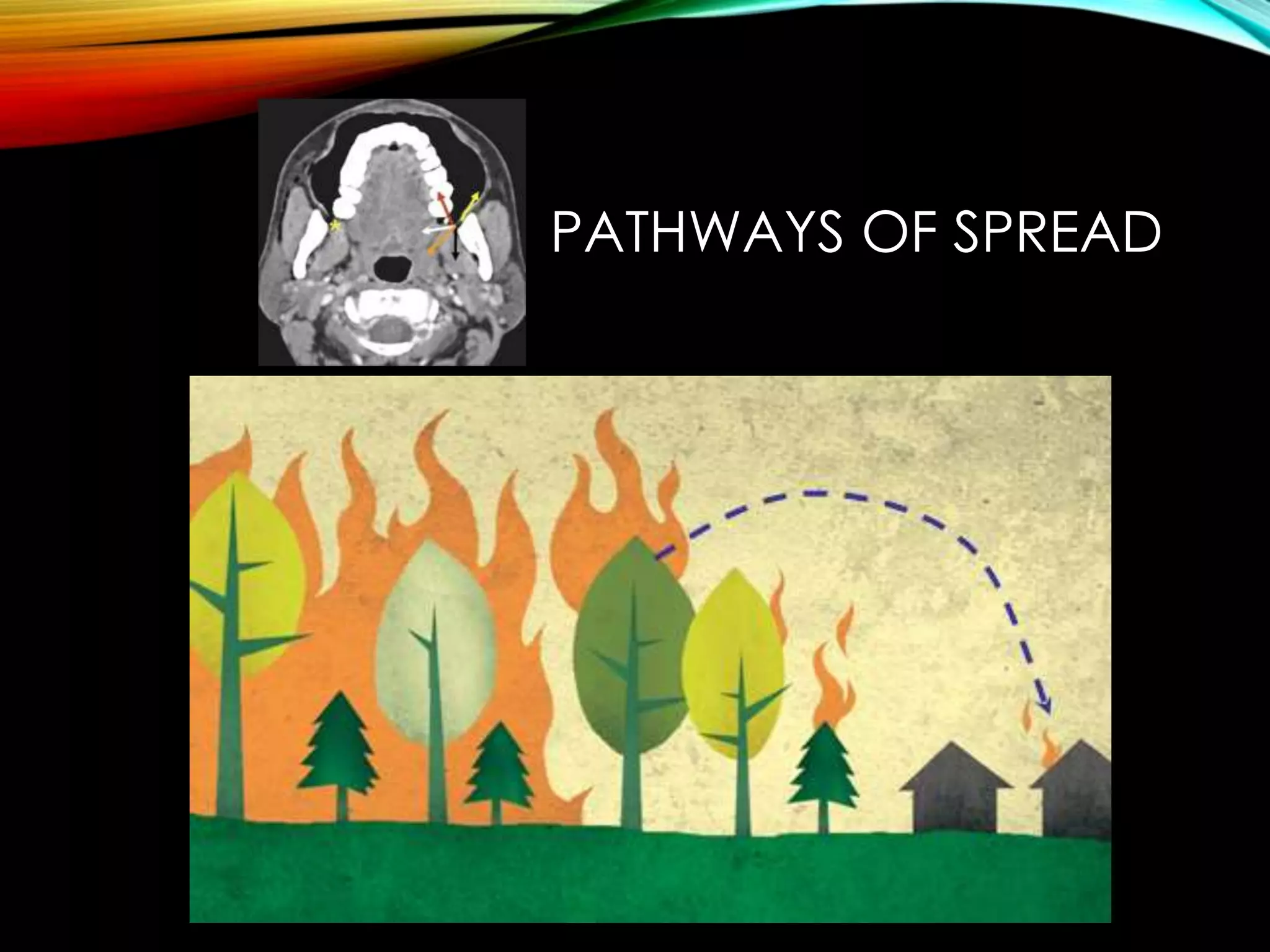
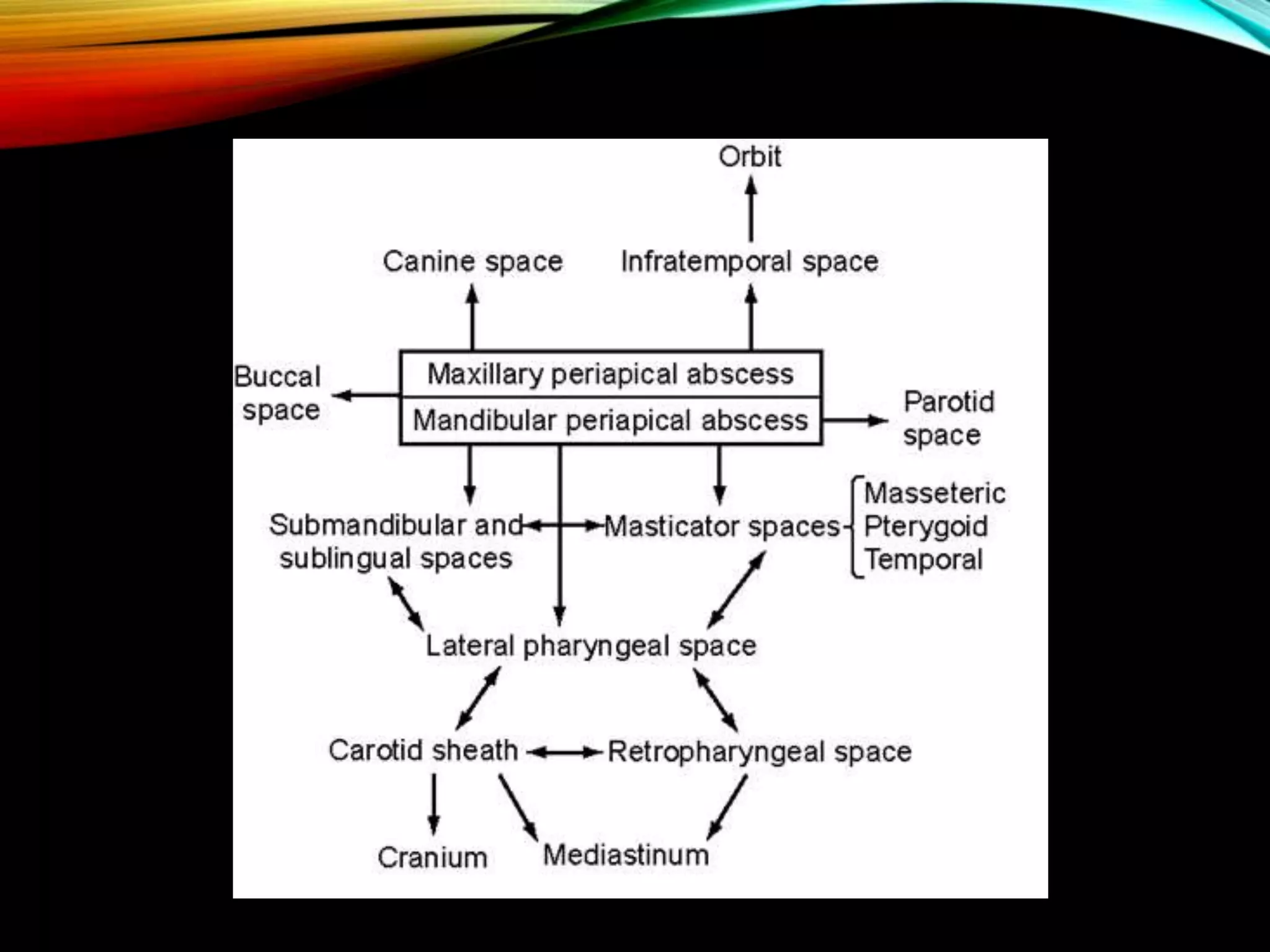
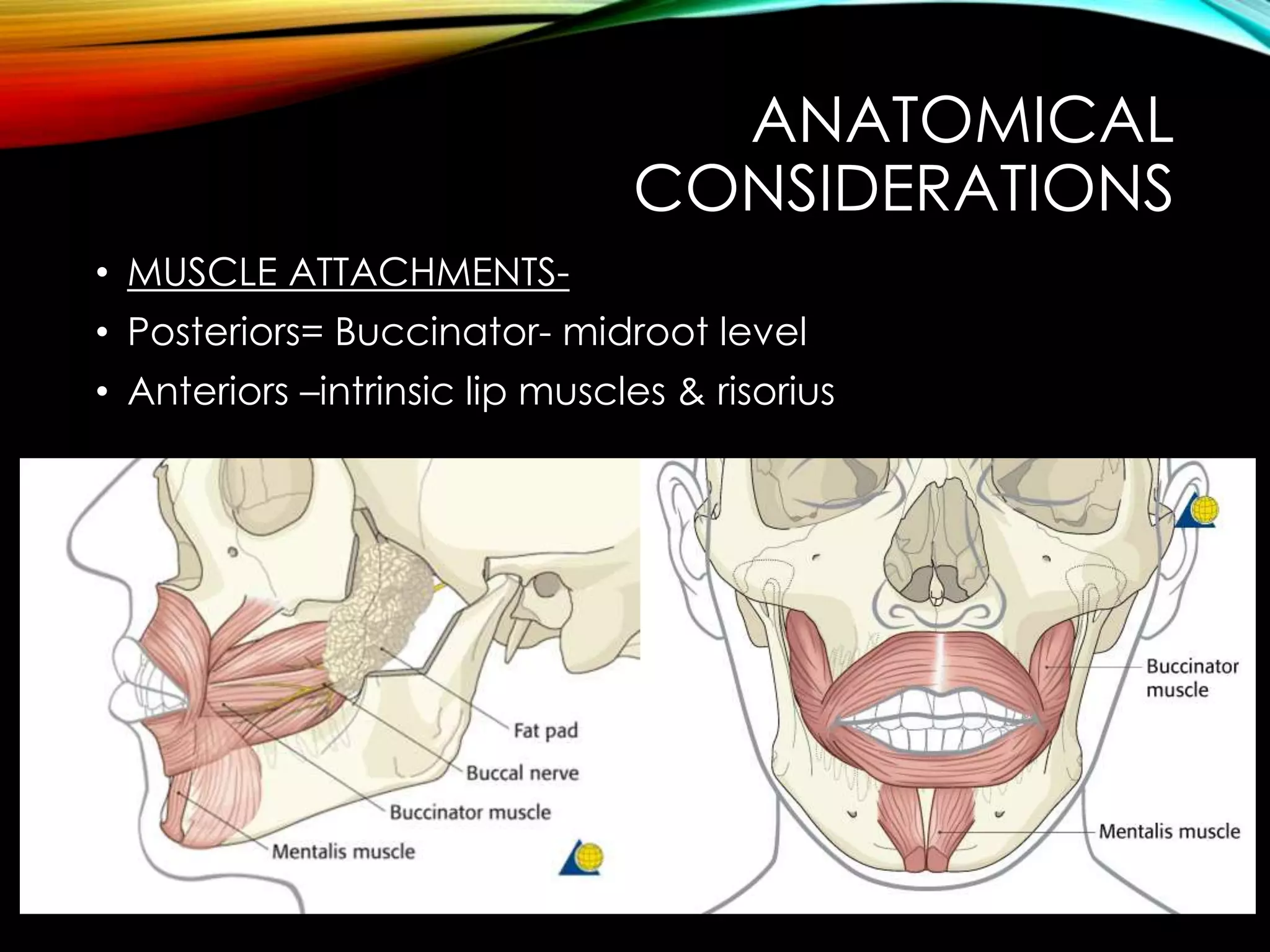
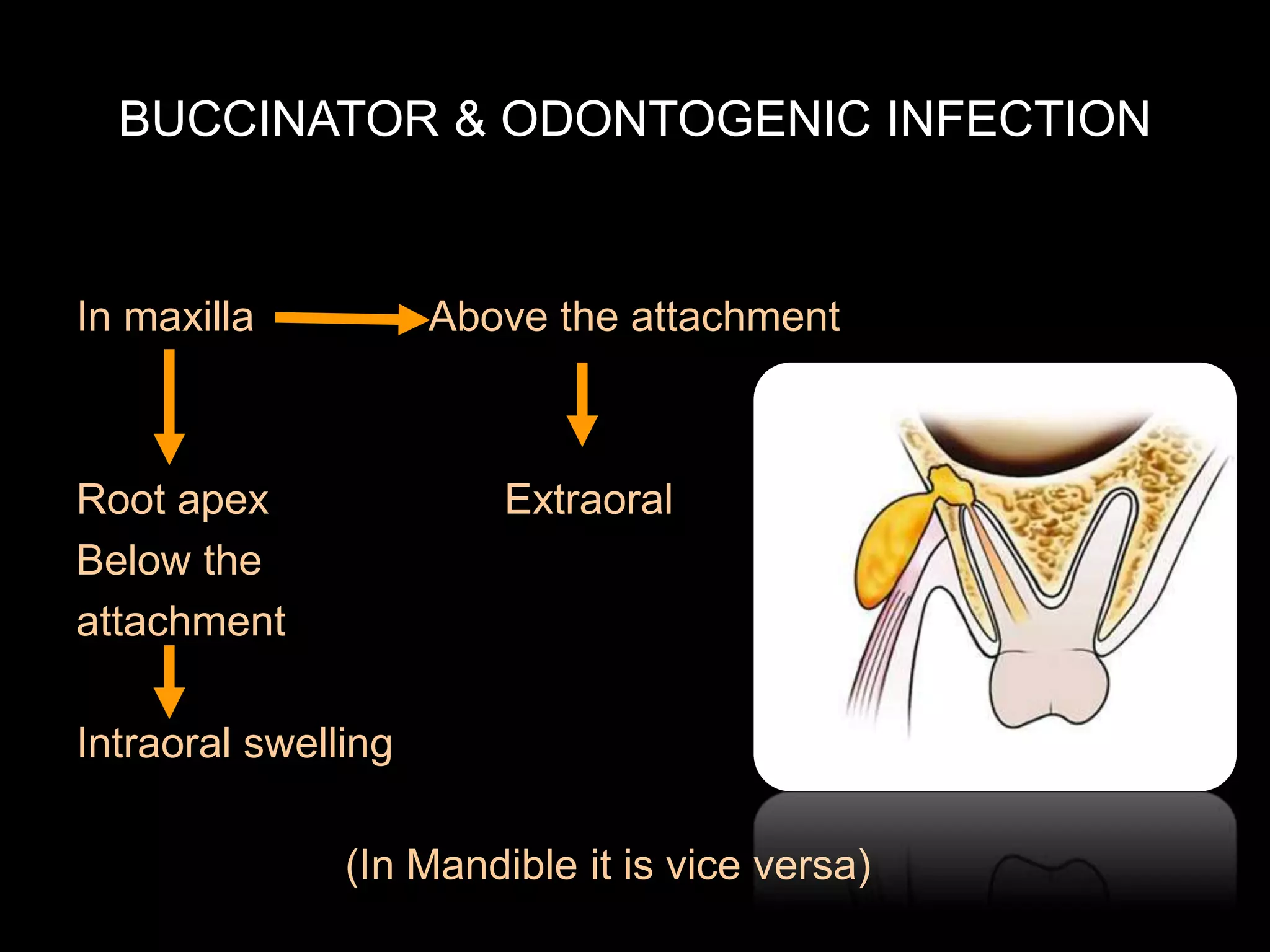
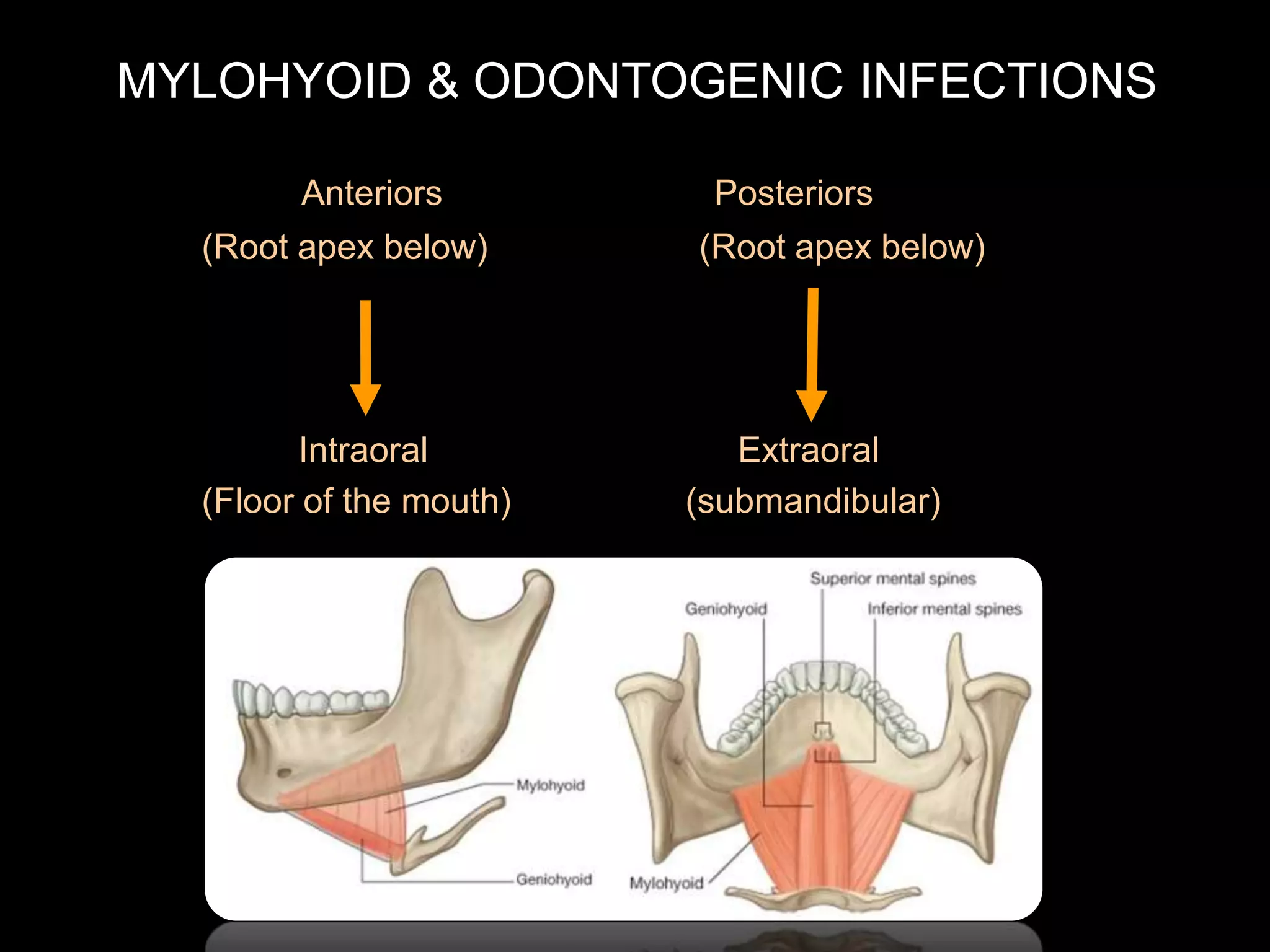
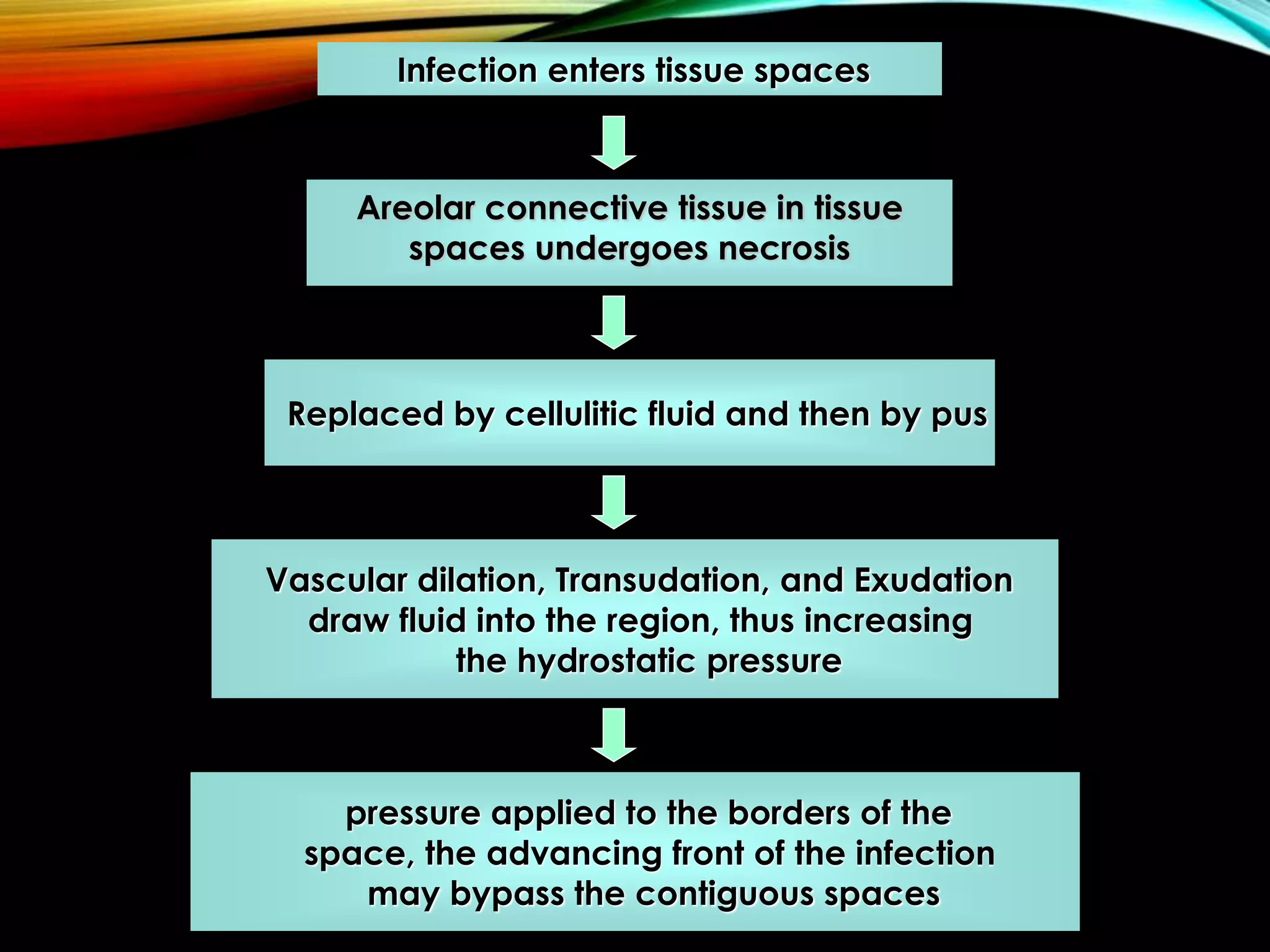
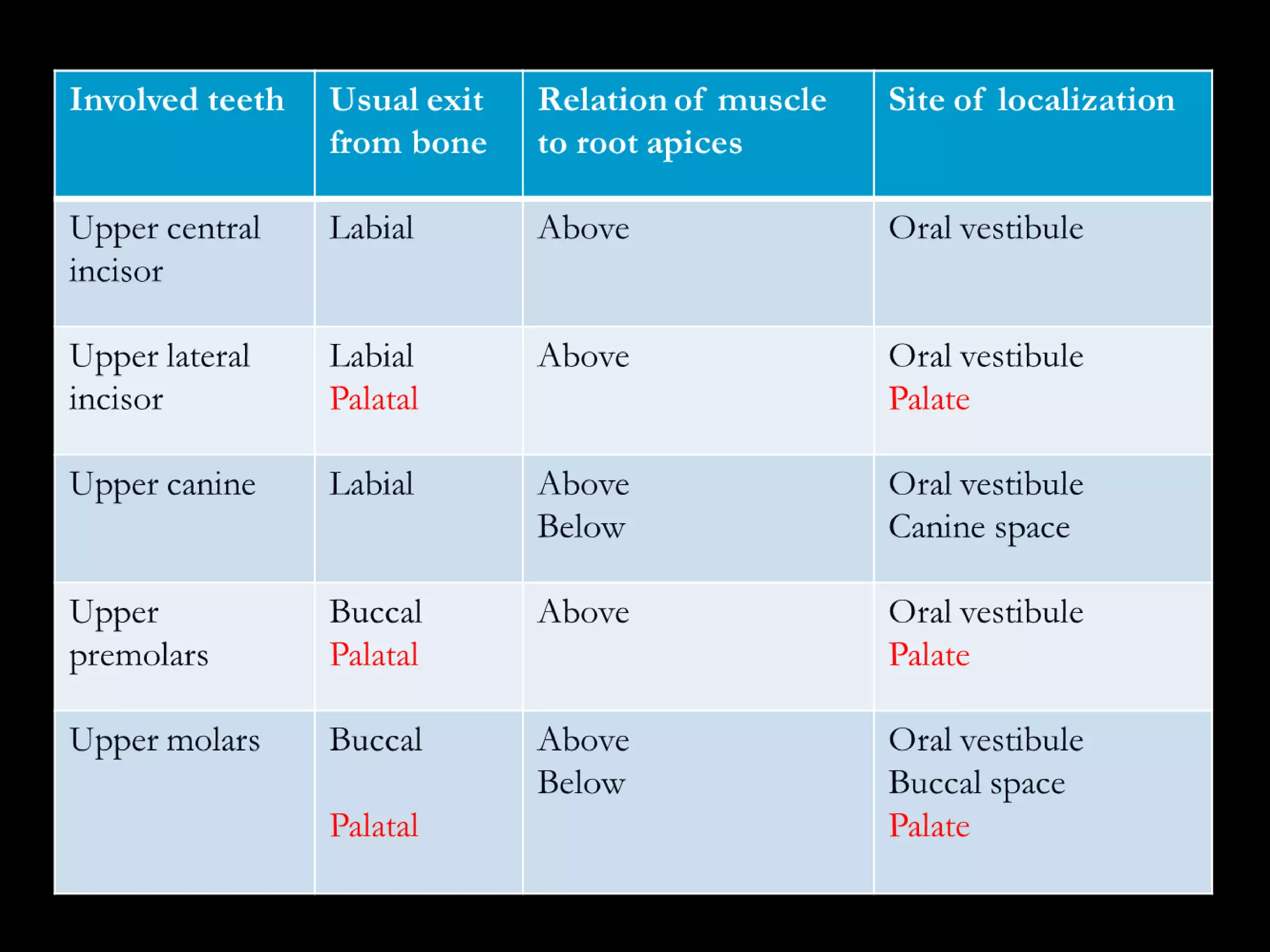
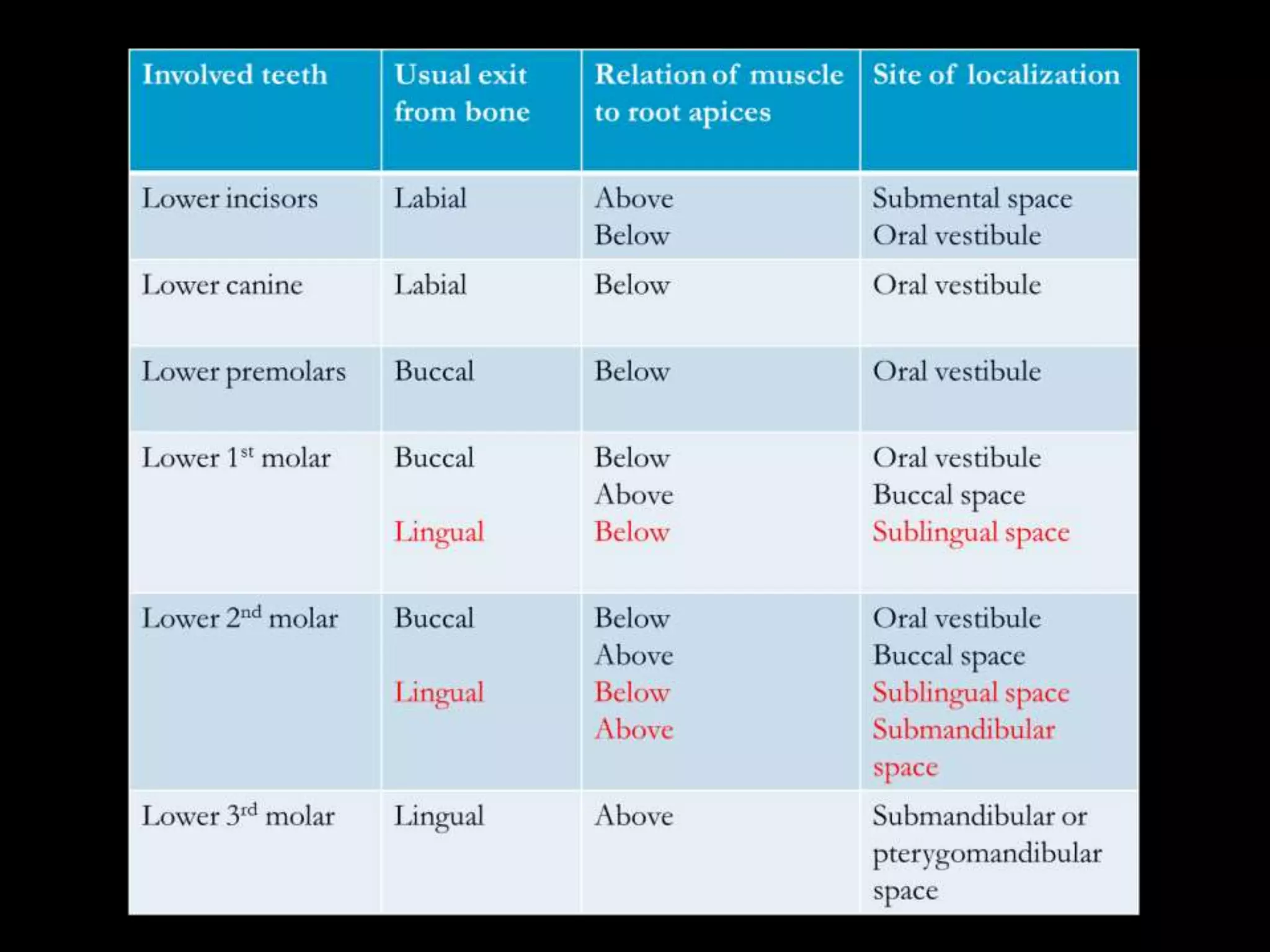
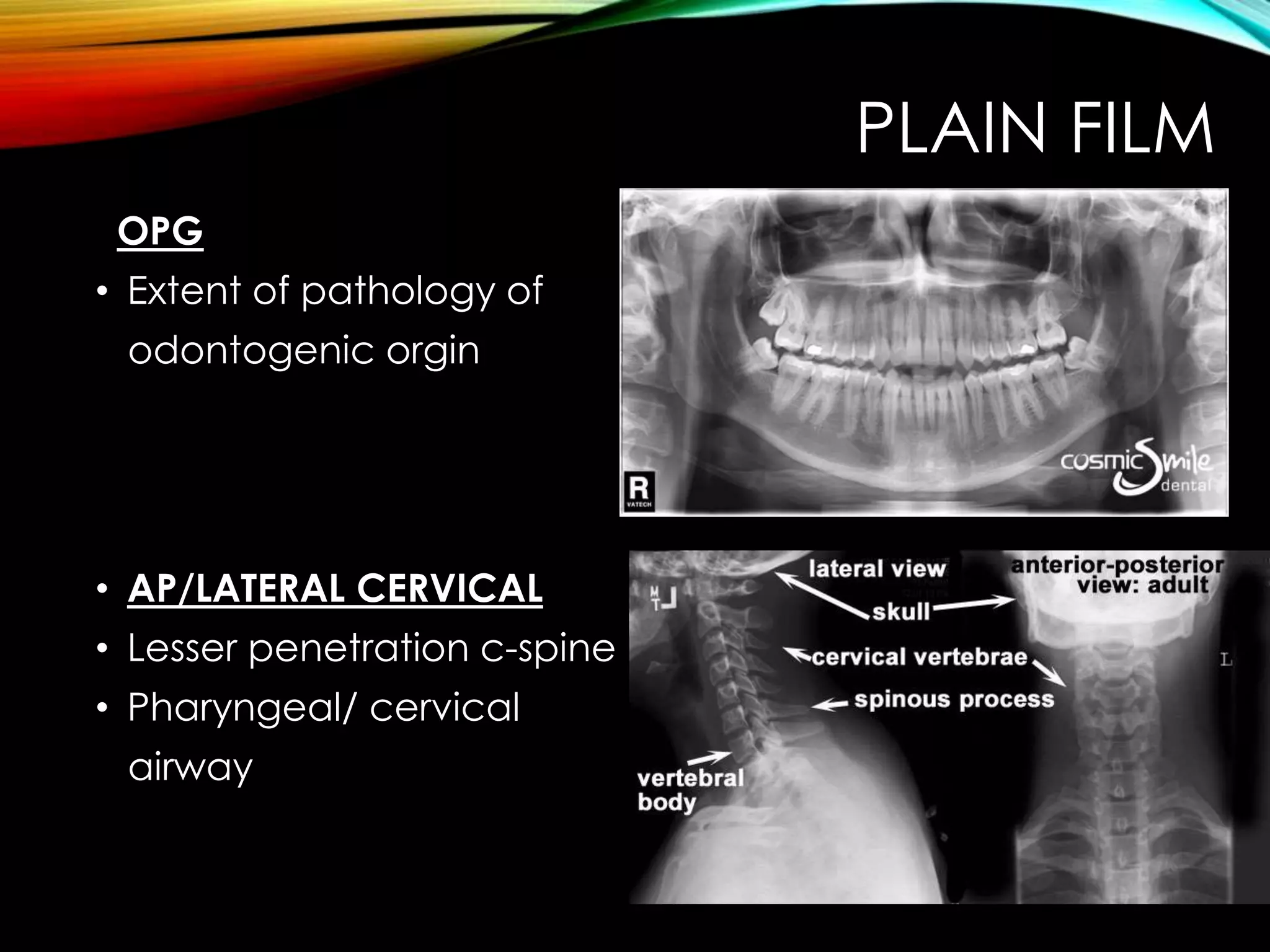
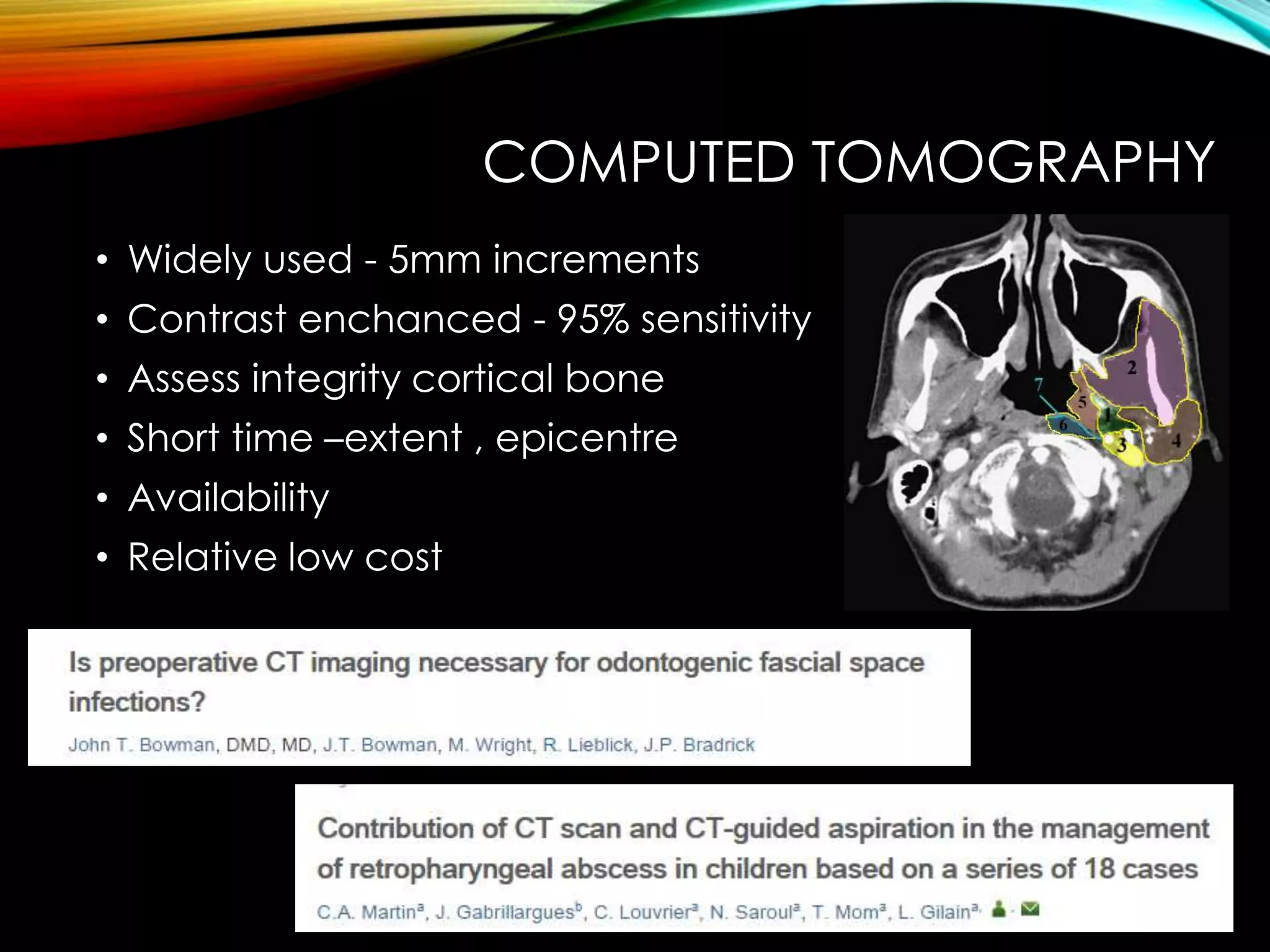
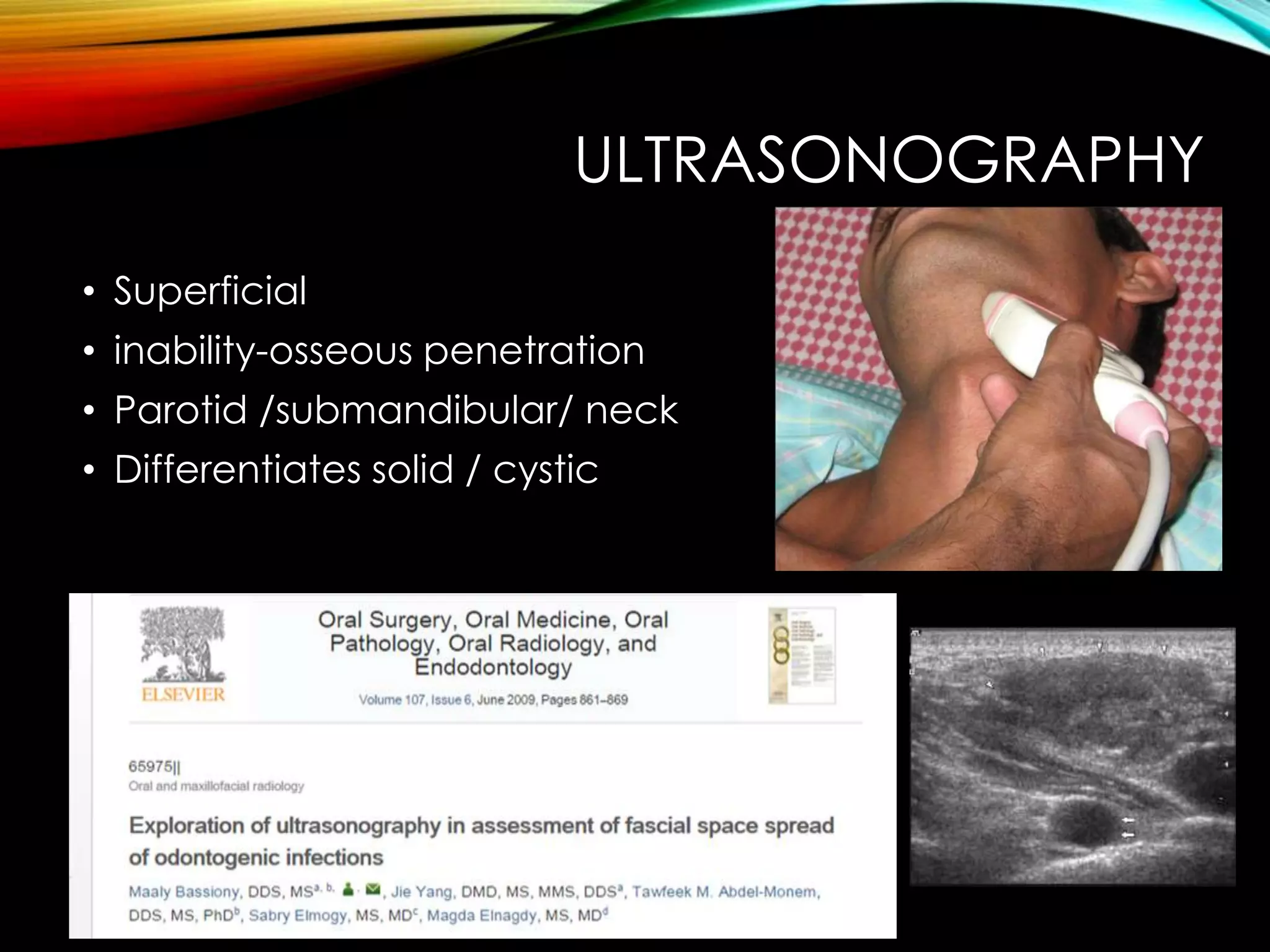
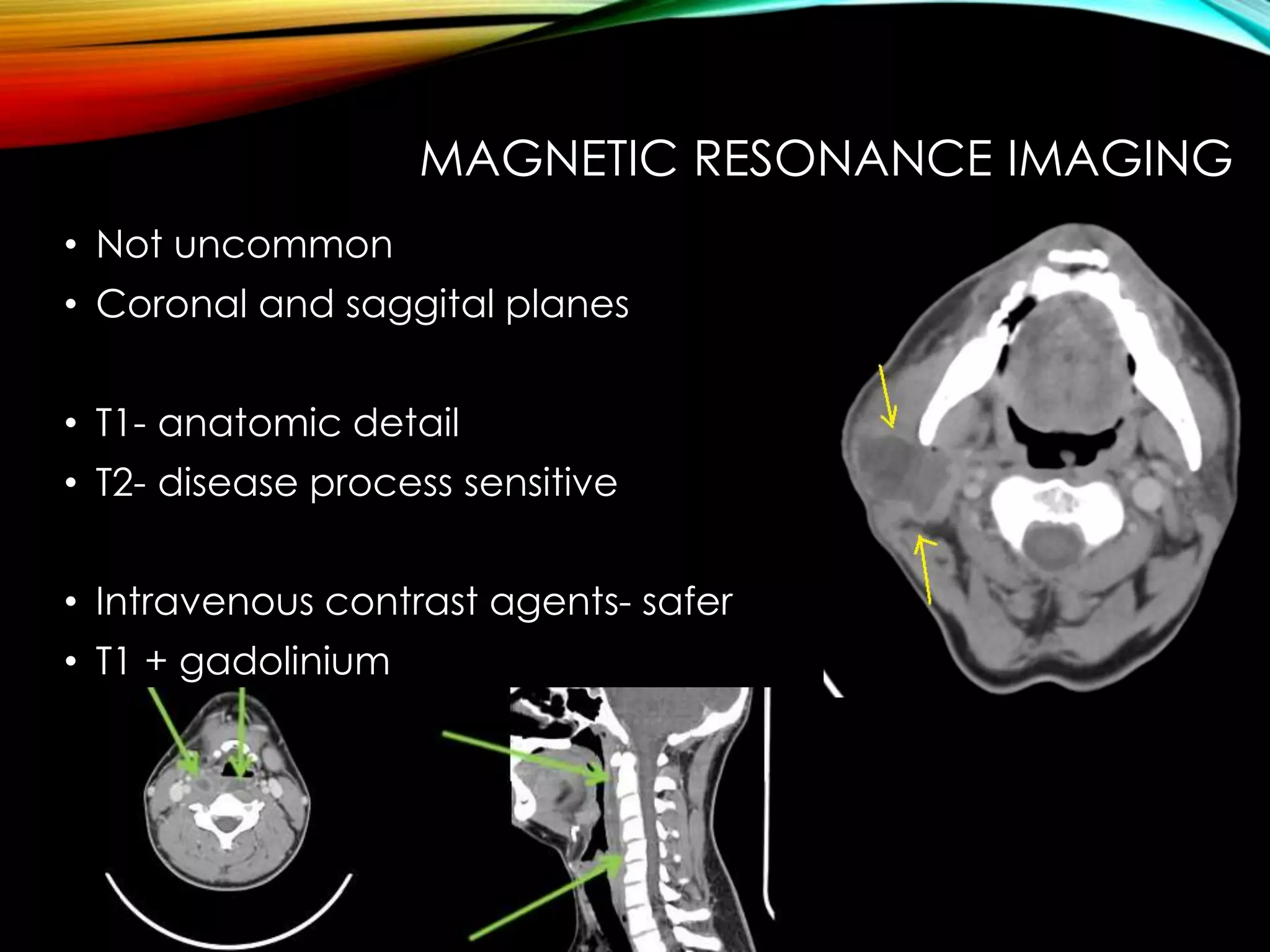
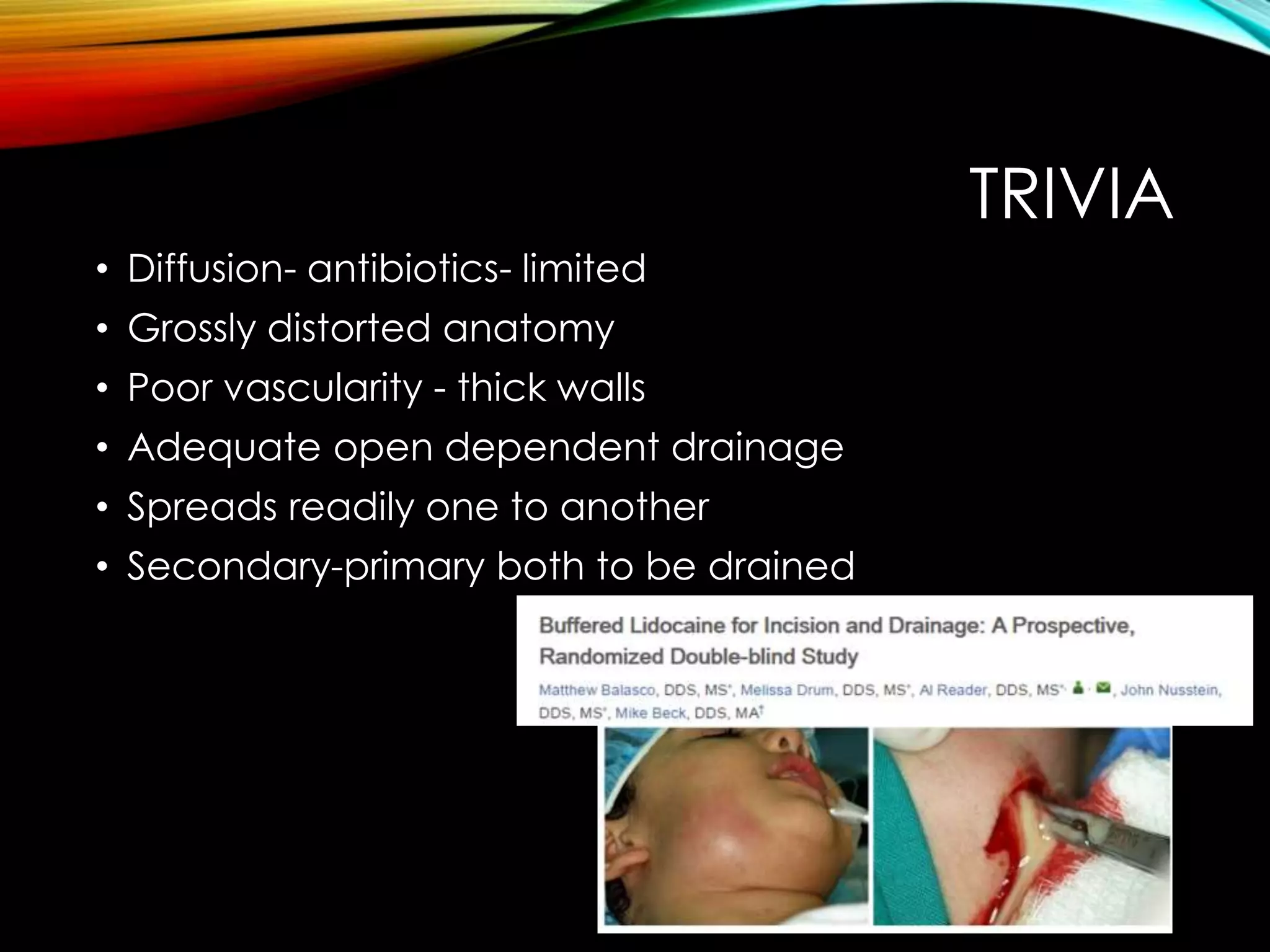
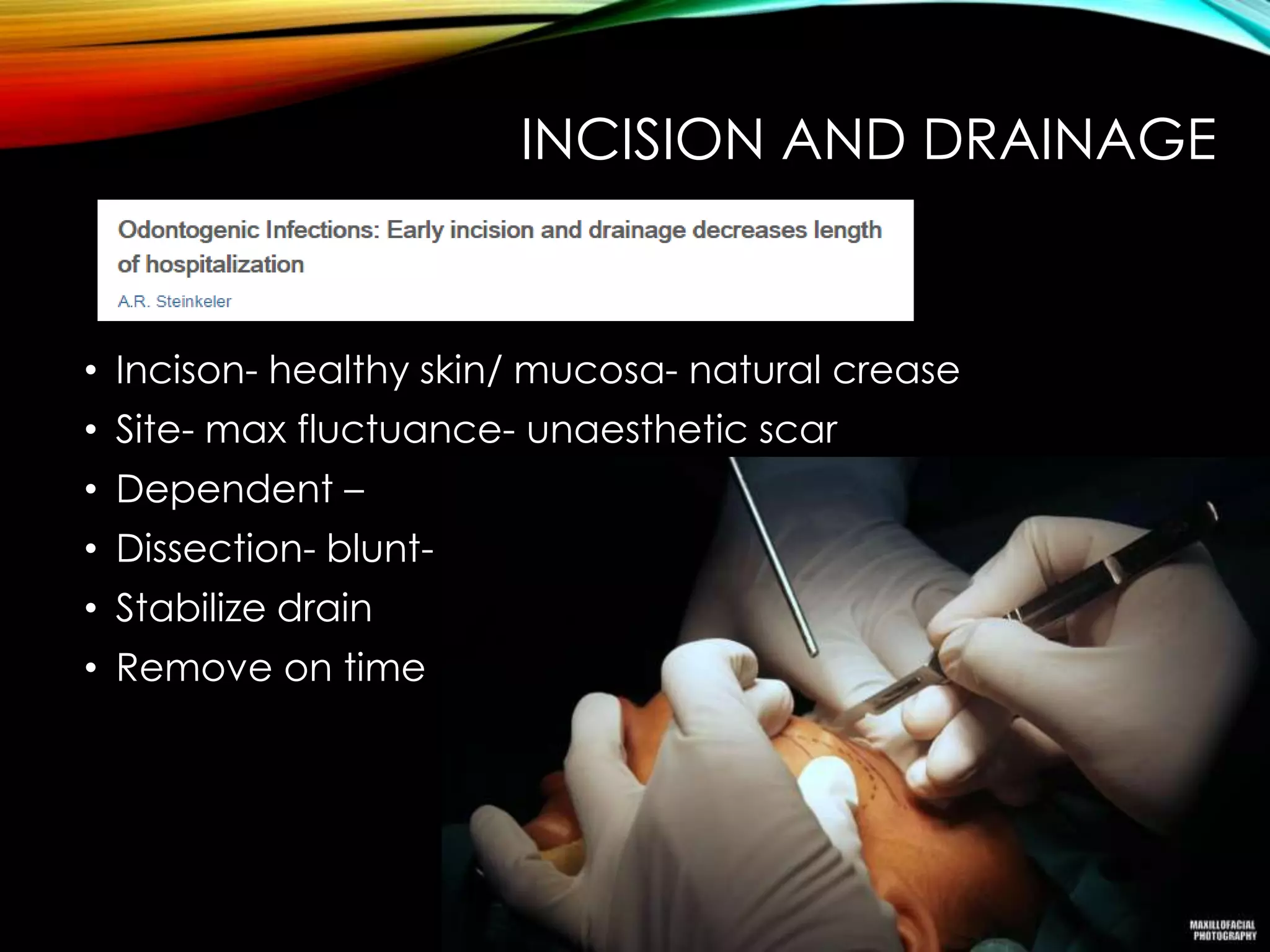
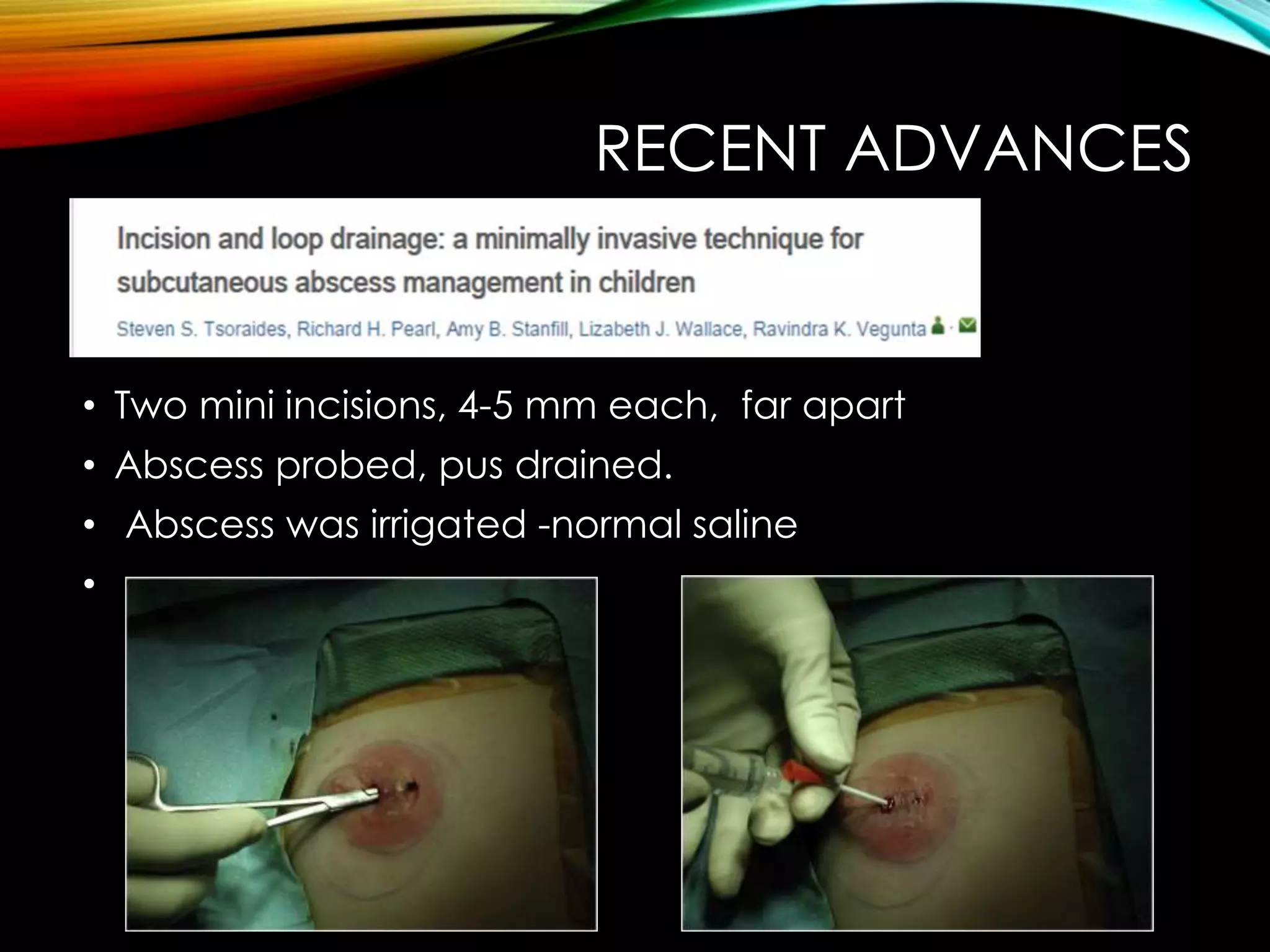
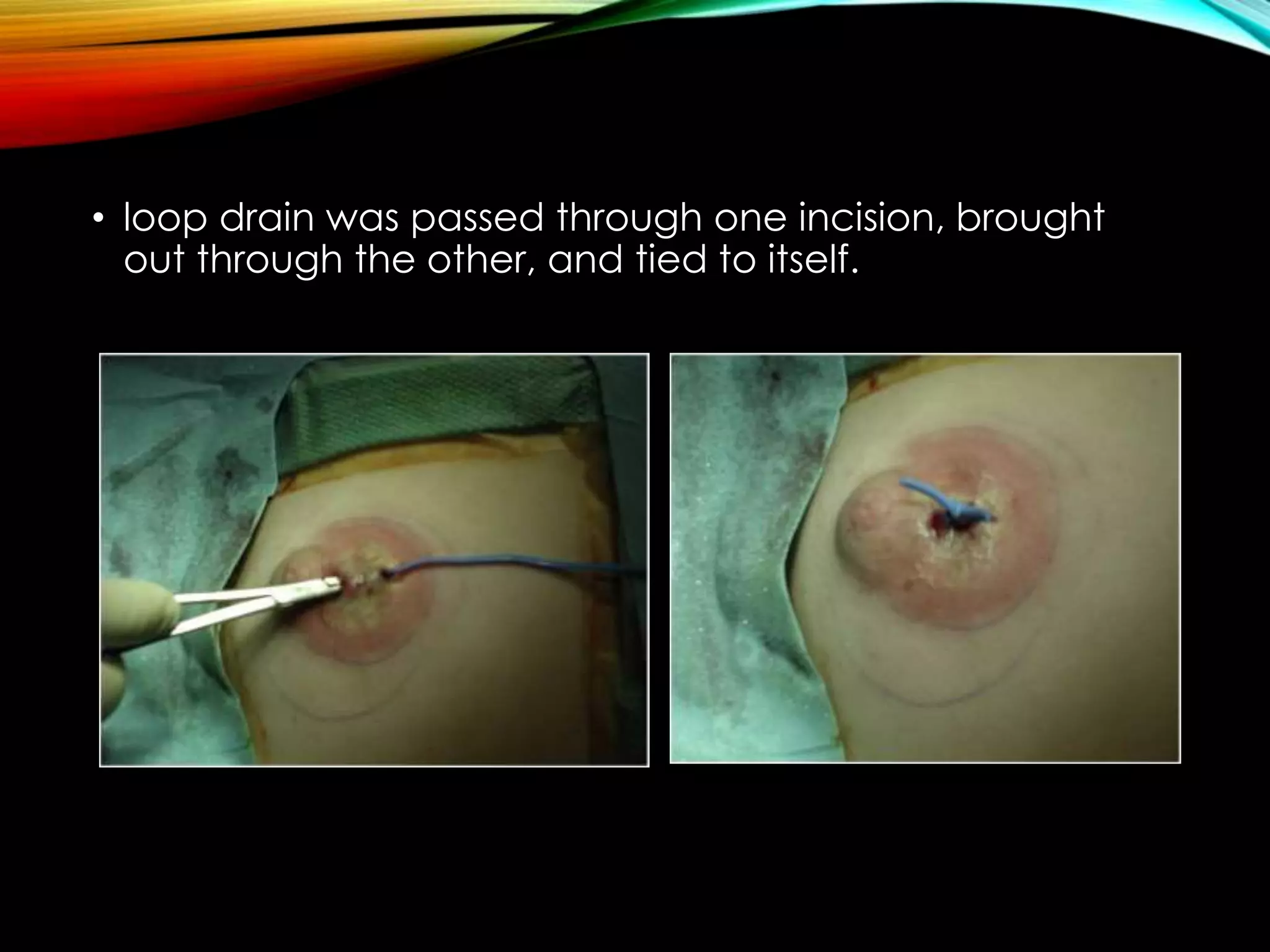
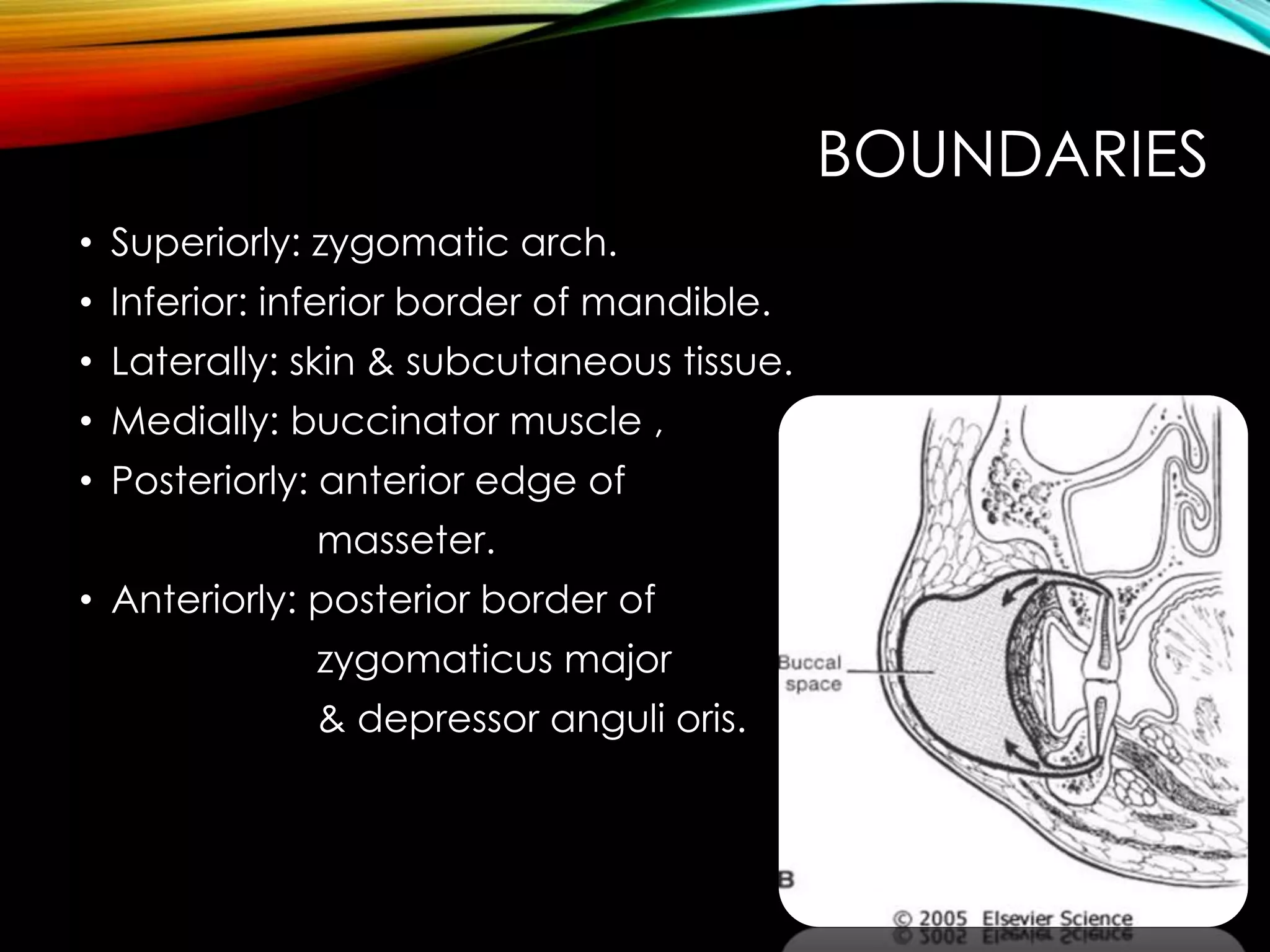
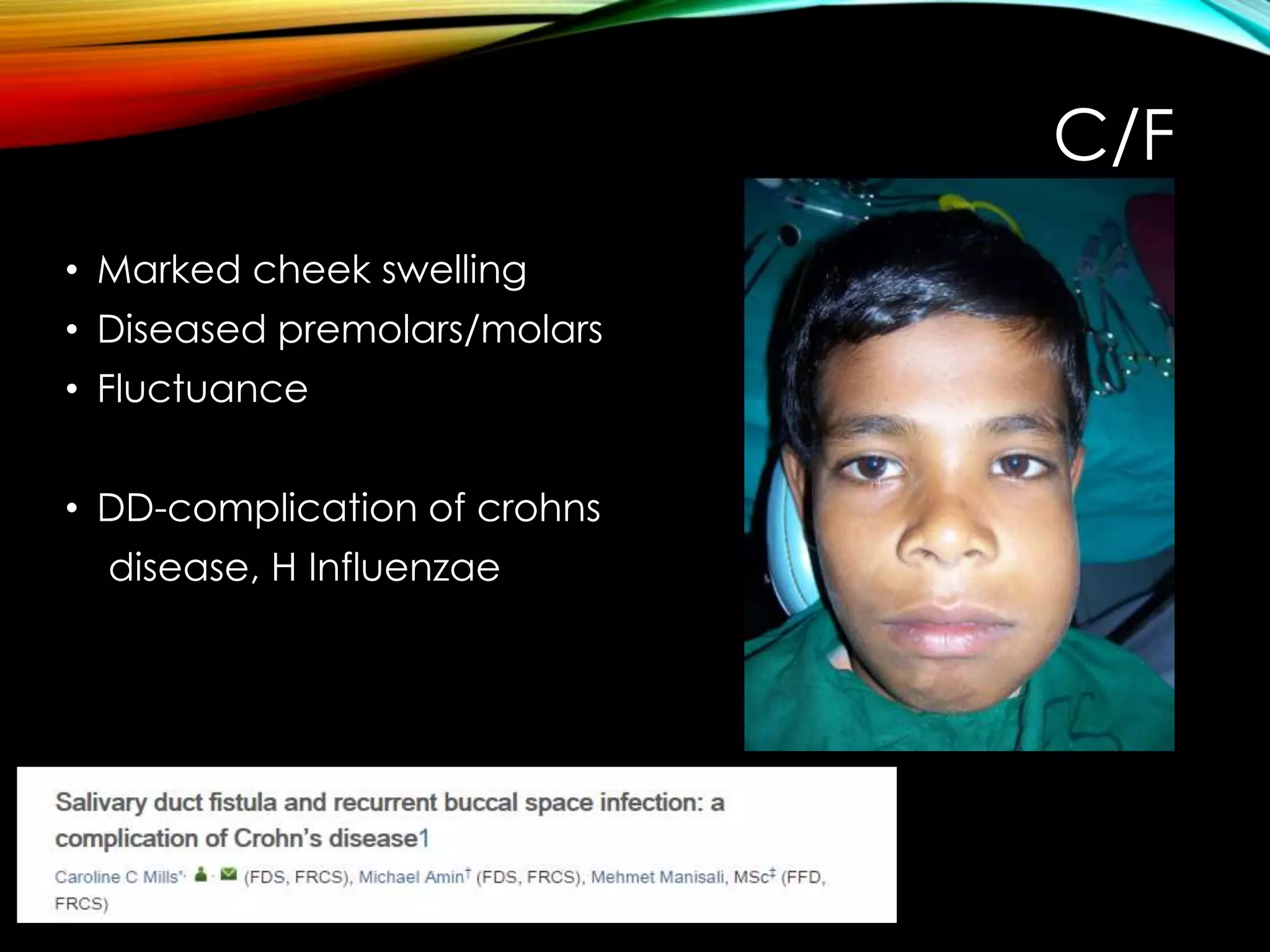
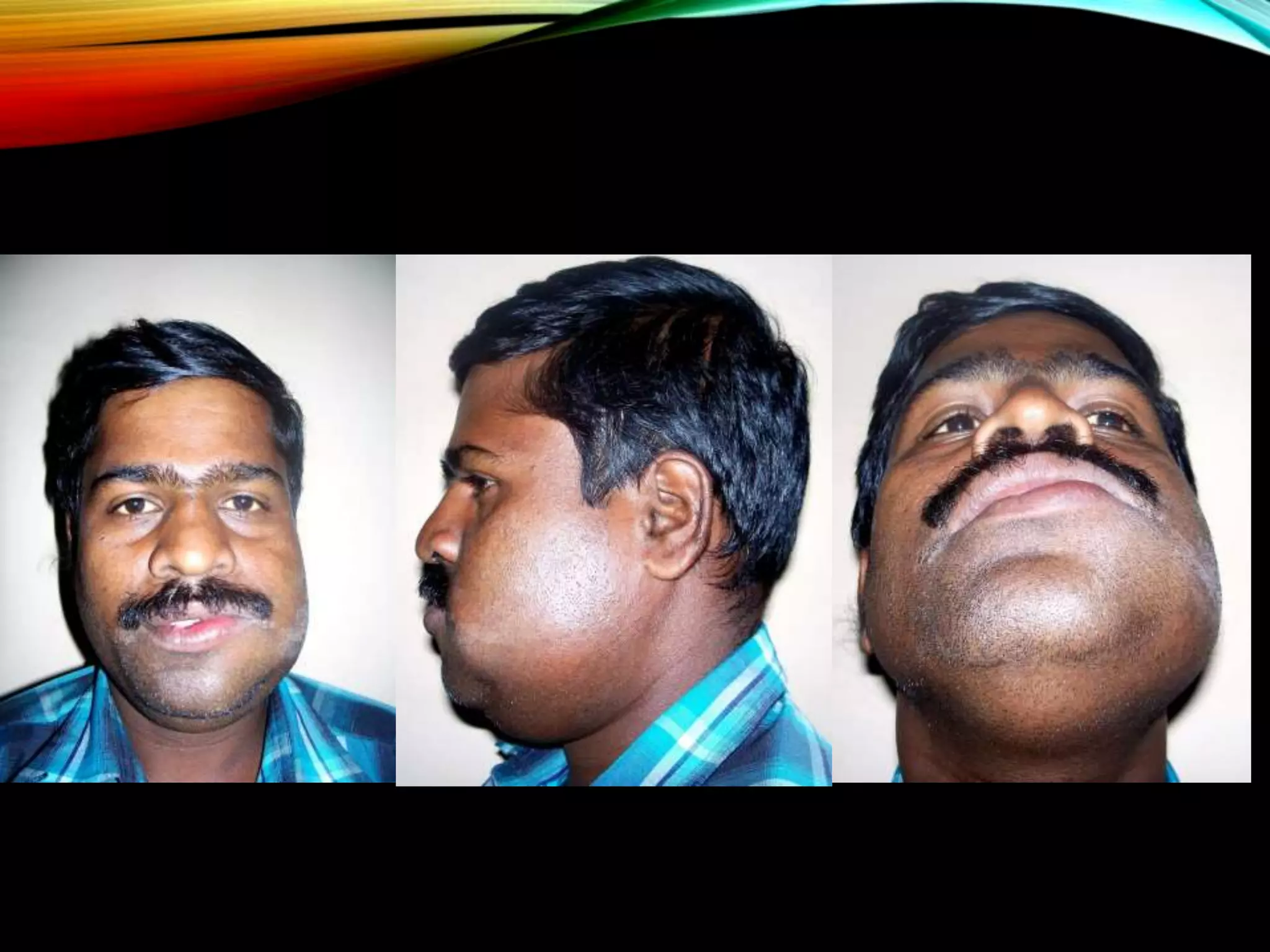
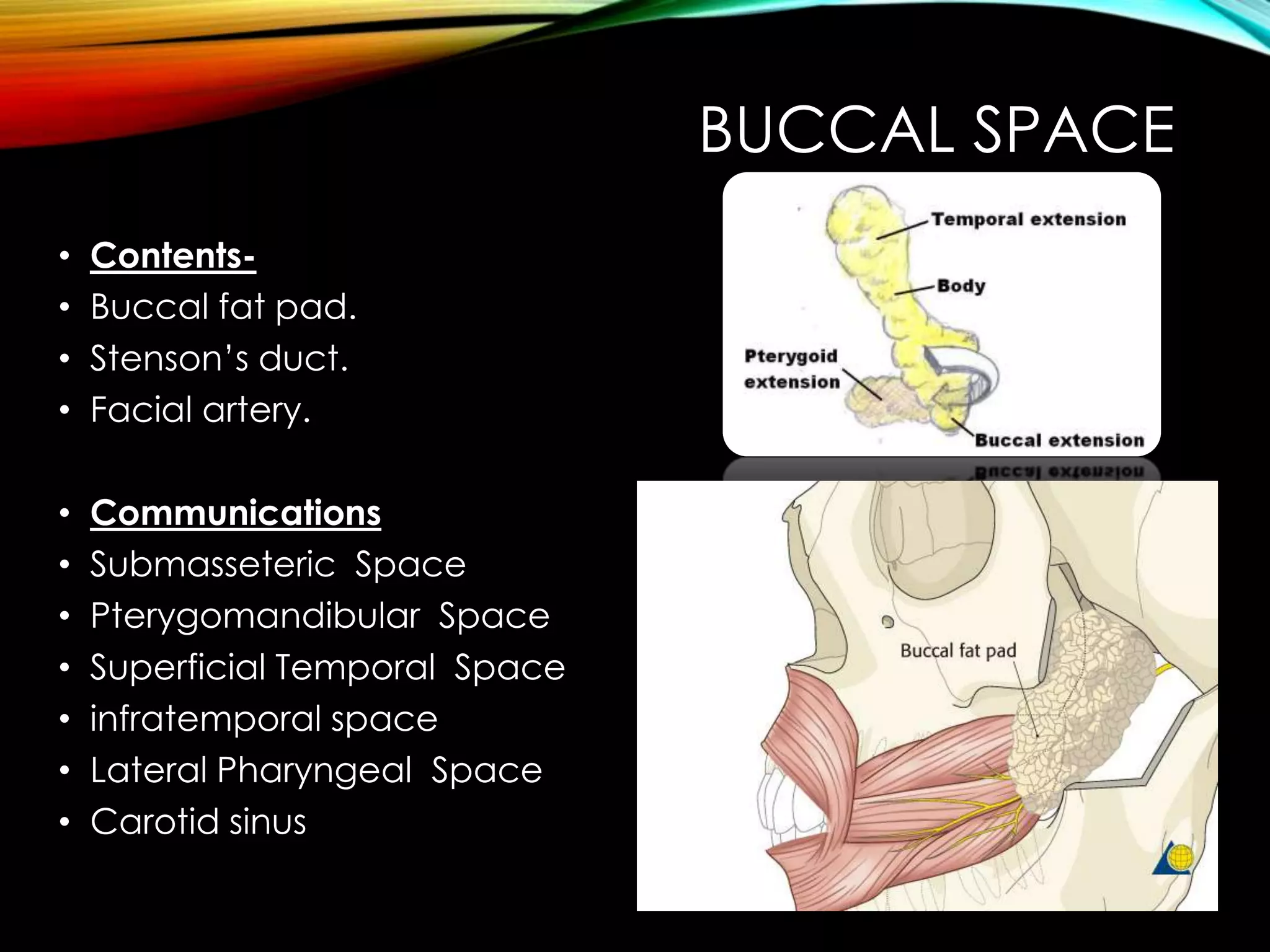
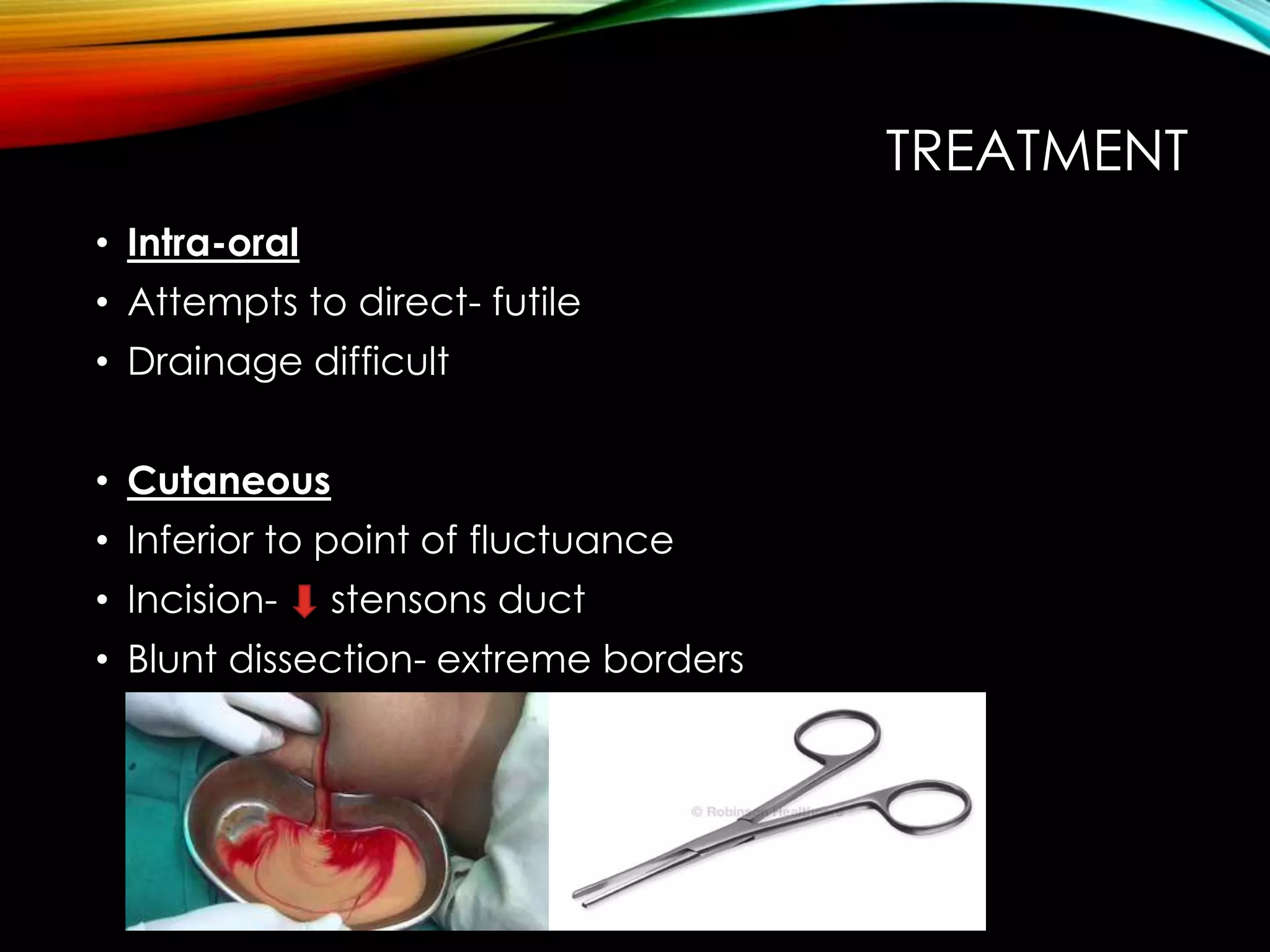
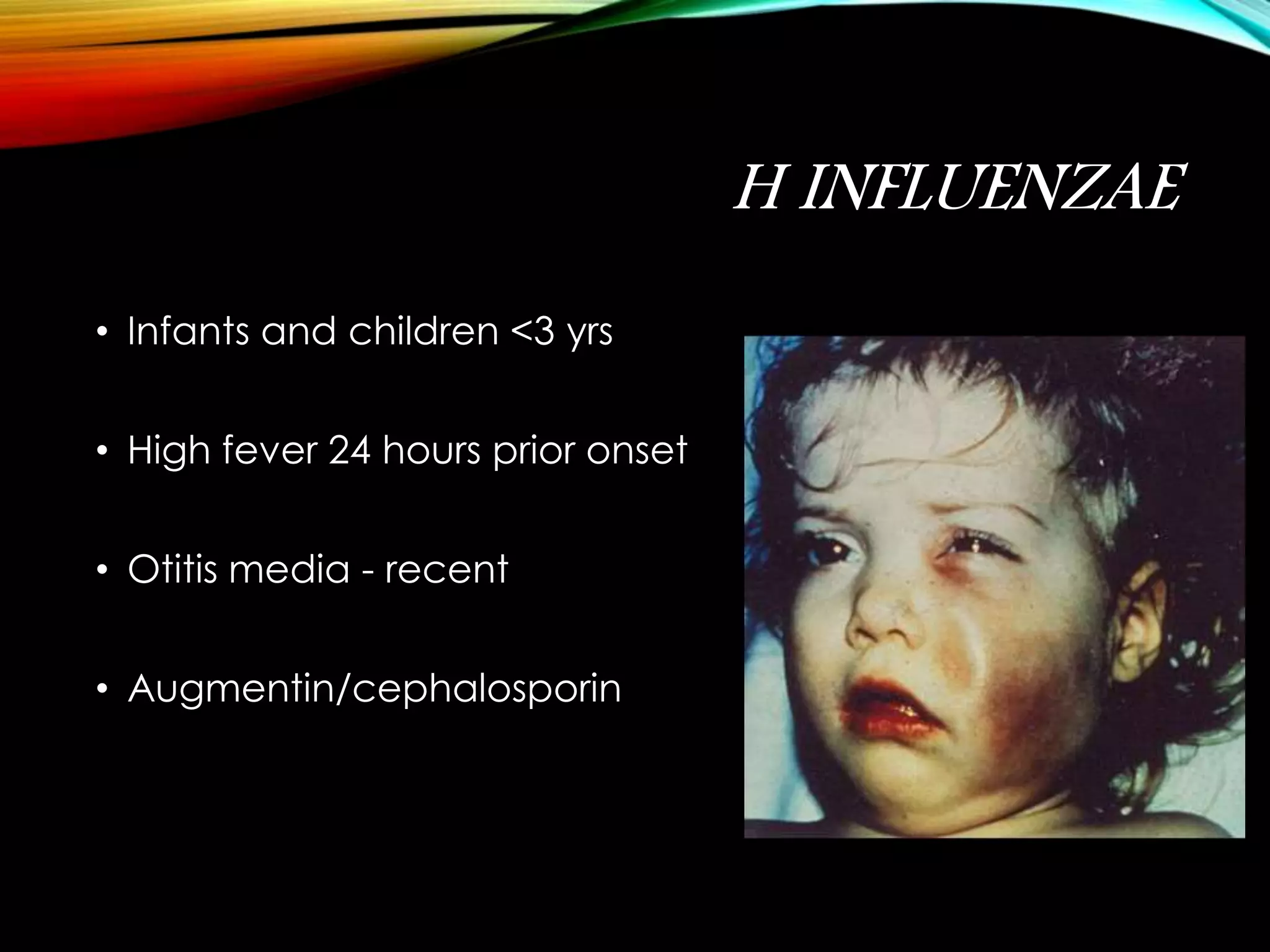
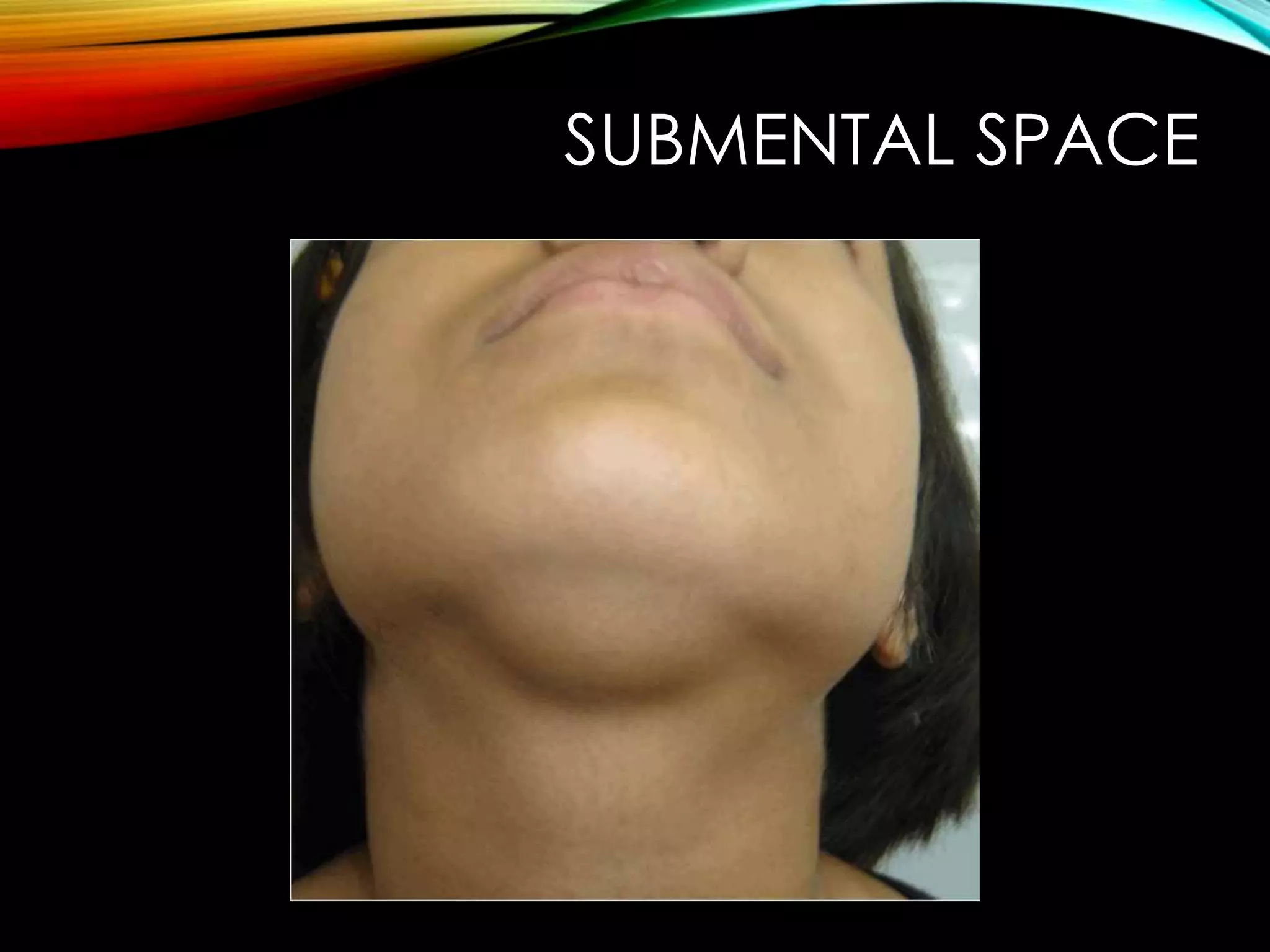
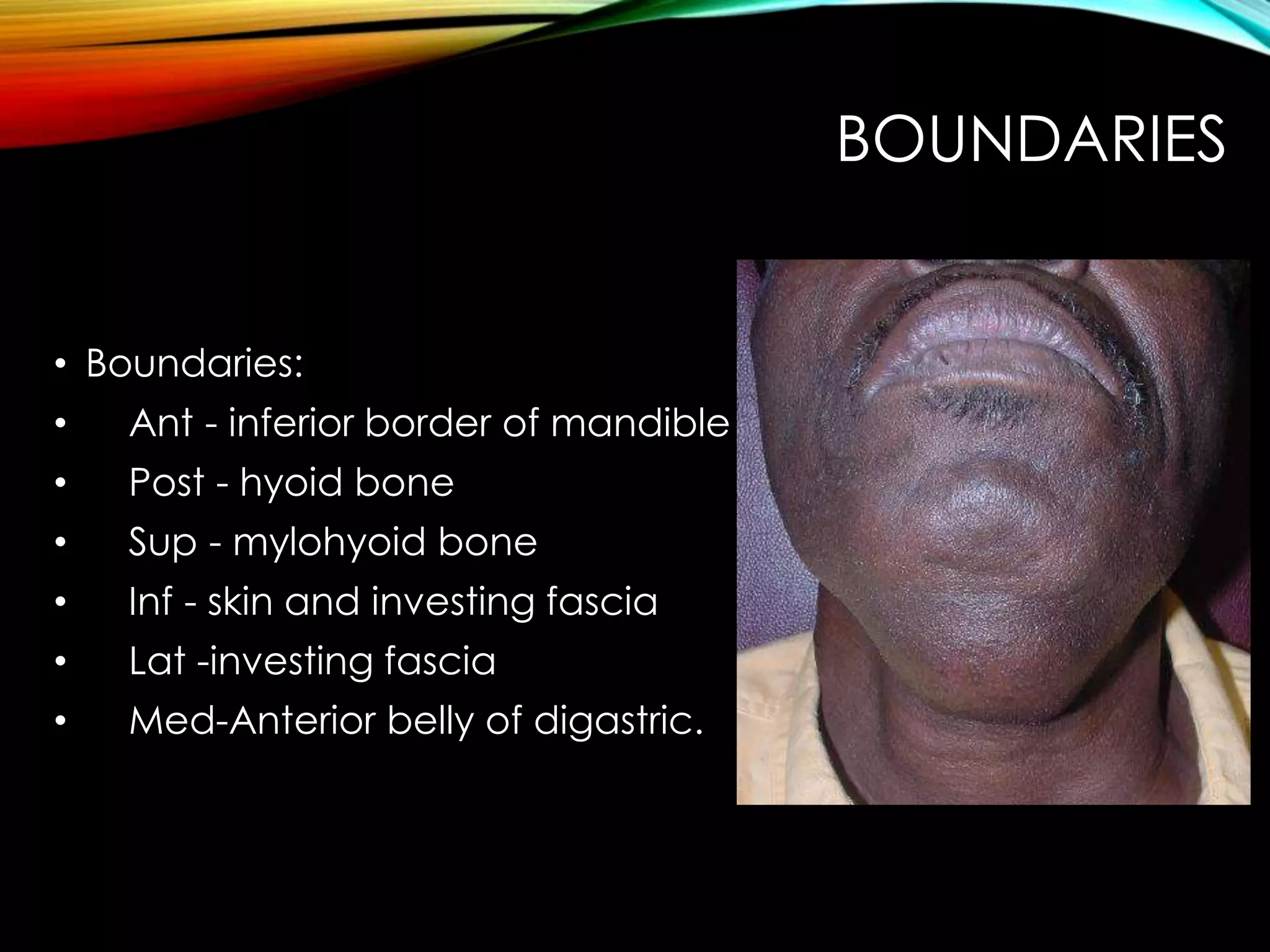
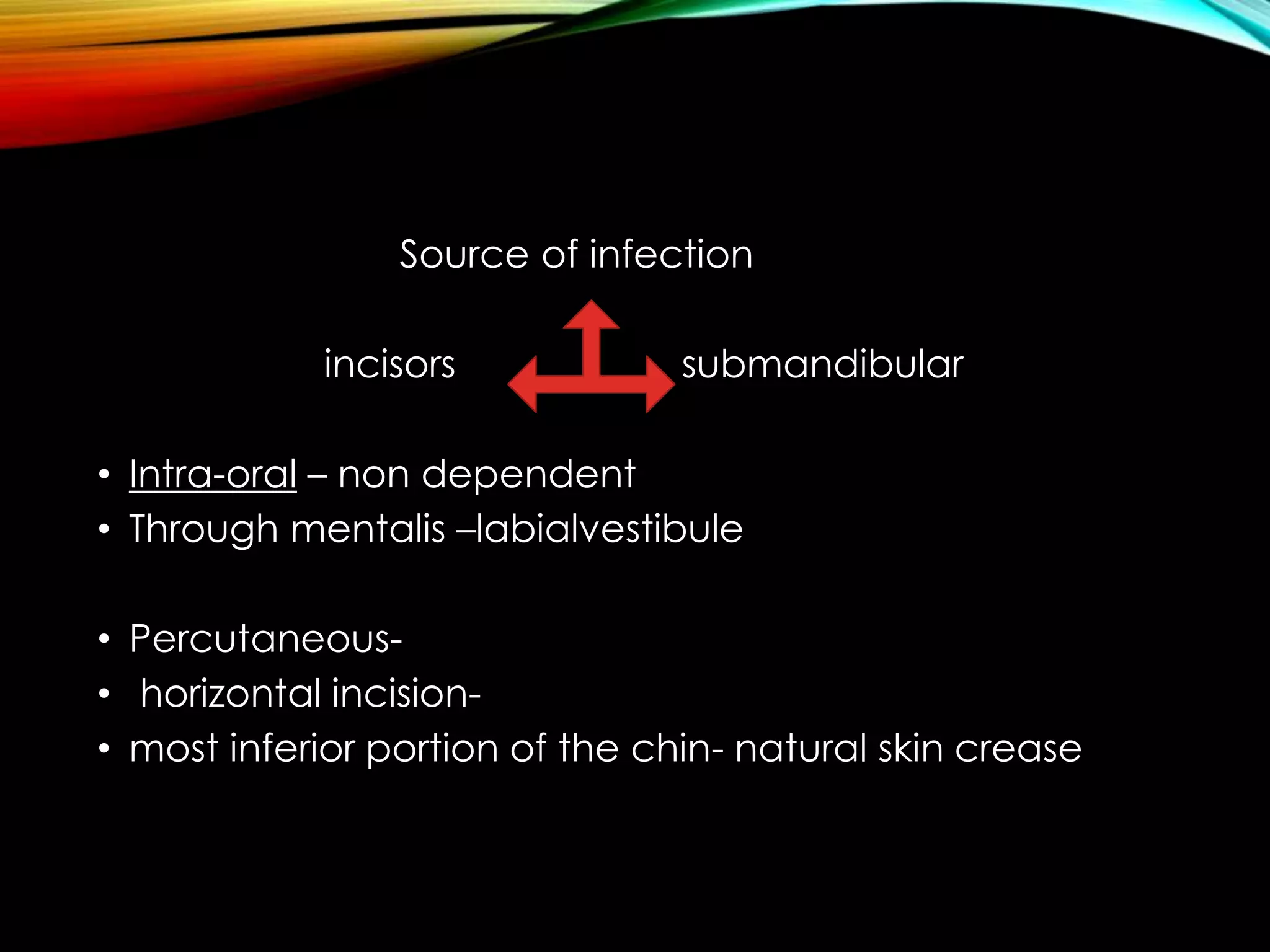
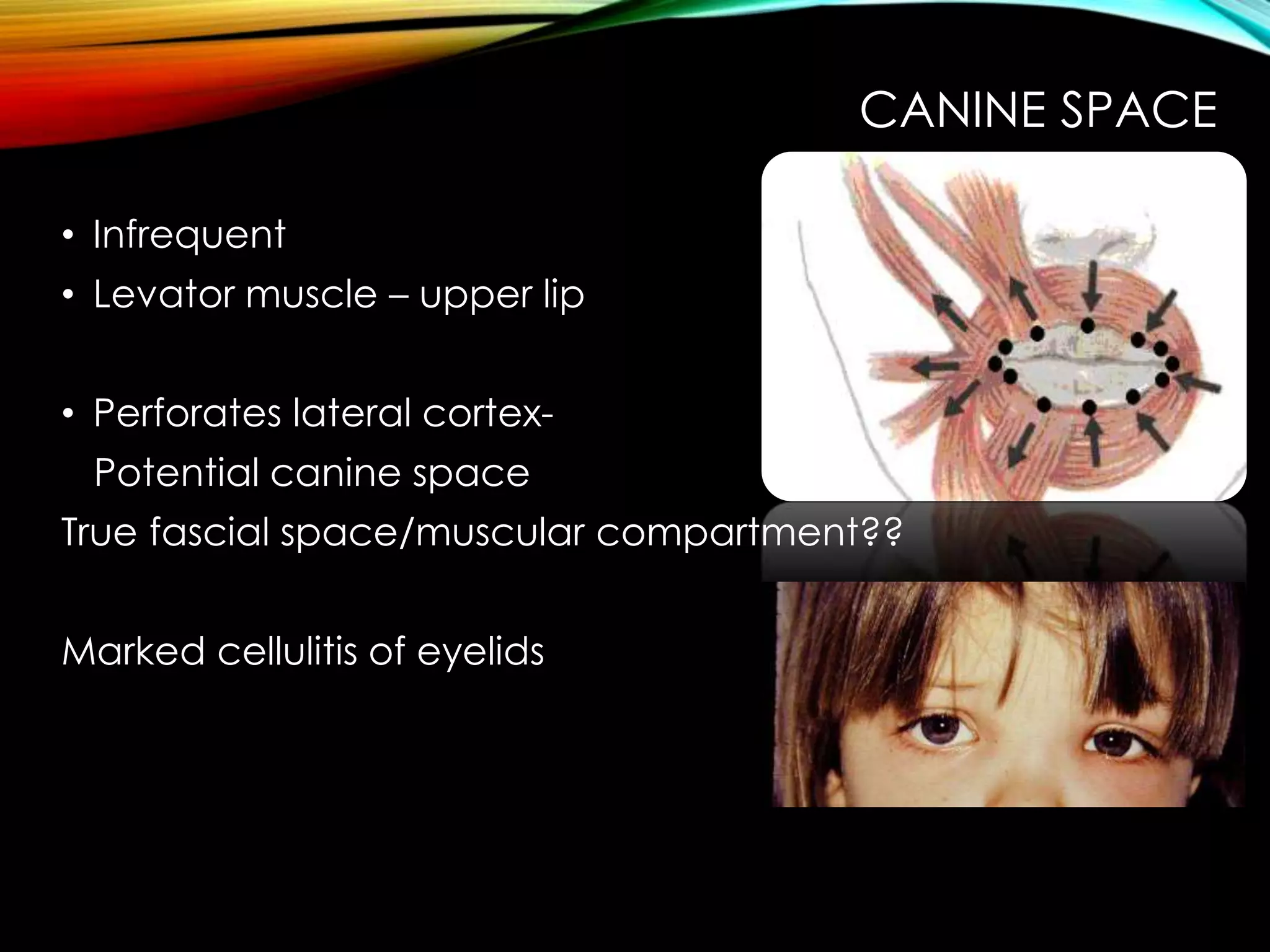
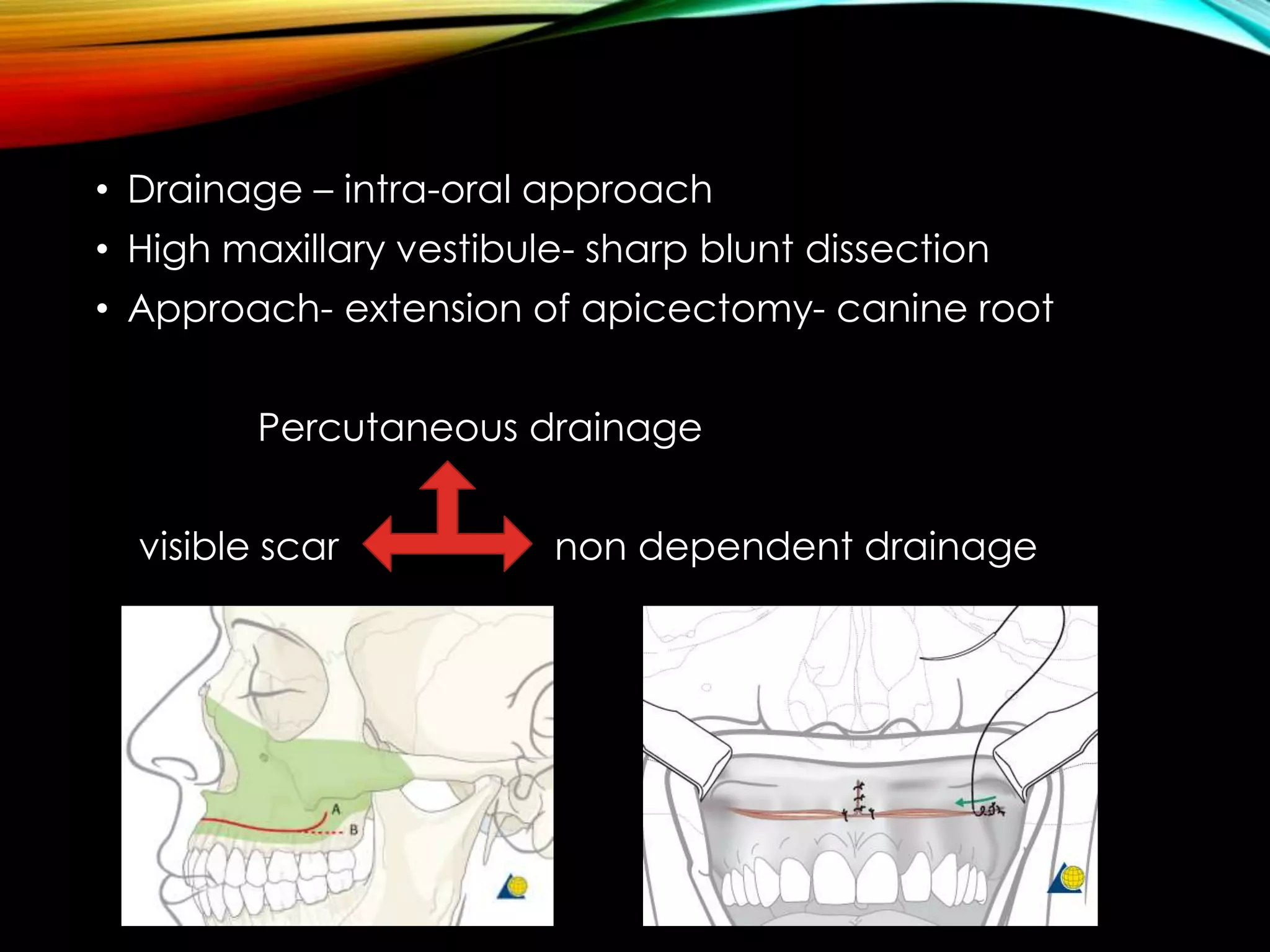
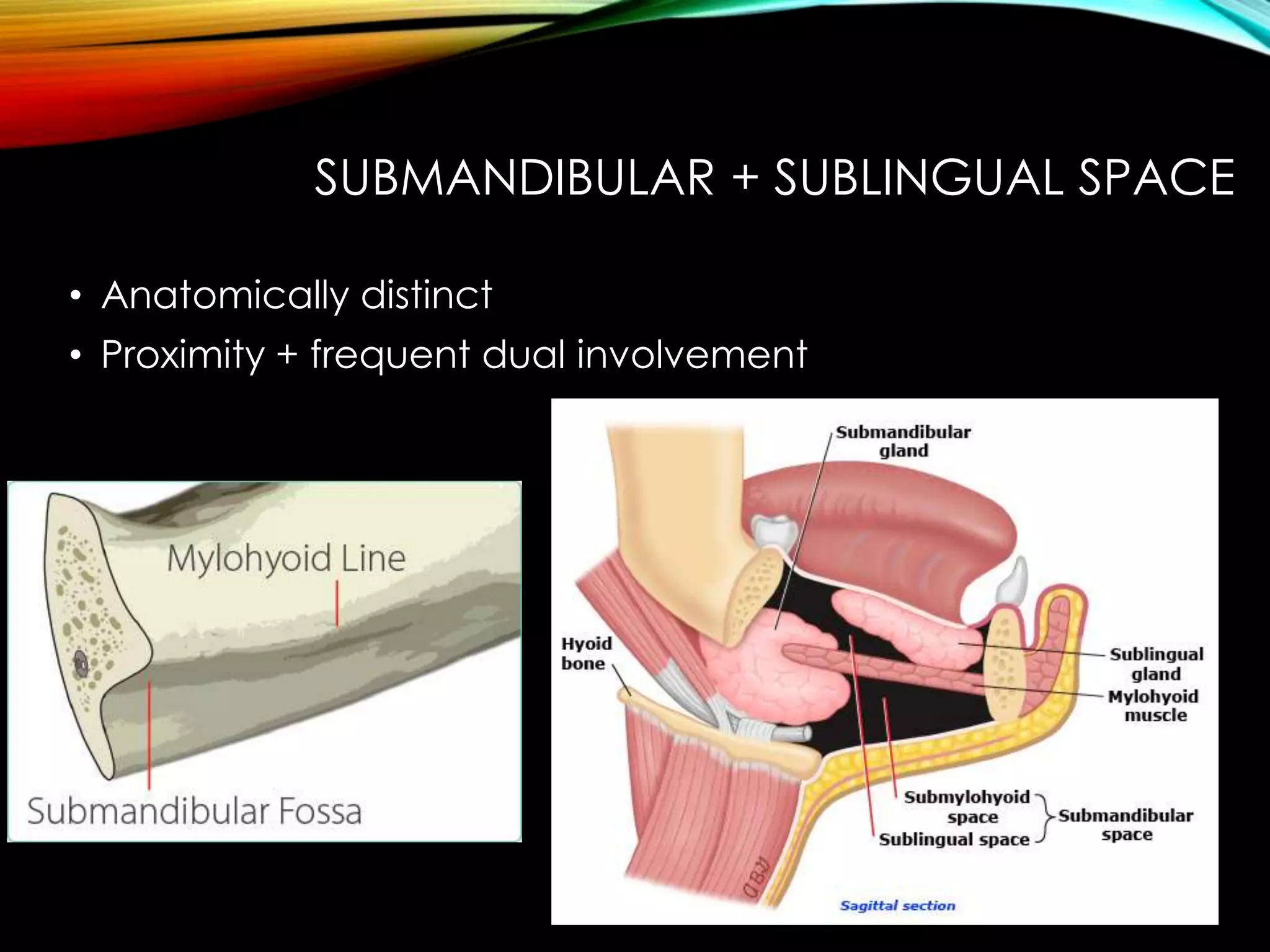
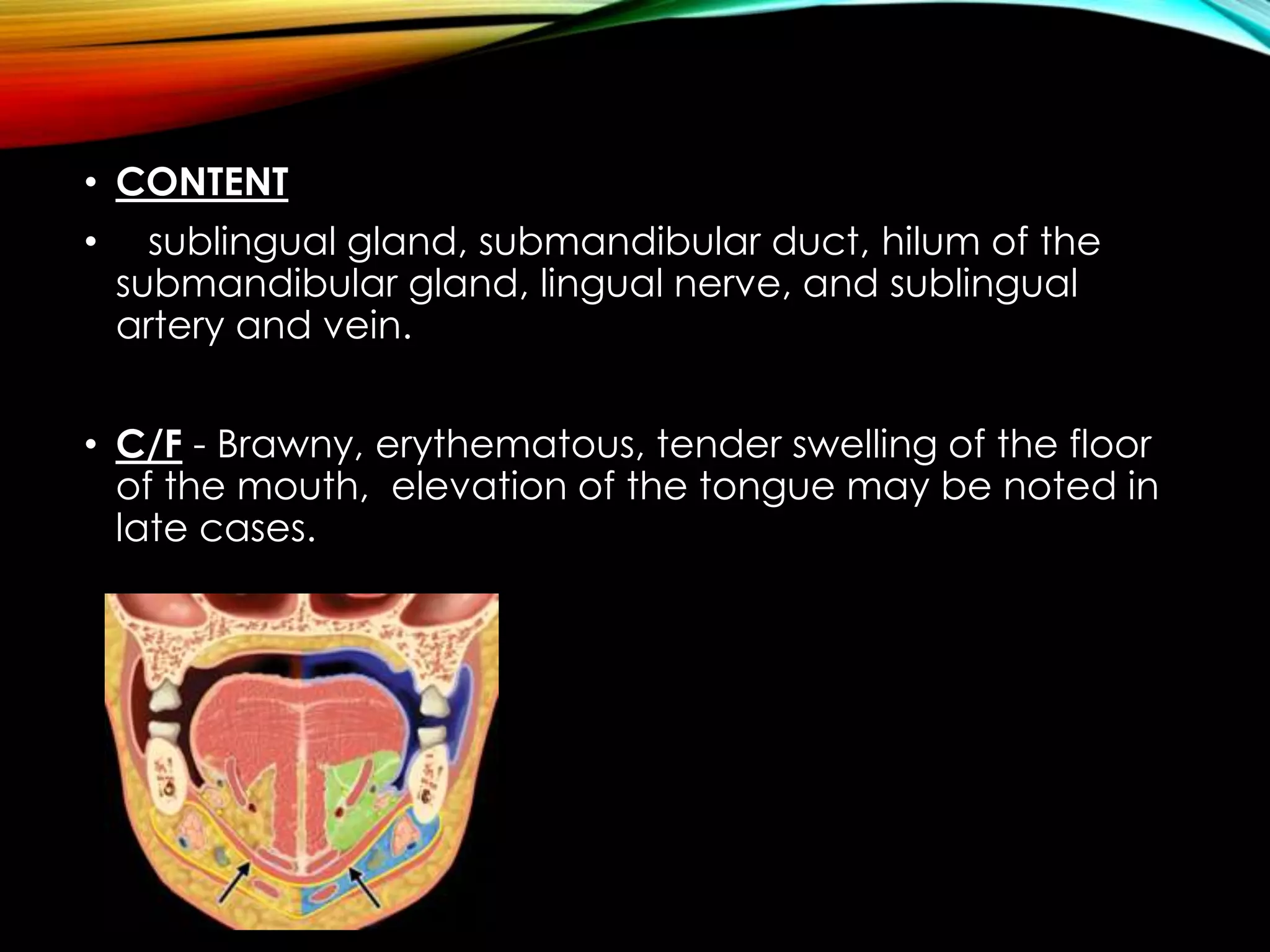
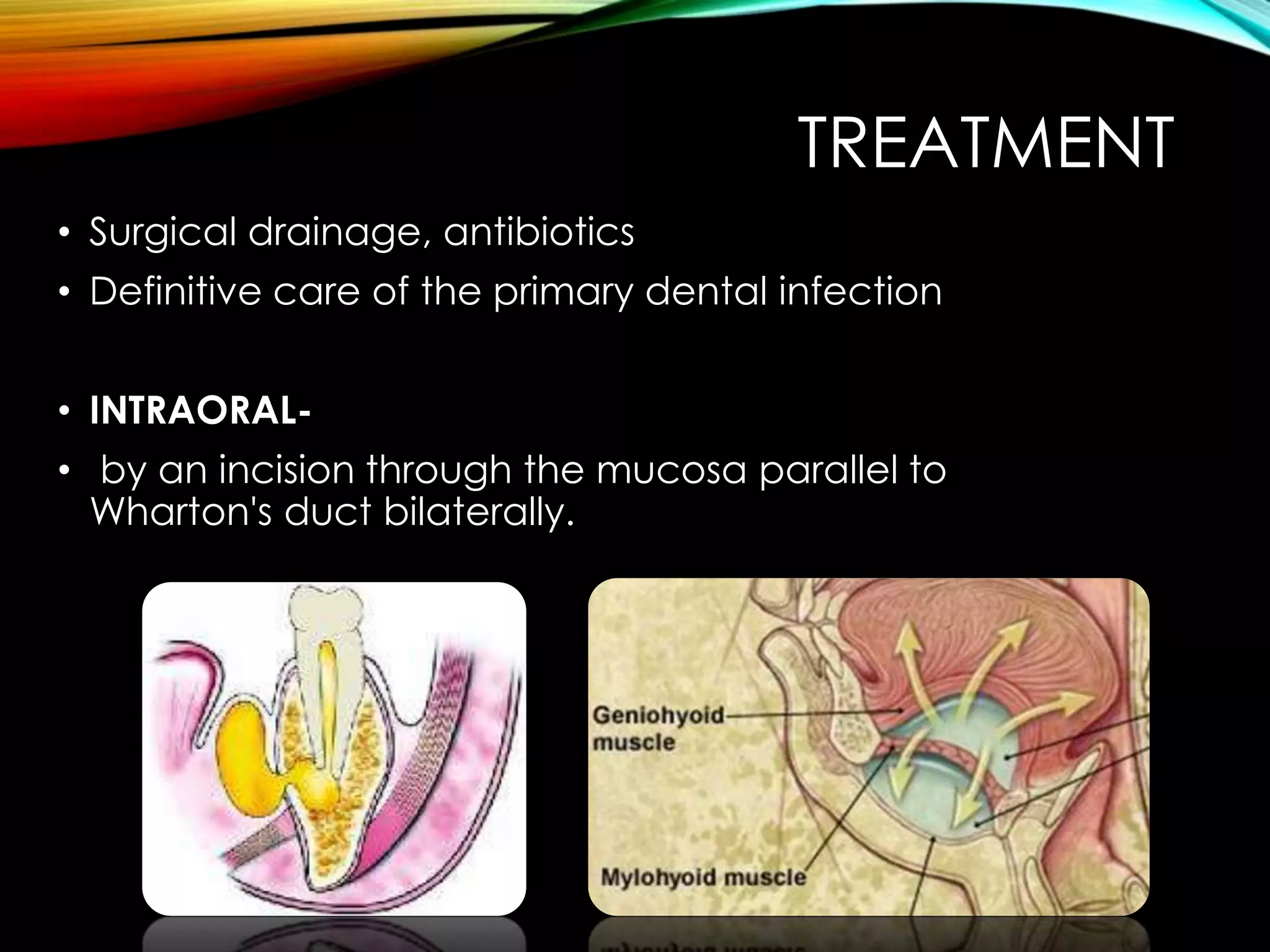
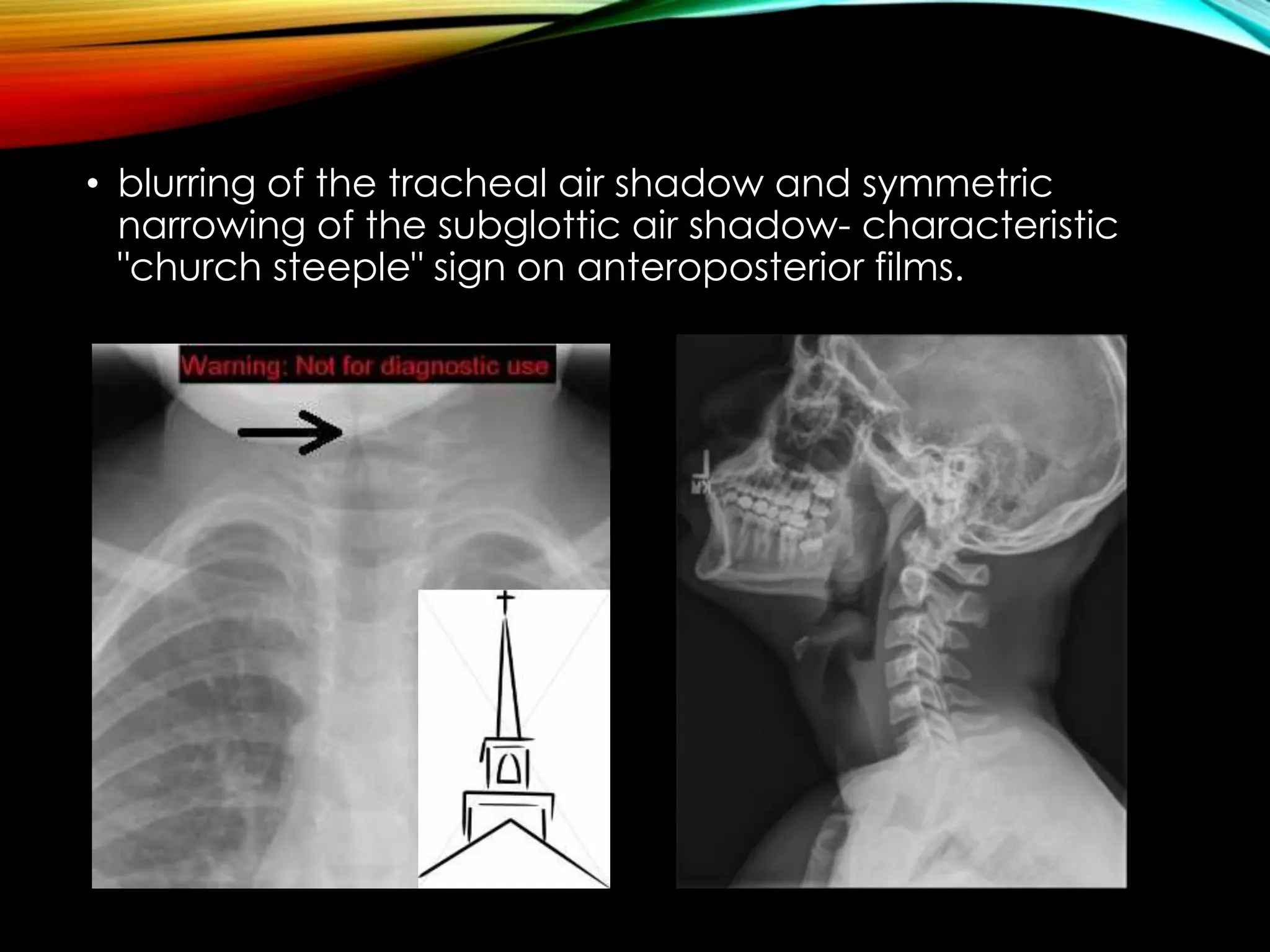
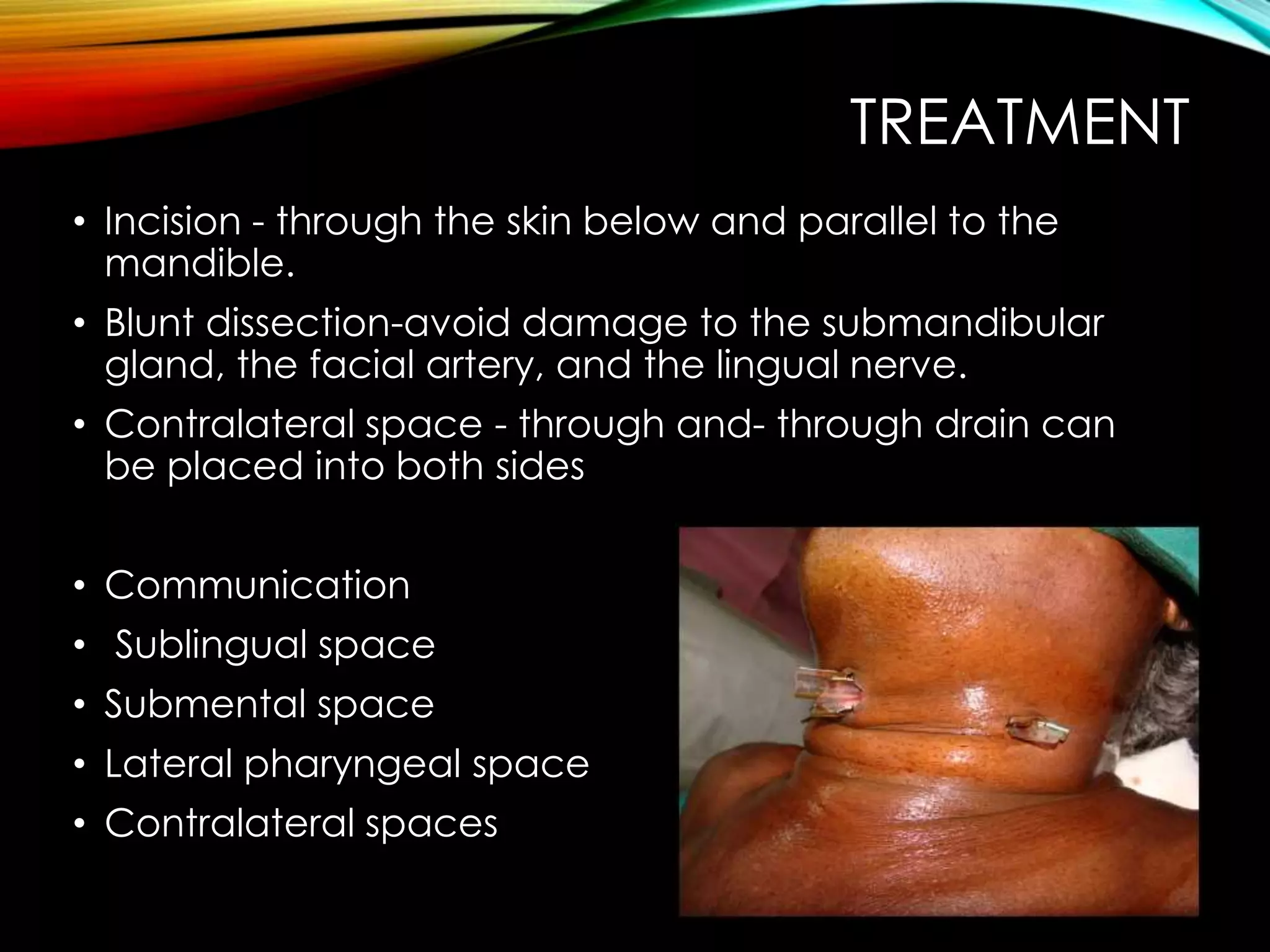
The document discusses deep fascial space infections, including their anatomy, classification, pathways of spread, diagnostic aids, and treatment. It describes several key fascial spaces of the face and neck that are clinically significant for odontogenic infections, such as the buccal, submandibular, sublingual, and submental spaces. Signs and symptoms, as well as surgical drainage techniques for managing infections in these different spaces are outlined.