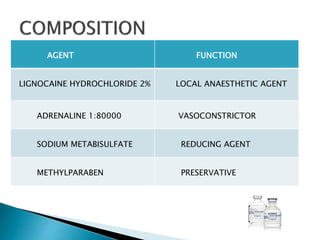
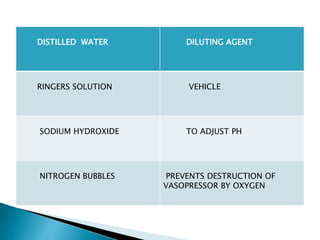
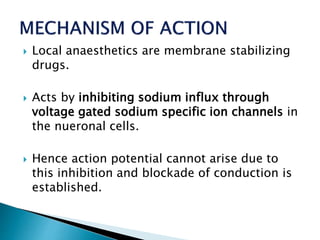
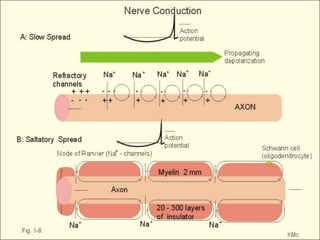
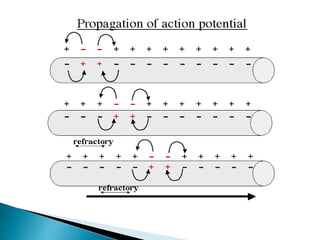
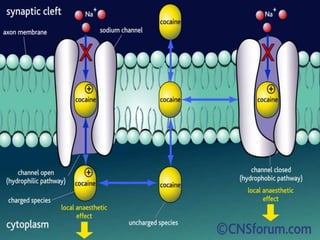
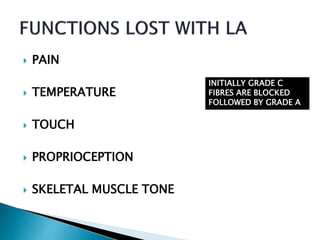
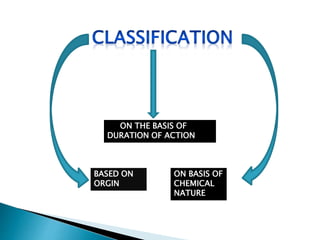
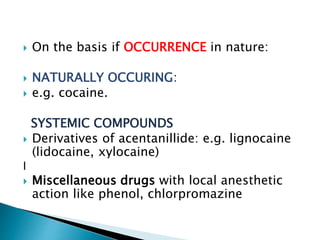
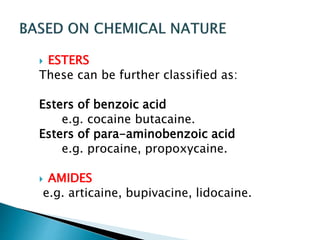
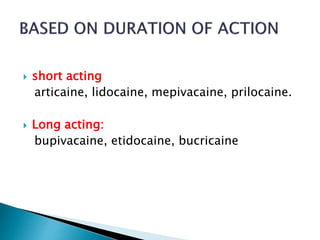
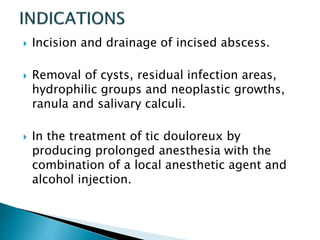
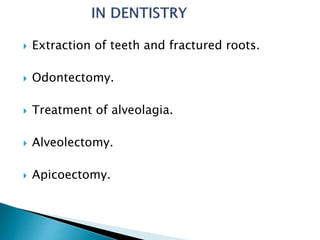
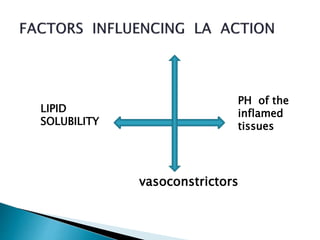
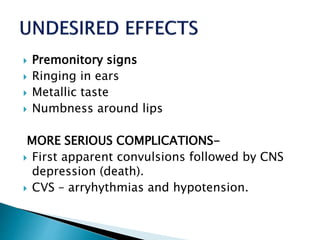
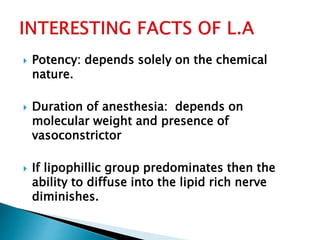
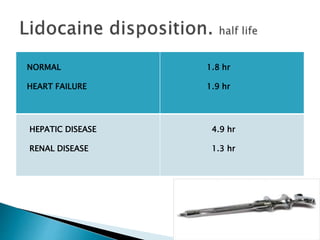
The document discusses local anesthetics, including their definition, requirements, mechanisms of action, classifications, and biotransformation. It notes that local anesthetics work by inhibiting sodium influx through voltage-gated sodium channels in neuronal cells, blocking nerve conduction. Local anesthetics are classified based on duration of action, chemical nature, and origin. Common examples are discussed and appropriate uses along with potential complications and contraindications are outlined.