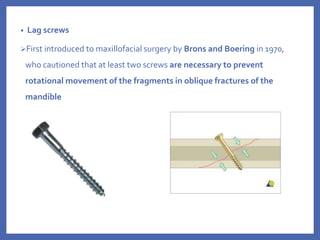
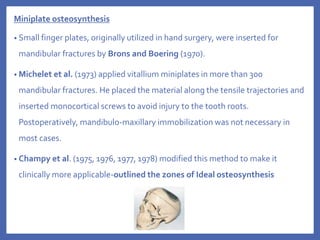
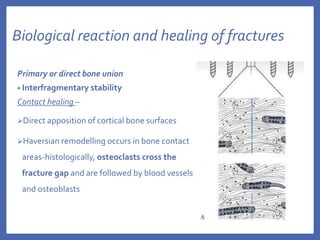
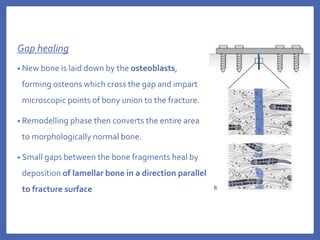
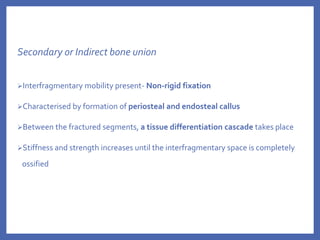
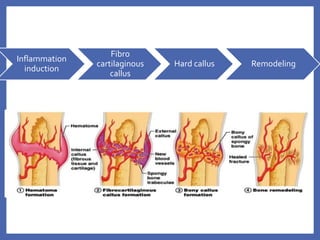
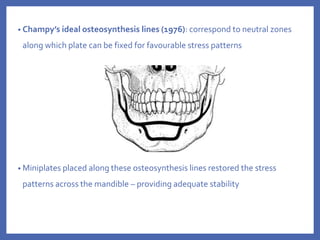
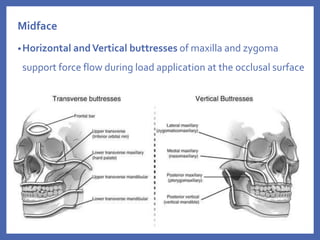
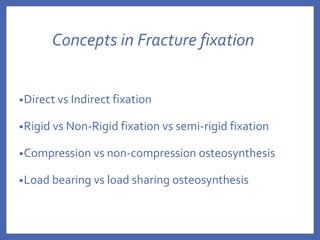
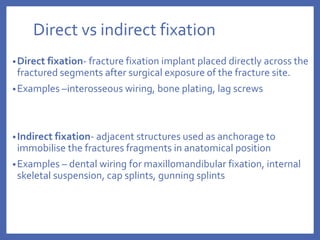
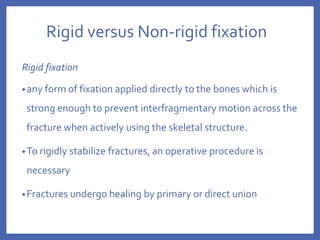
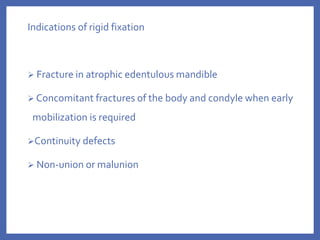
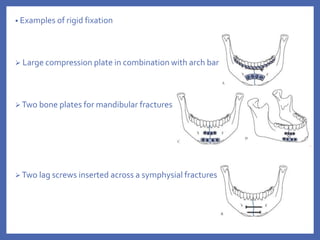
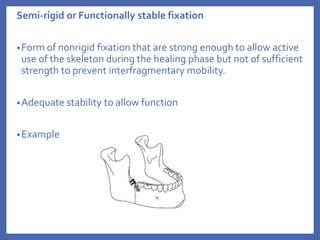
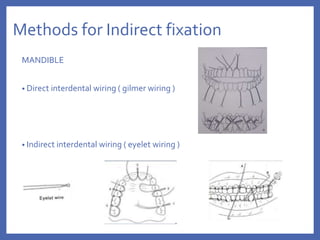
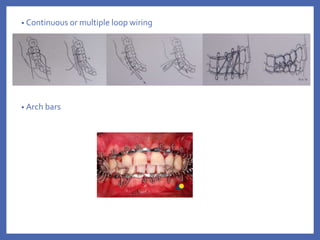
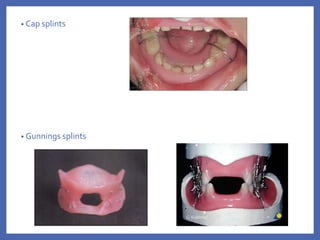
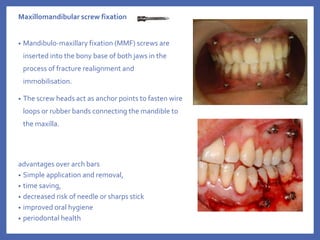
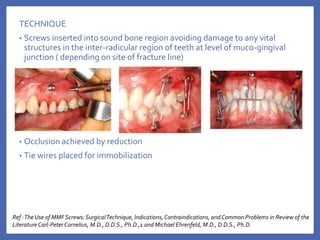
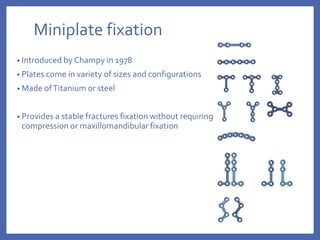
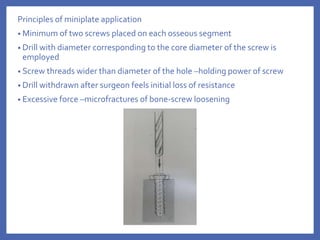
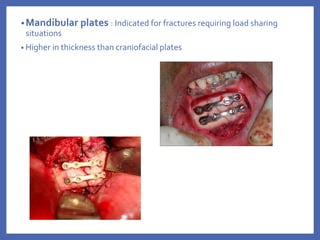
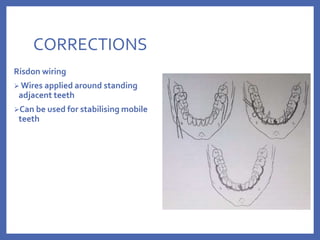
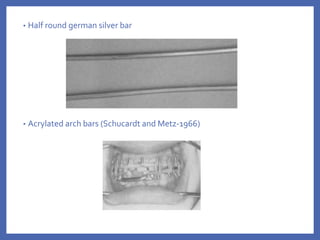
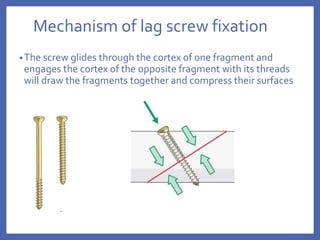
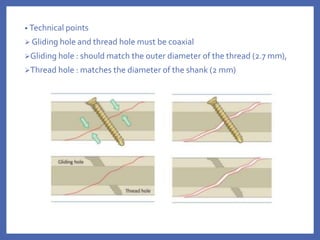
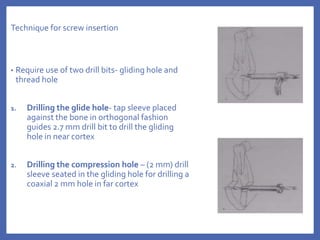
The document provides a comprehensive overview of fixation systems used in maxillofacial fractures, detailing their historical development, biological responses, and biomechanics. It discusses various concepts of fracture fixation, including rigid, non-rigid, and semi-rigid methods, along with specific techniques and advances in fixation systems. Additionally, it addresses the aims of fracture fixation such as restoring anatomical relationships and stabilizing bone fragments for effective healing.