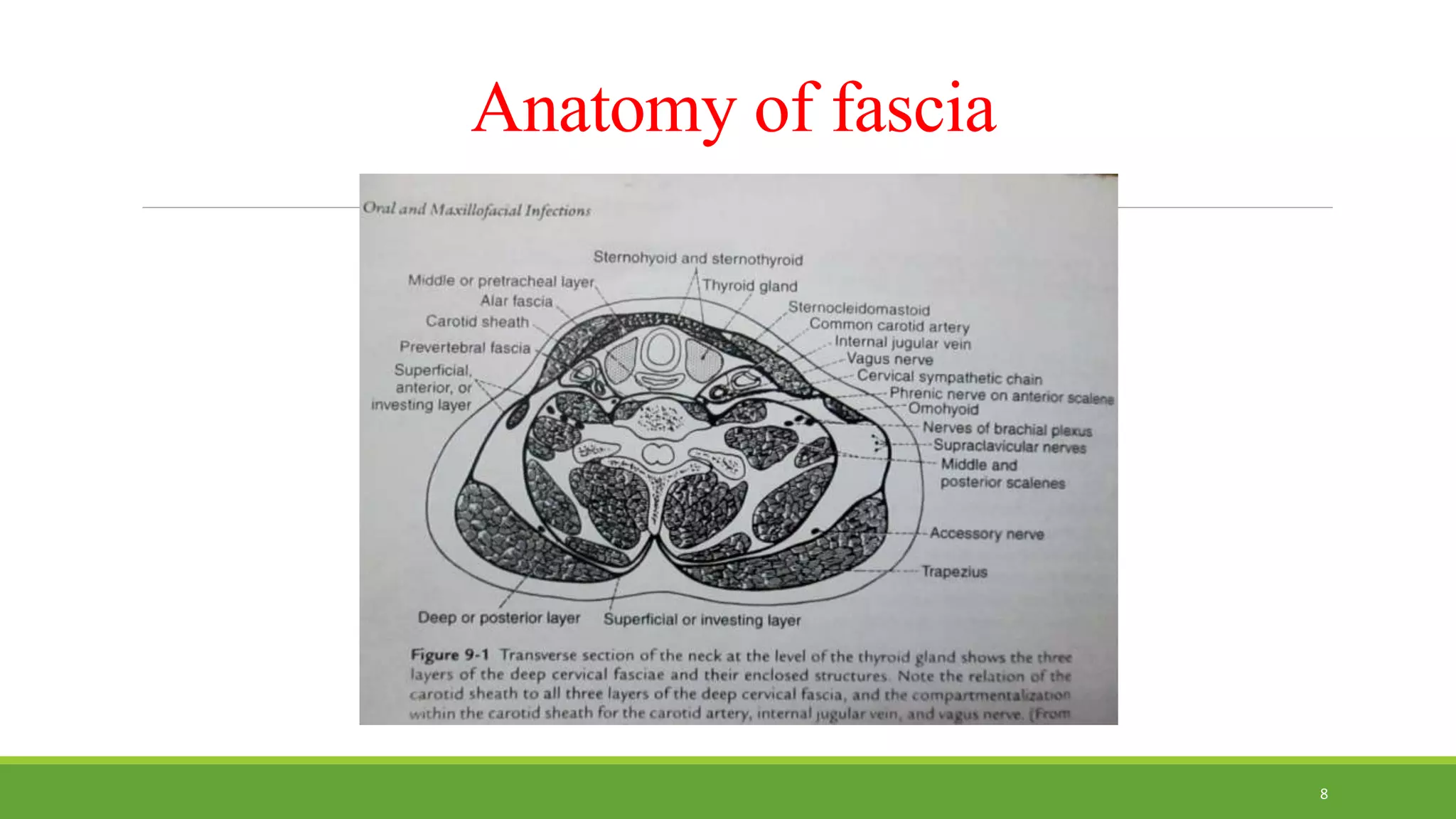
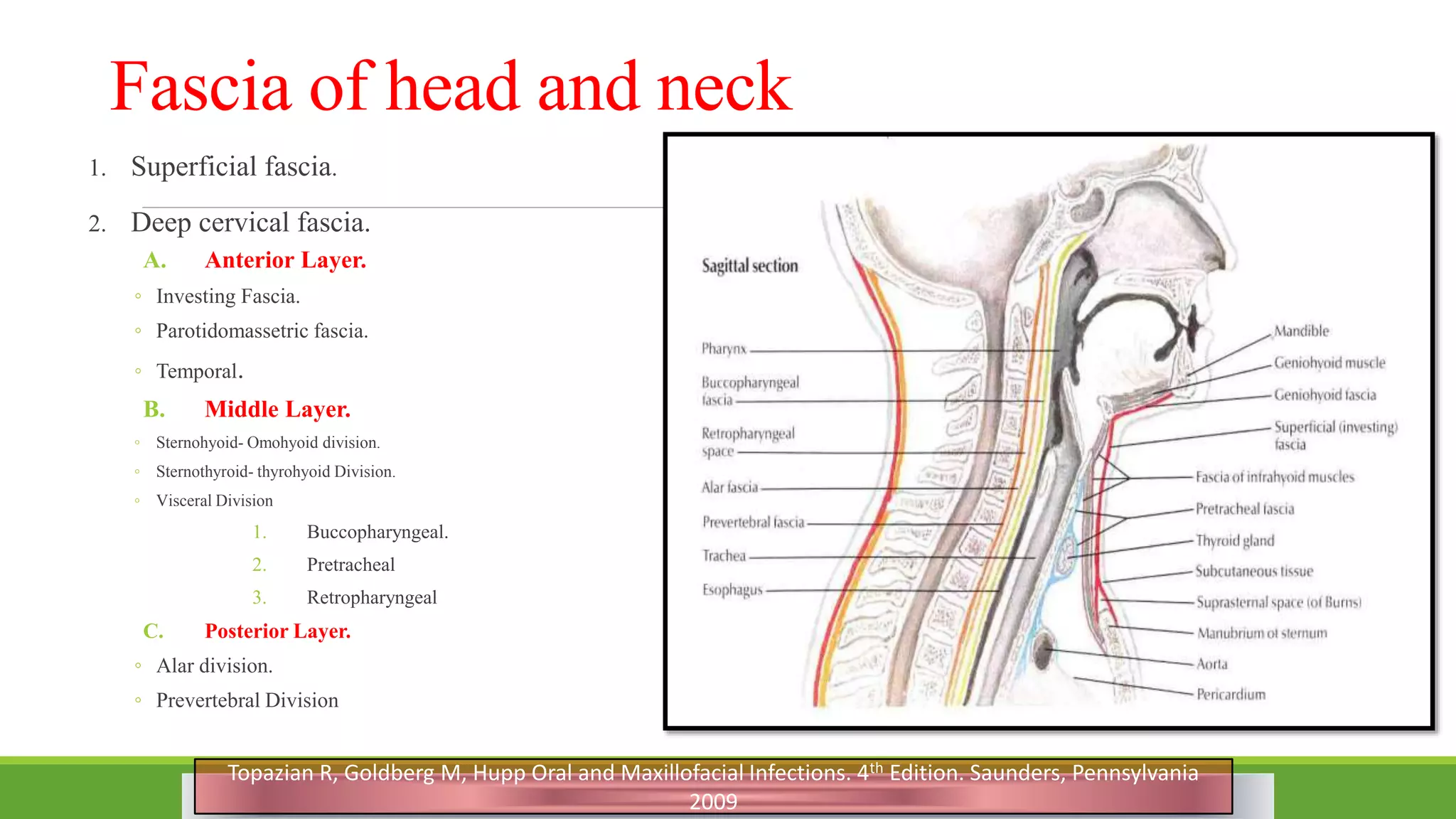
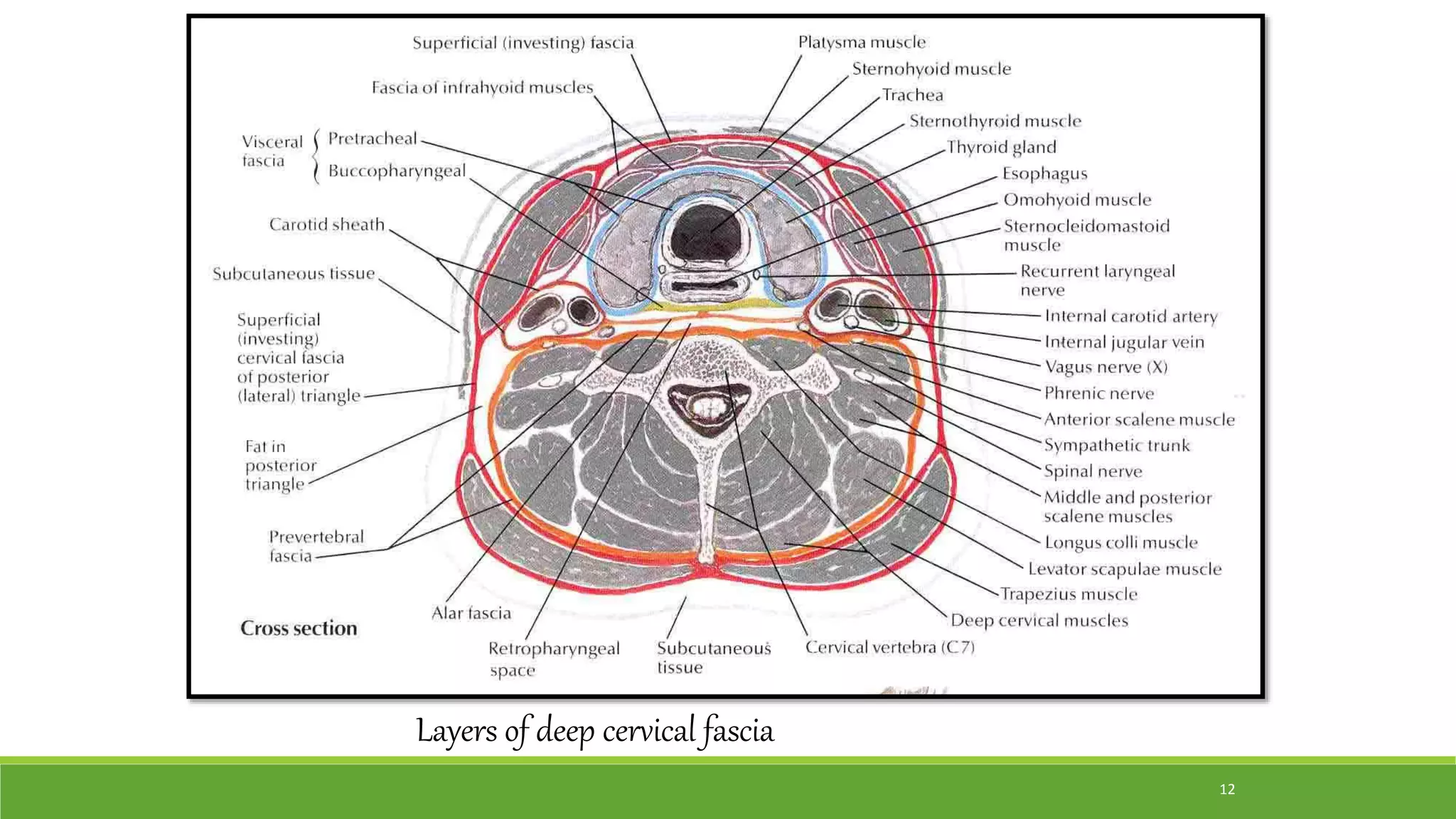
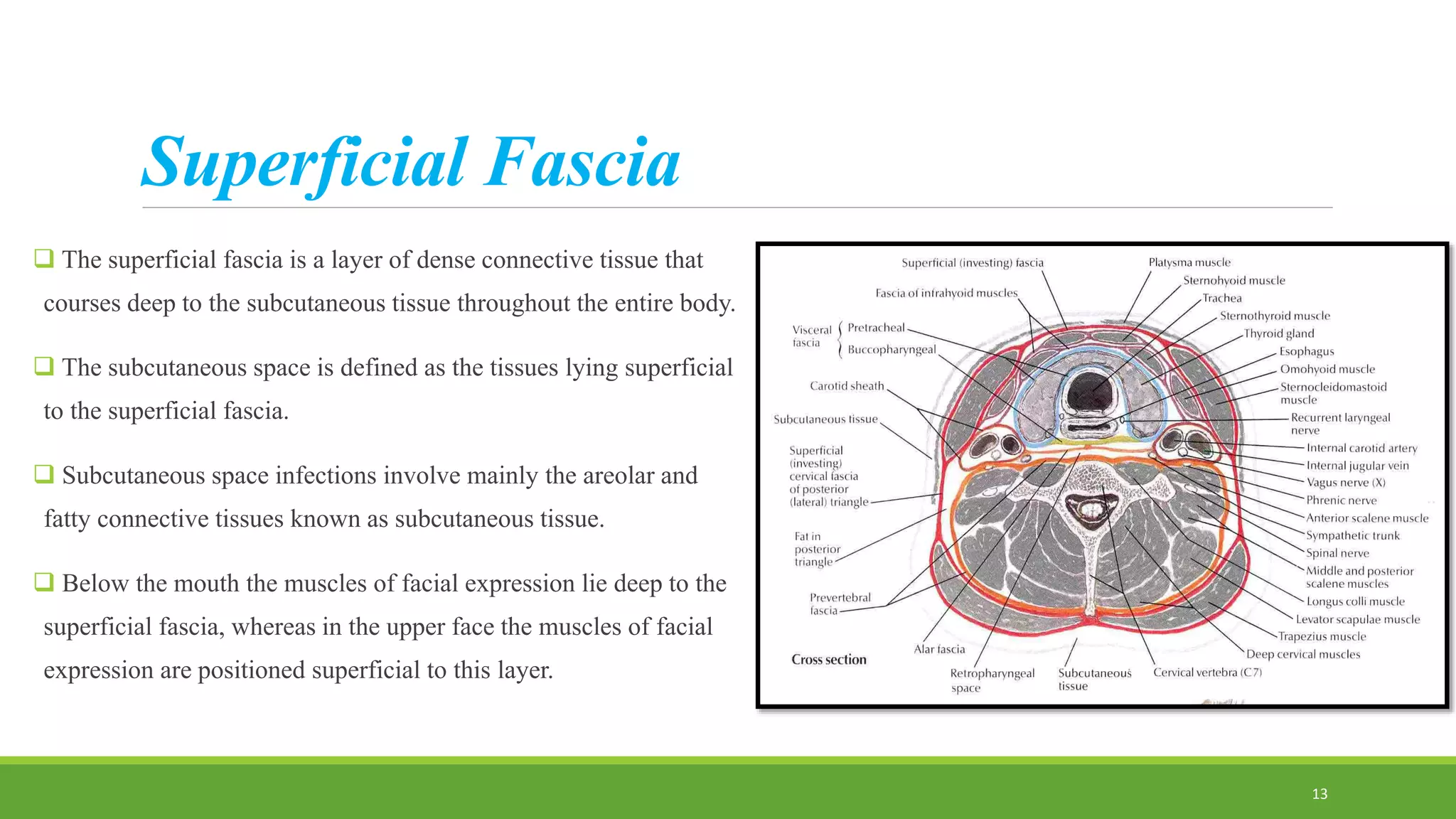
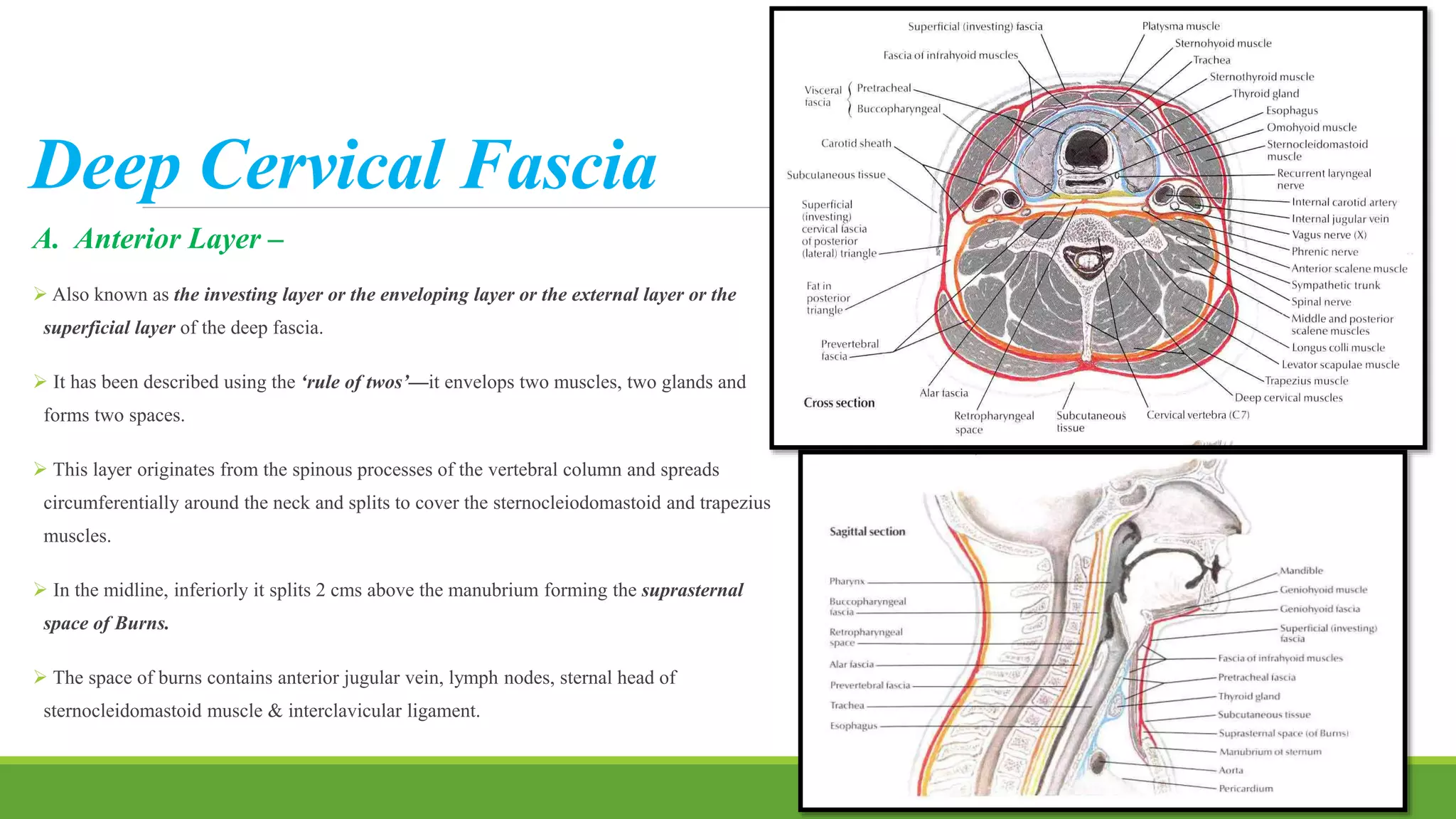
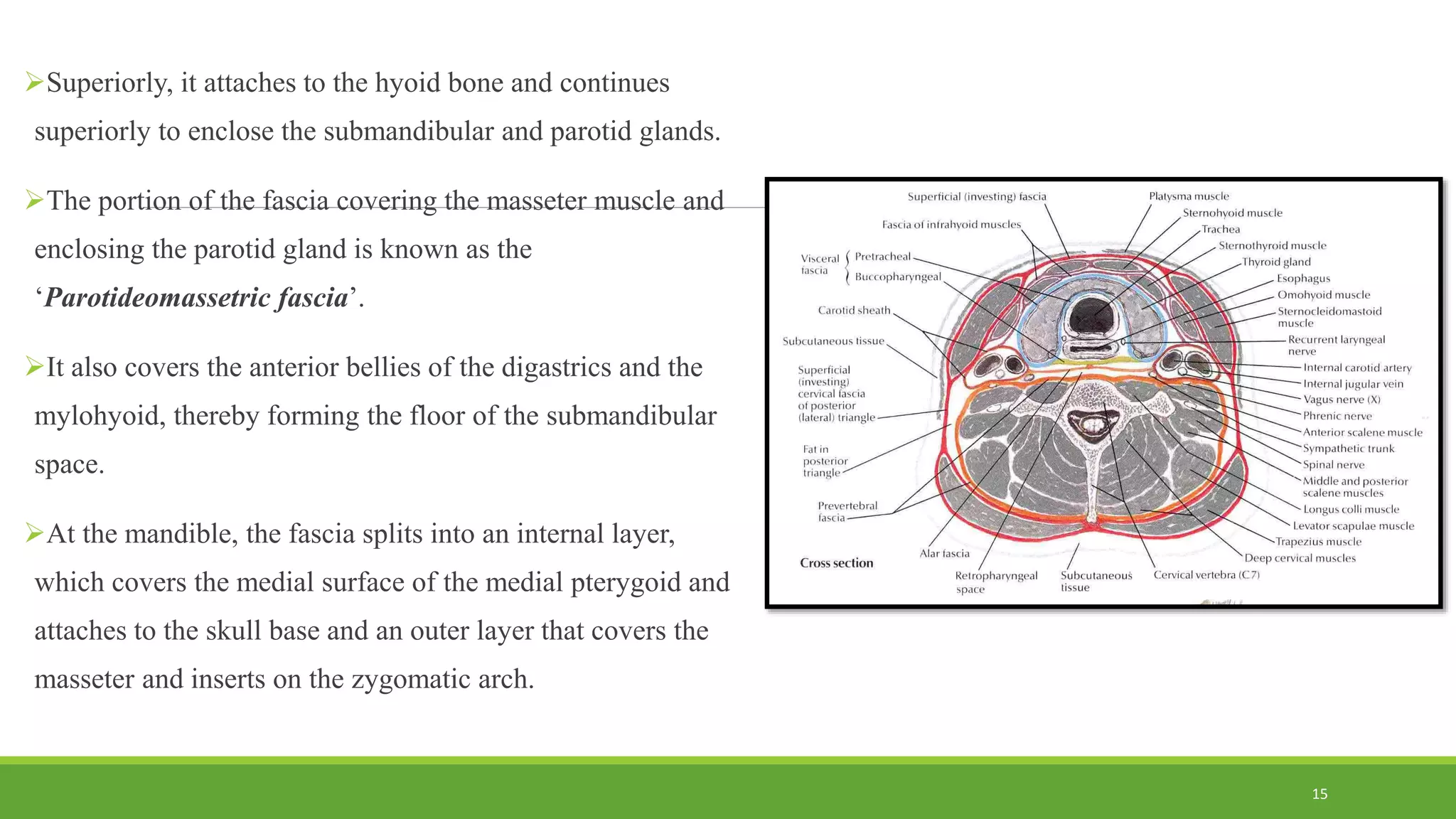
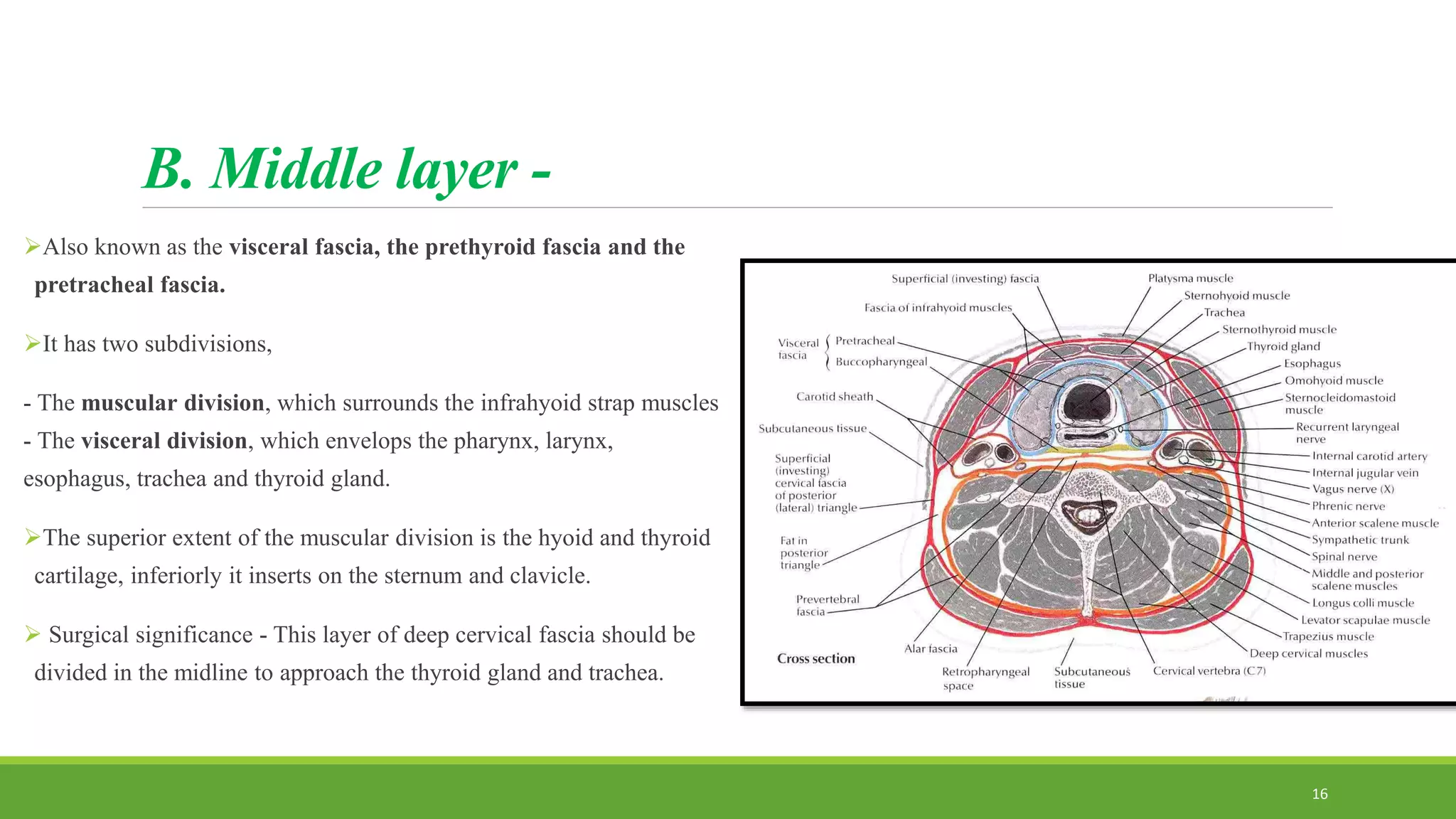
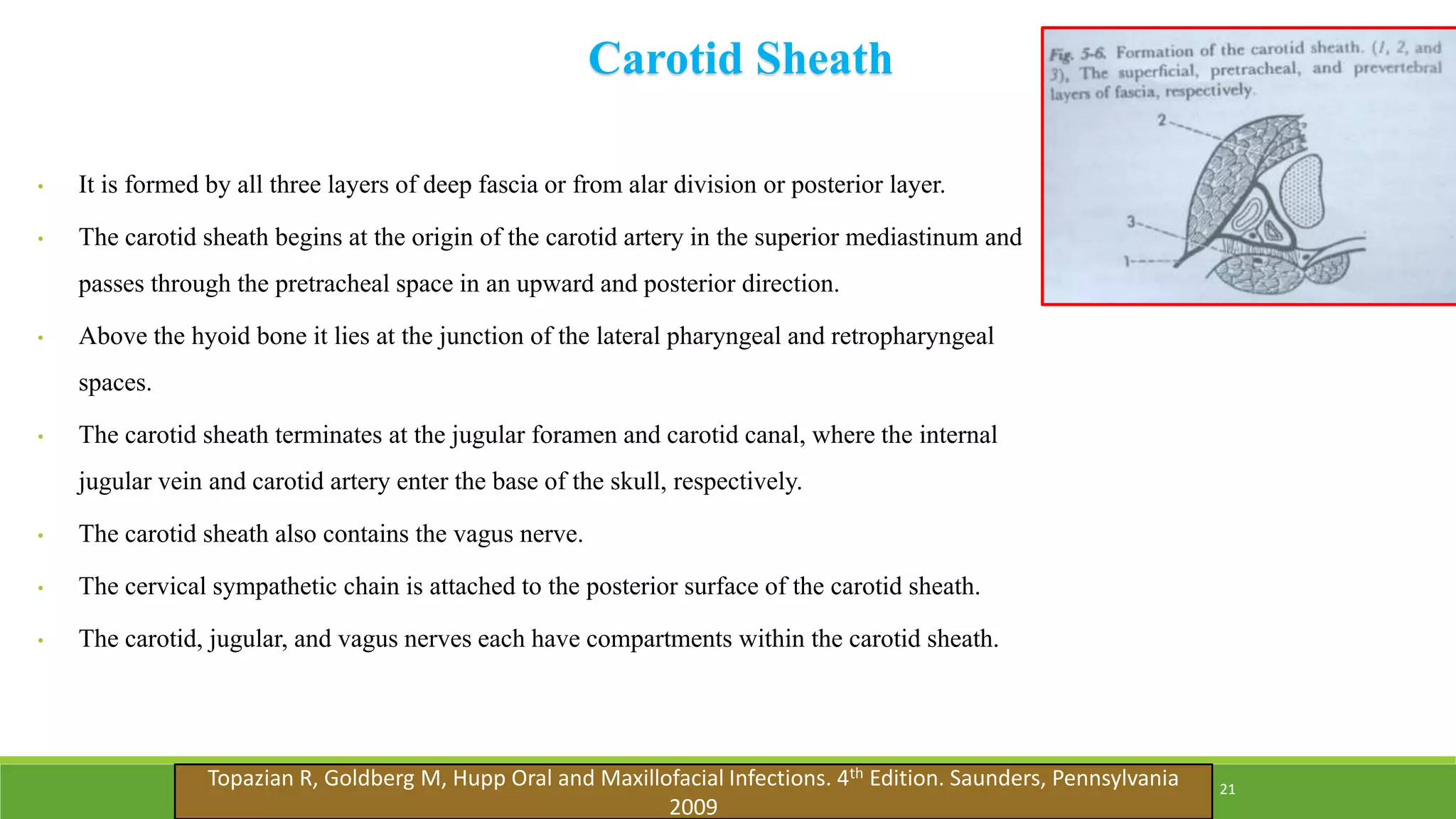
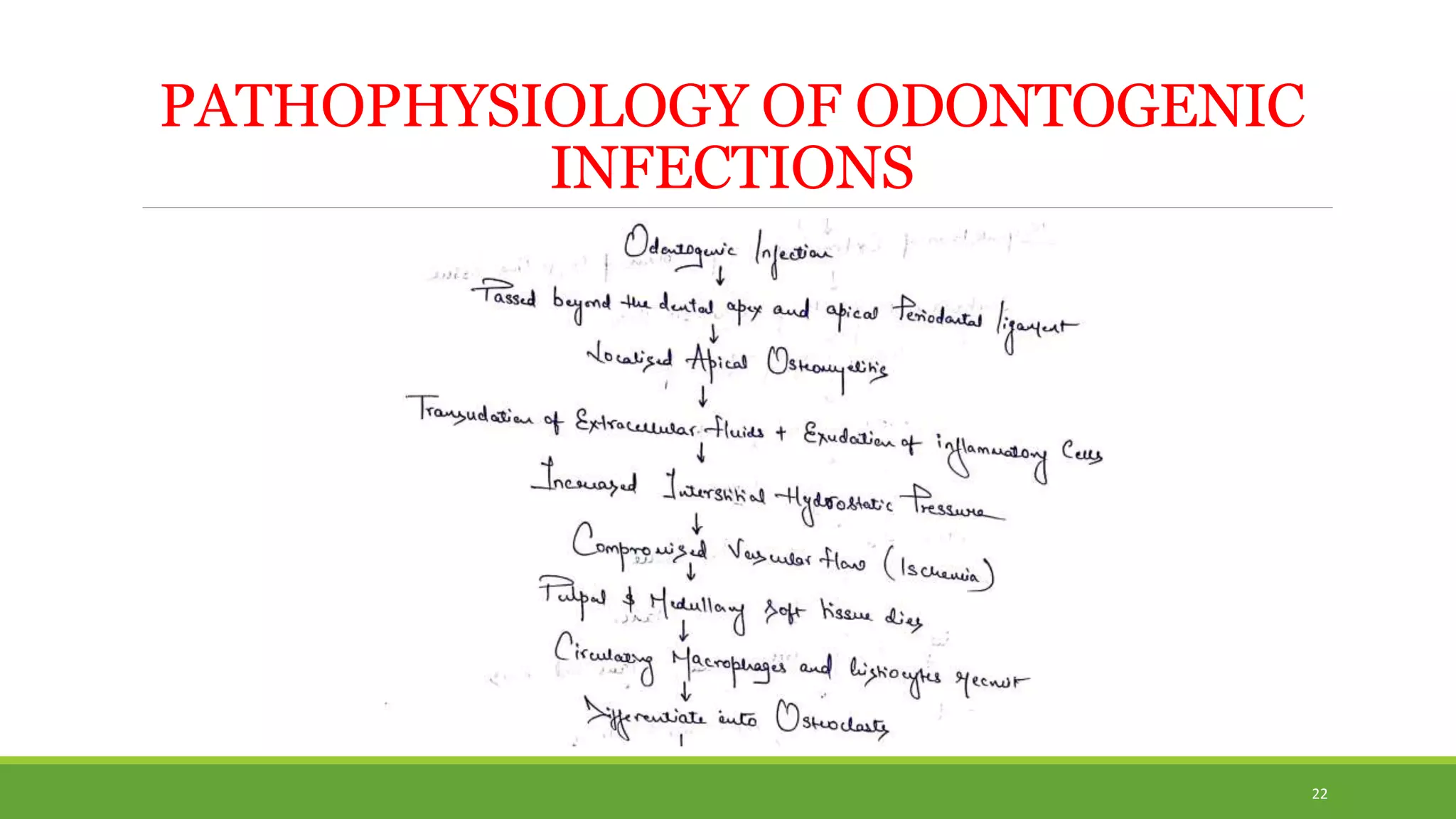
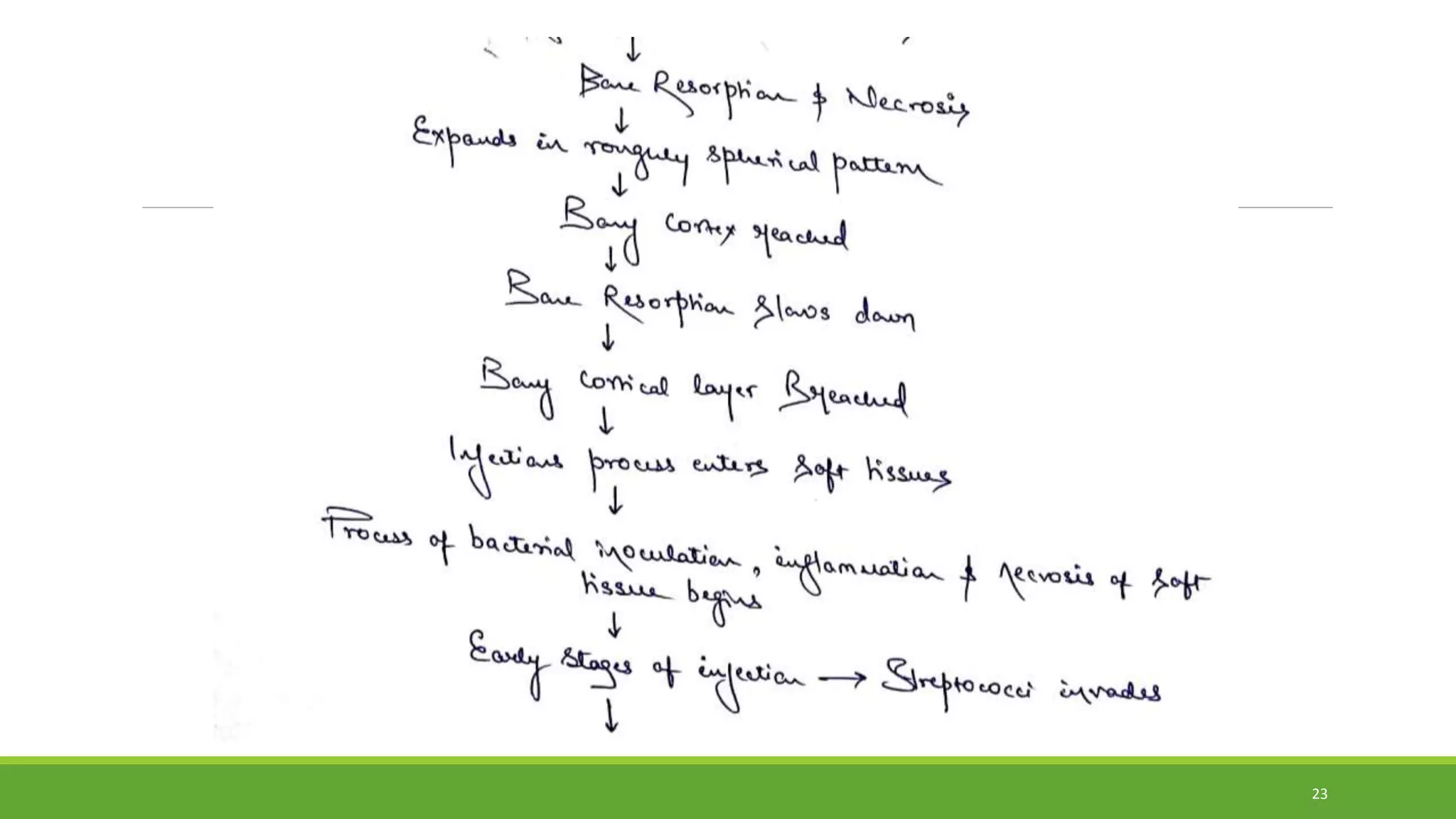
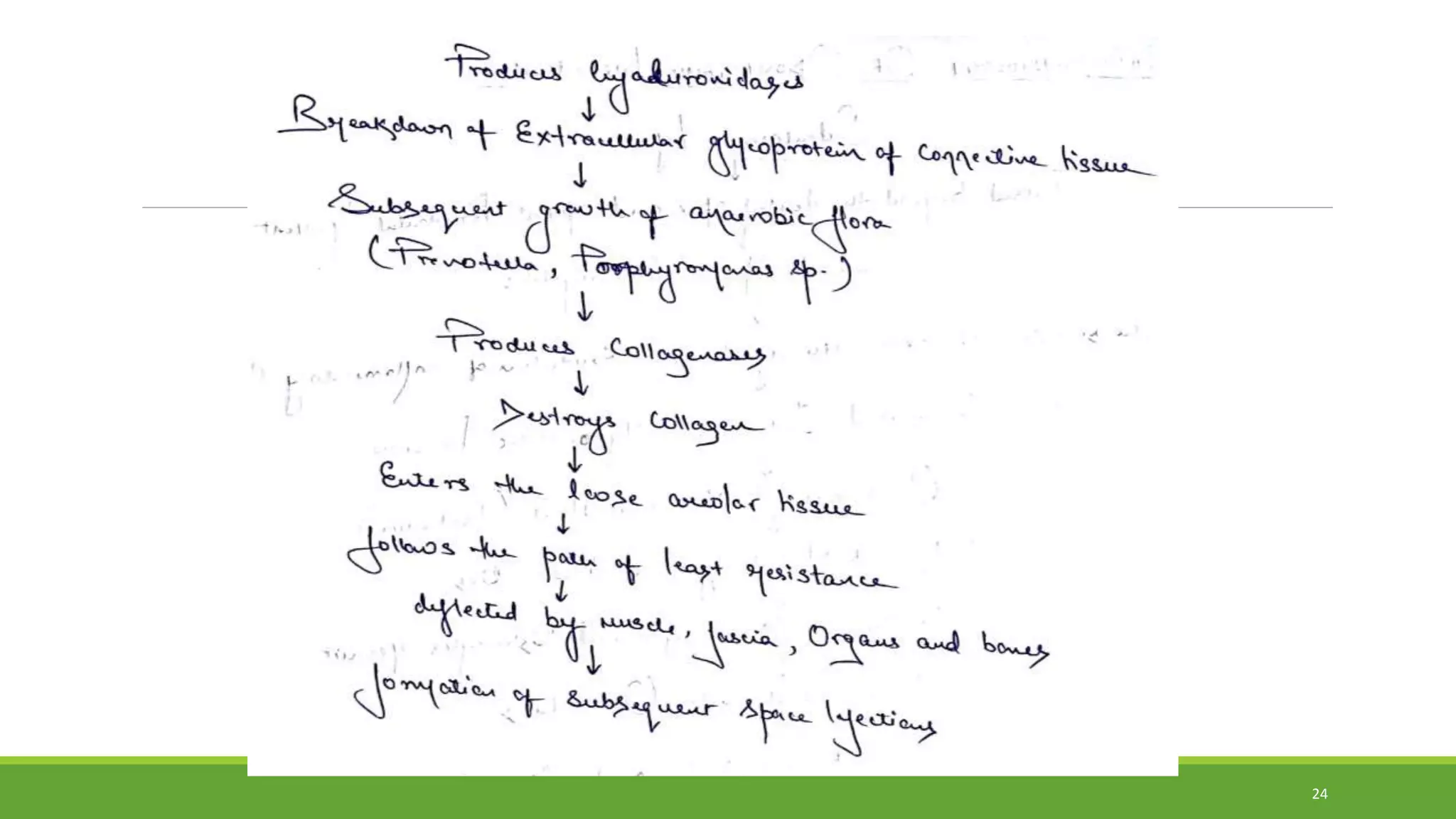
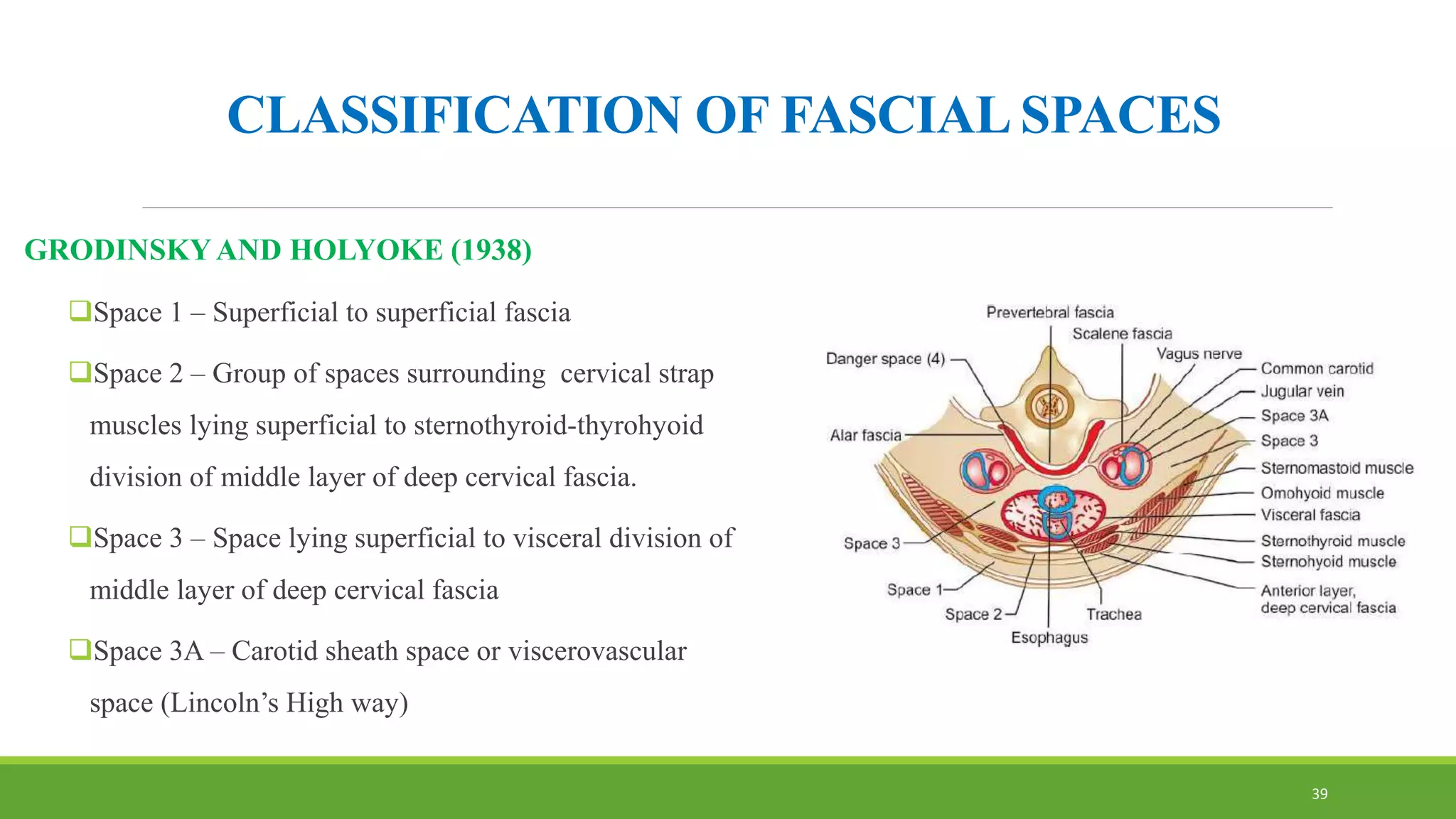
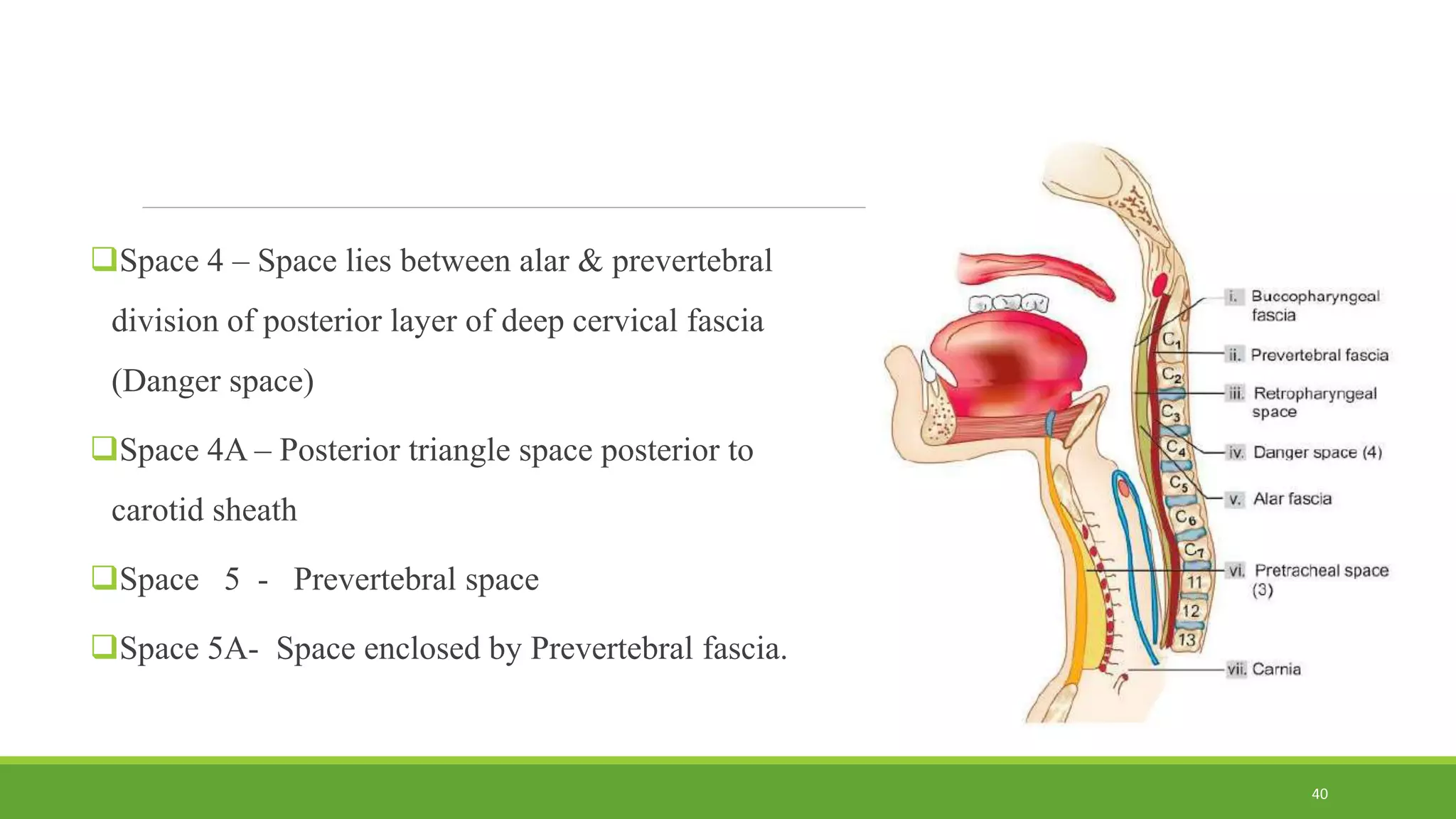
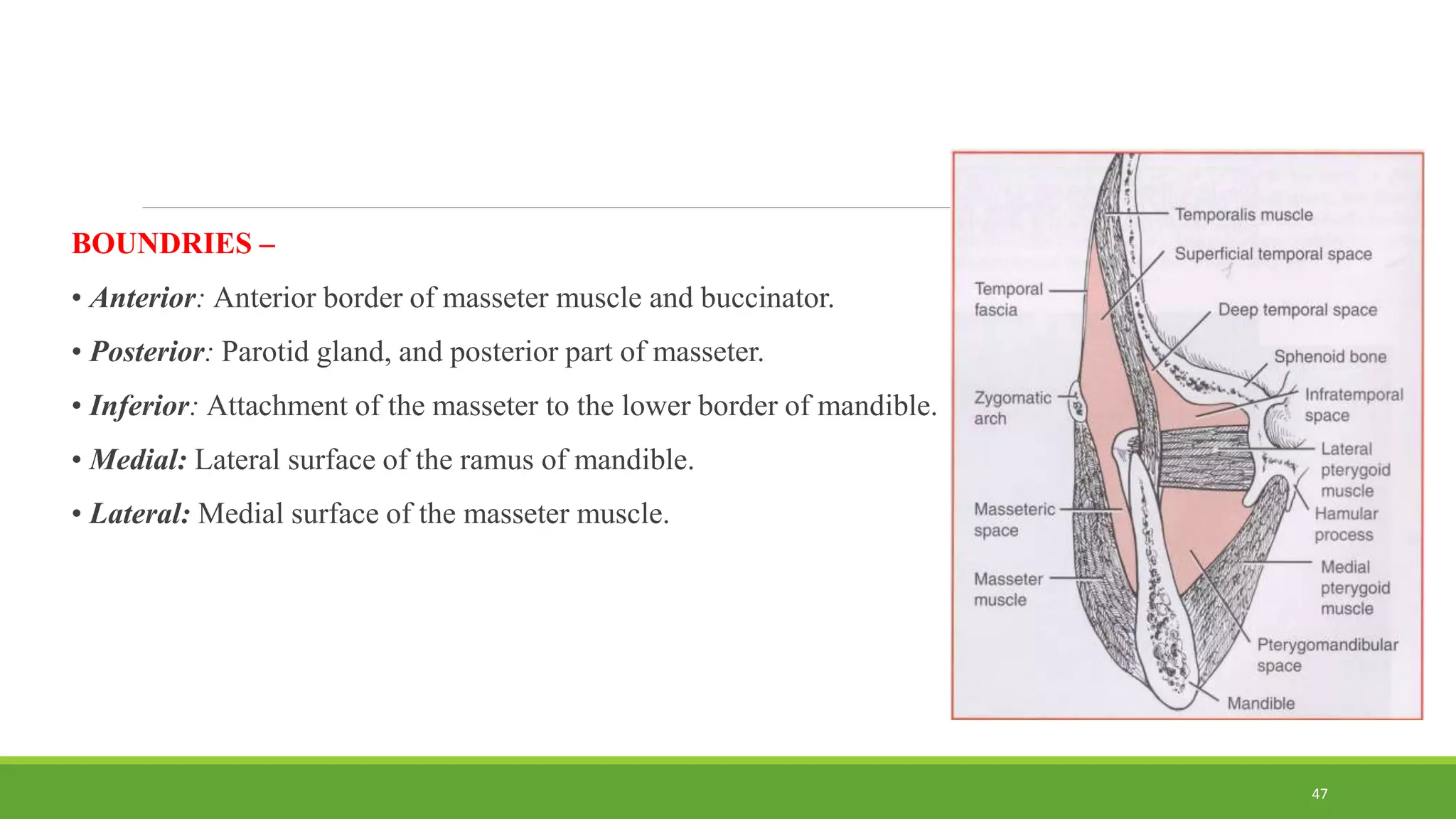
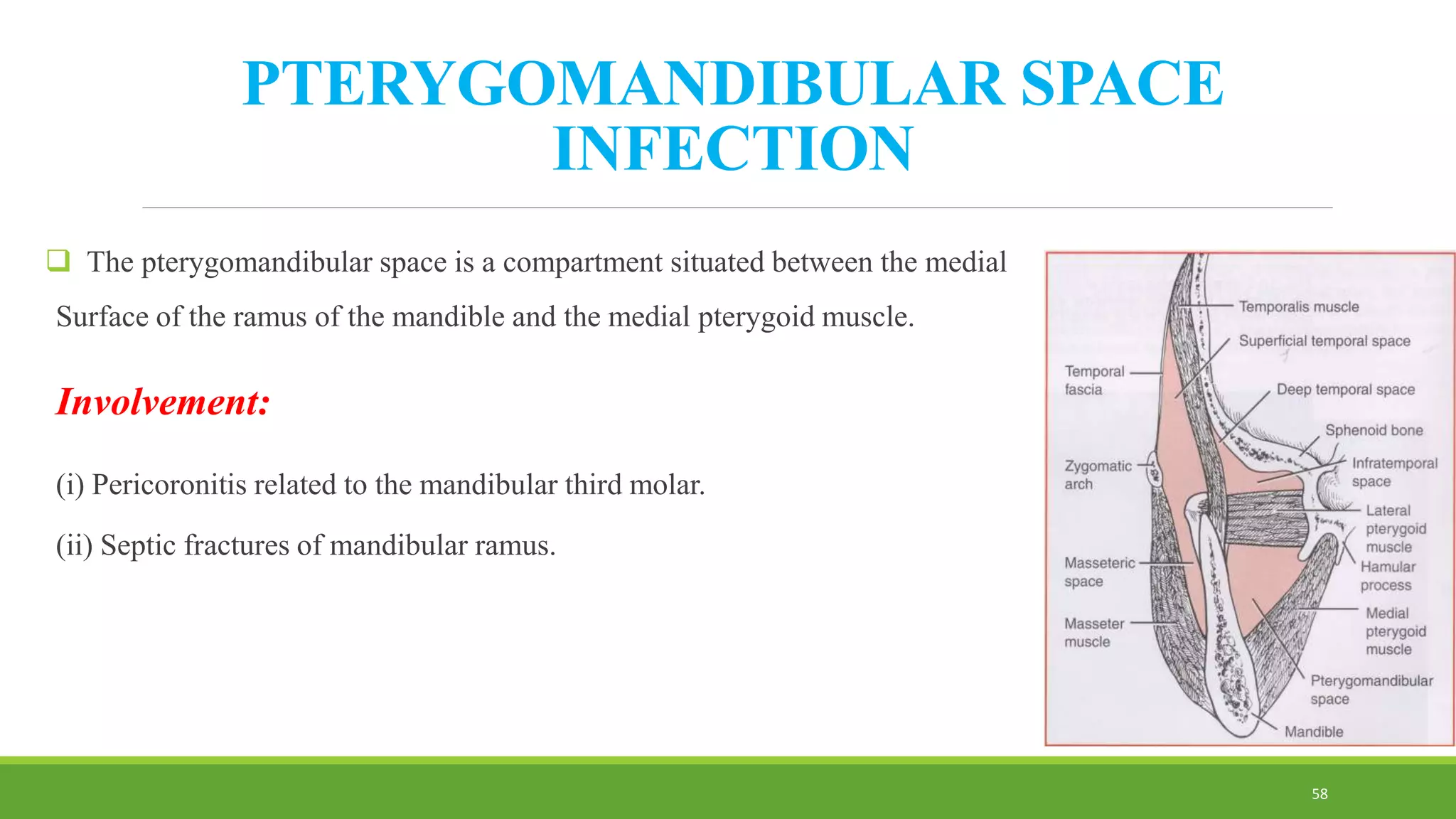
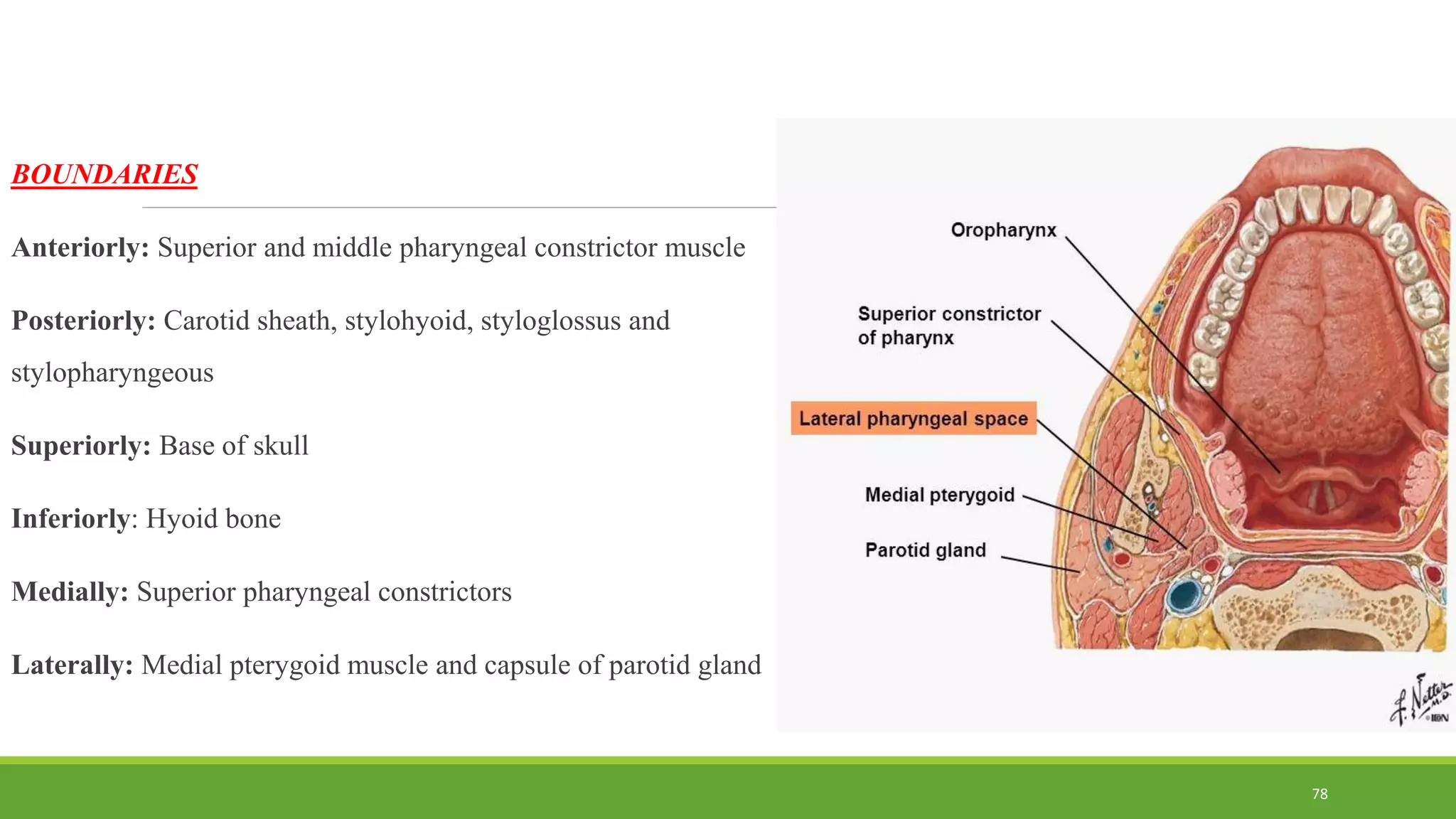
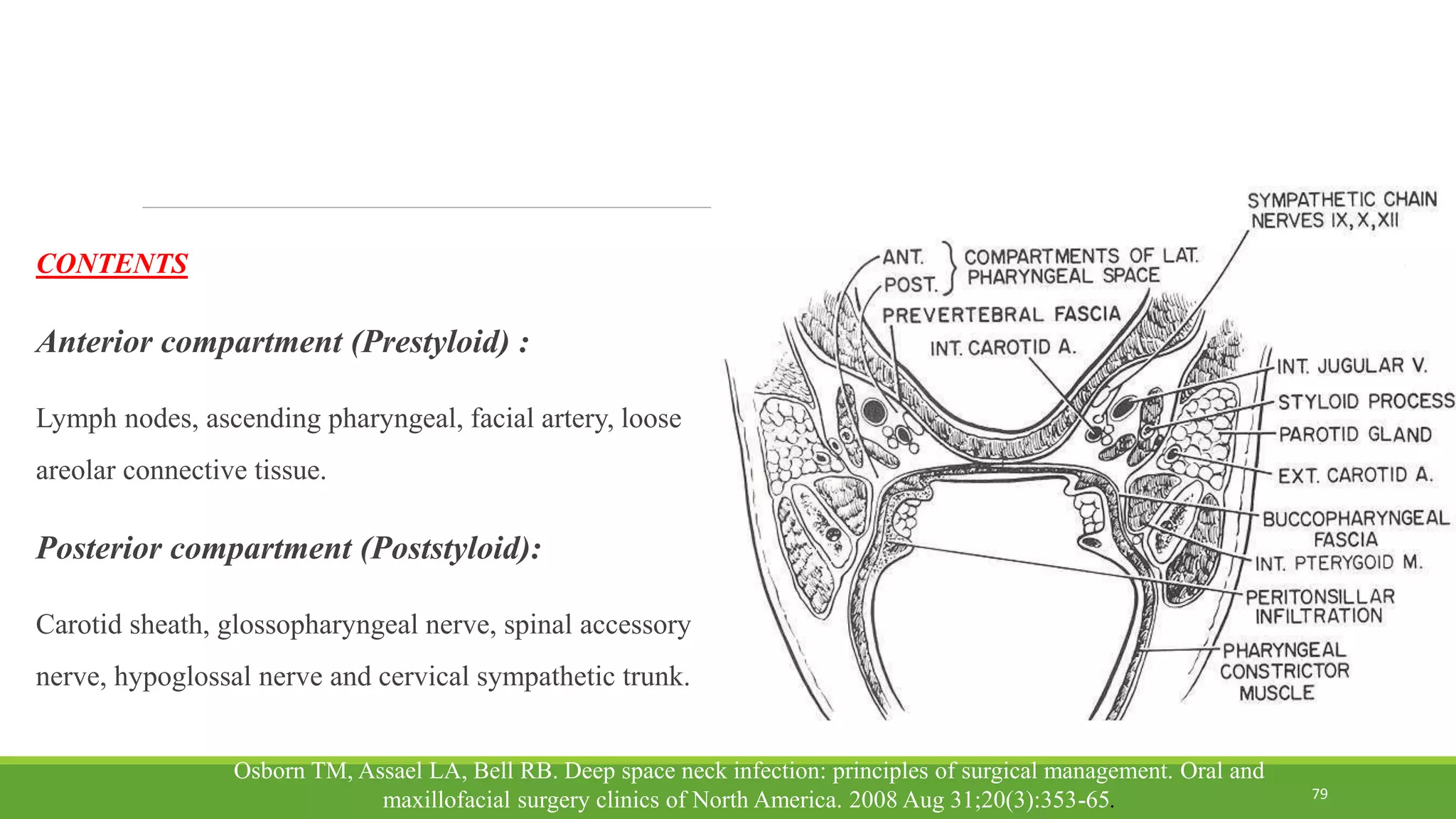
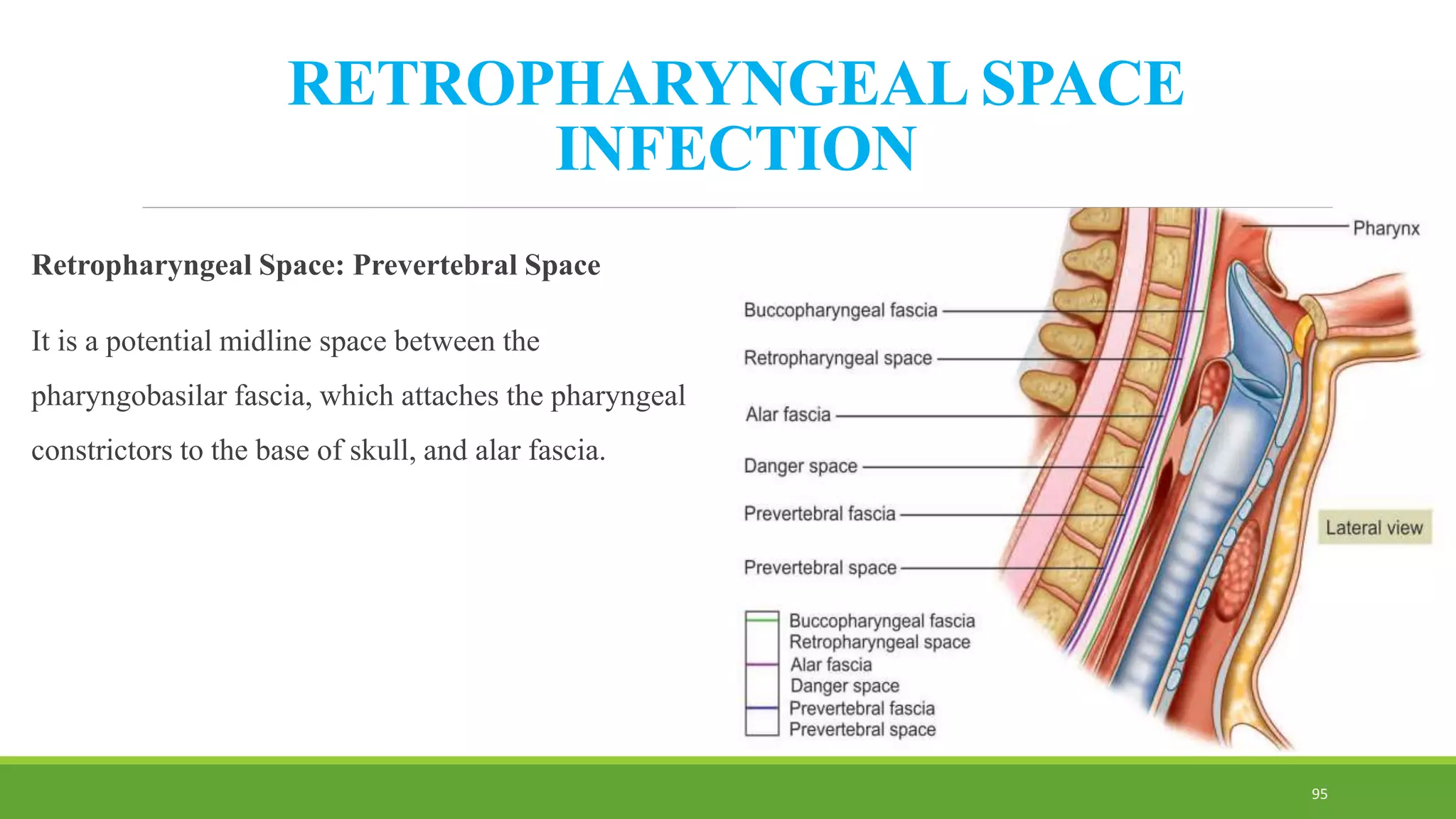
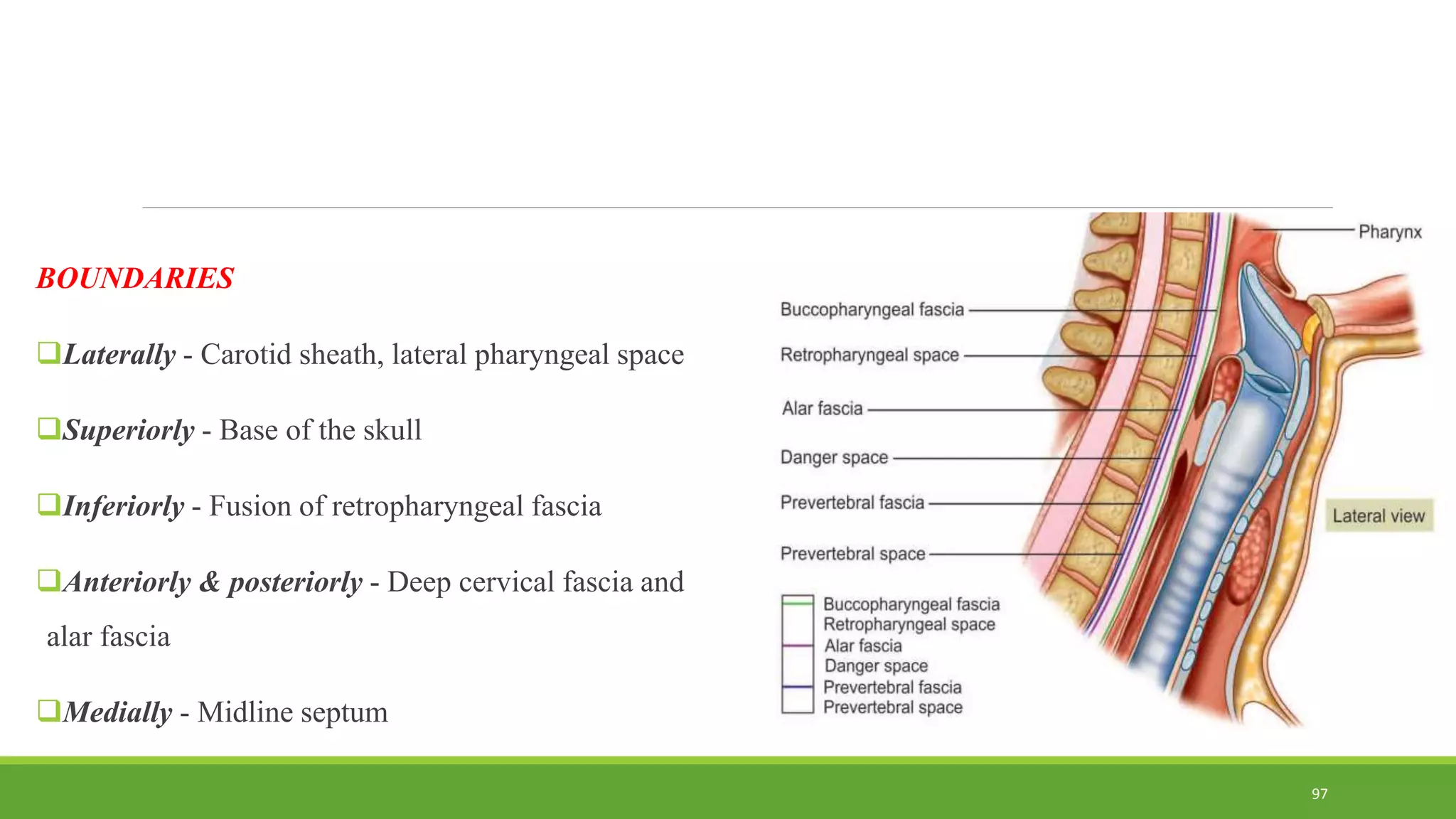
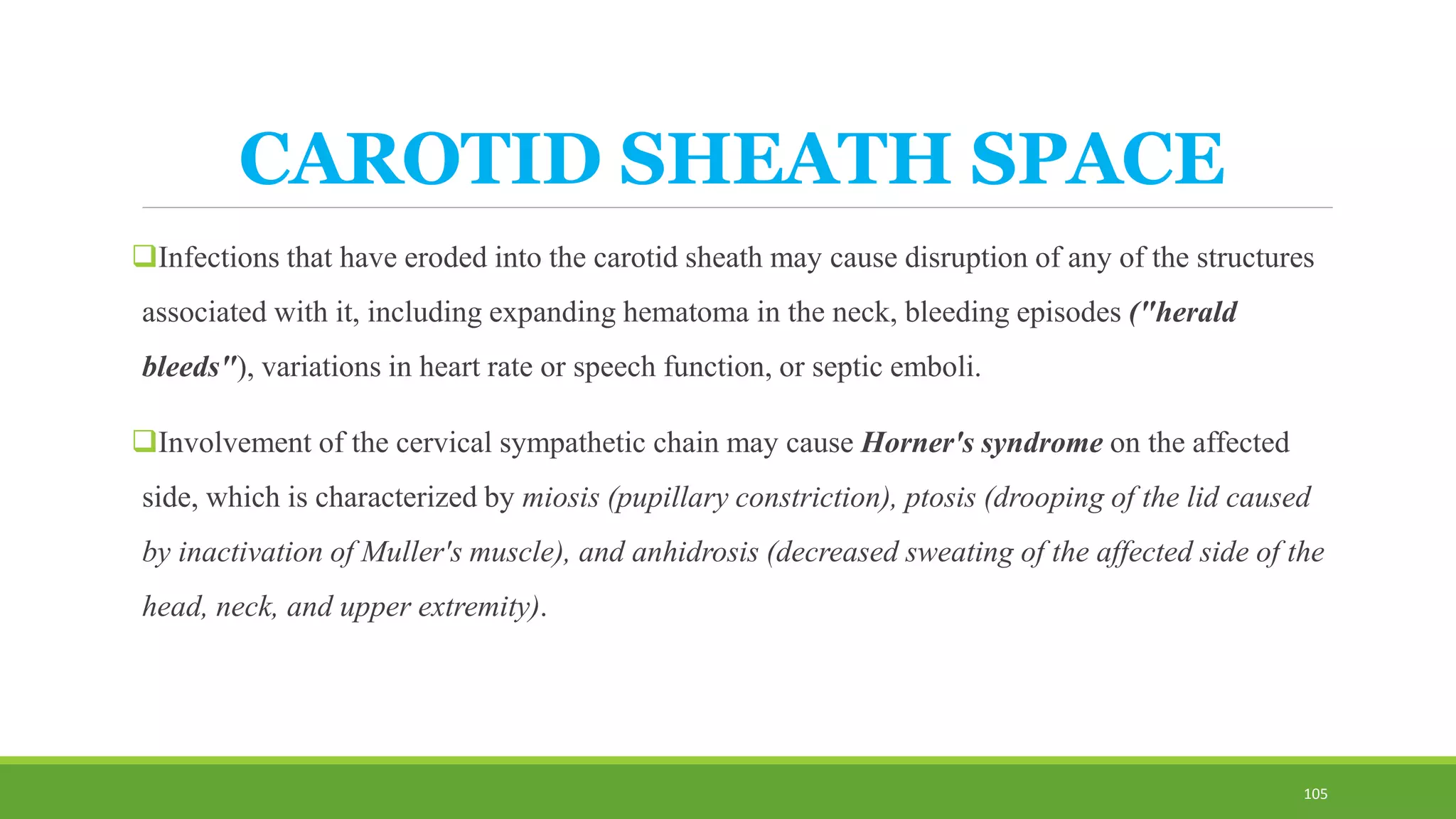
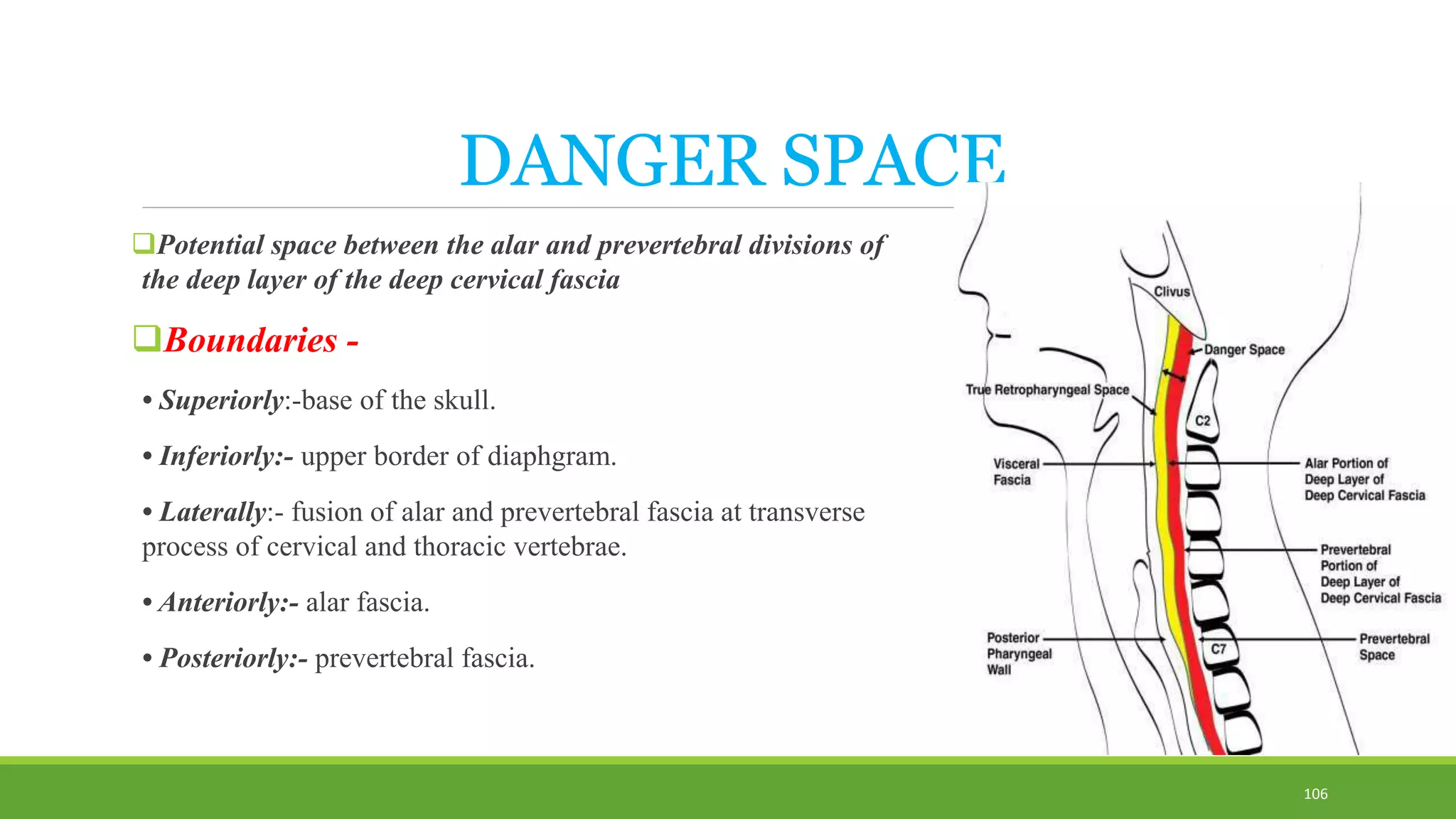
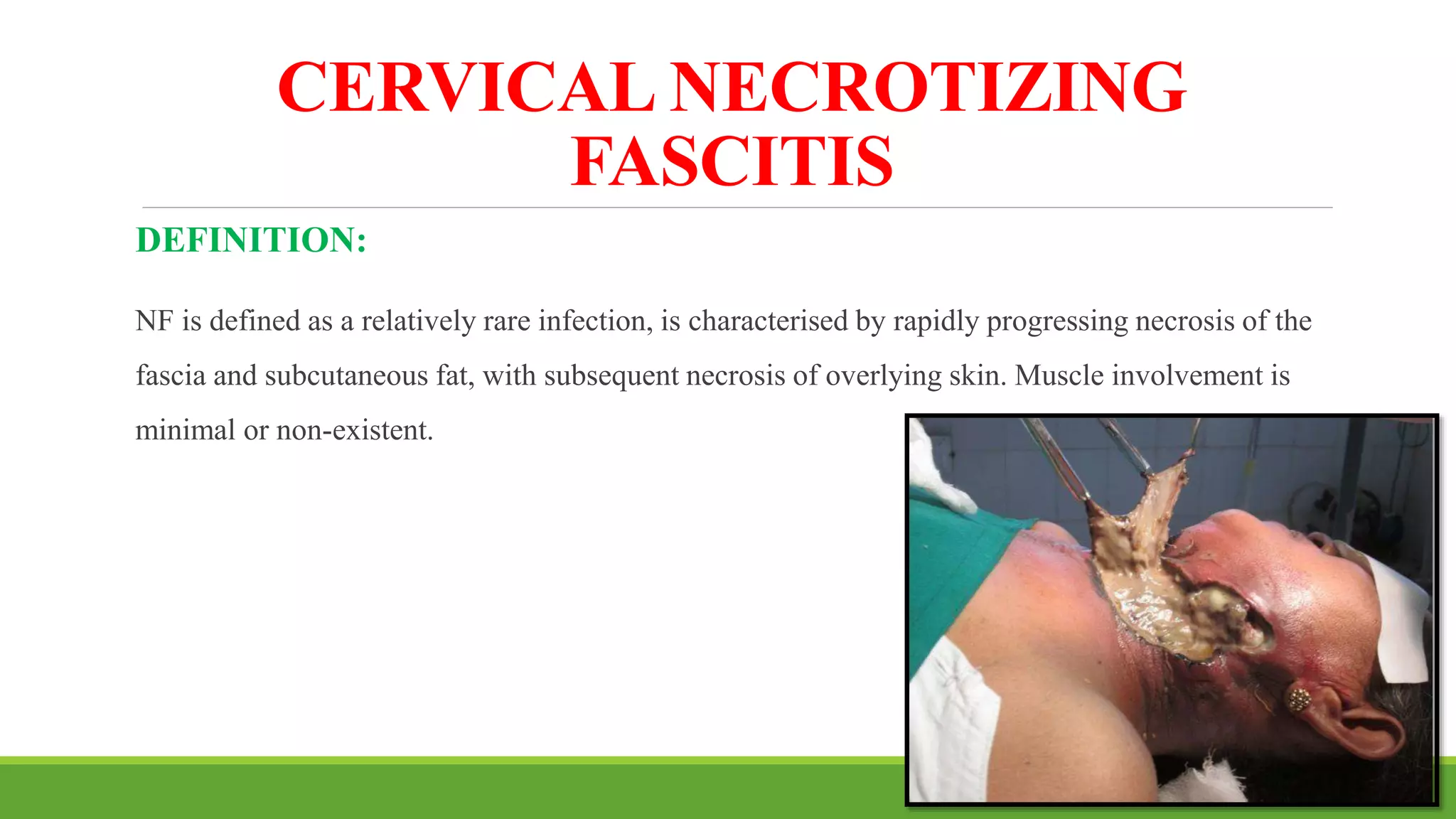
1. The document discusses the anatomy and pathophysiology of odontogenic infections. It describes the layers of fascia in the head and neck region and how infections can spread along these layers.
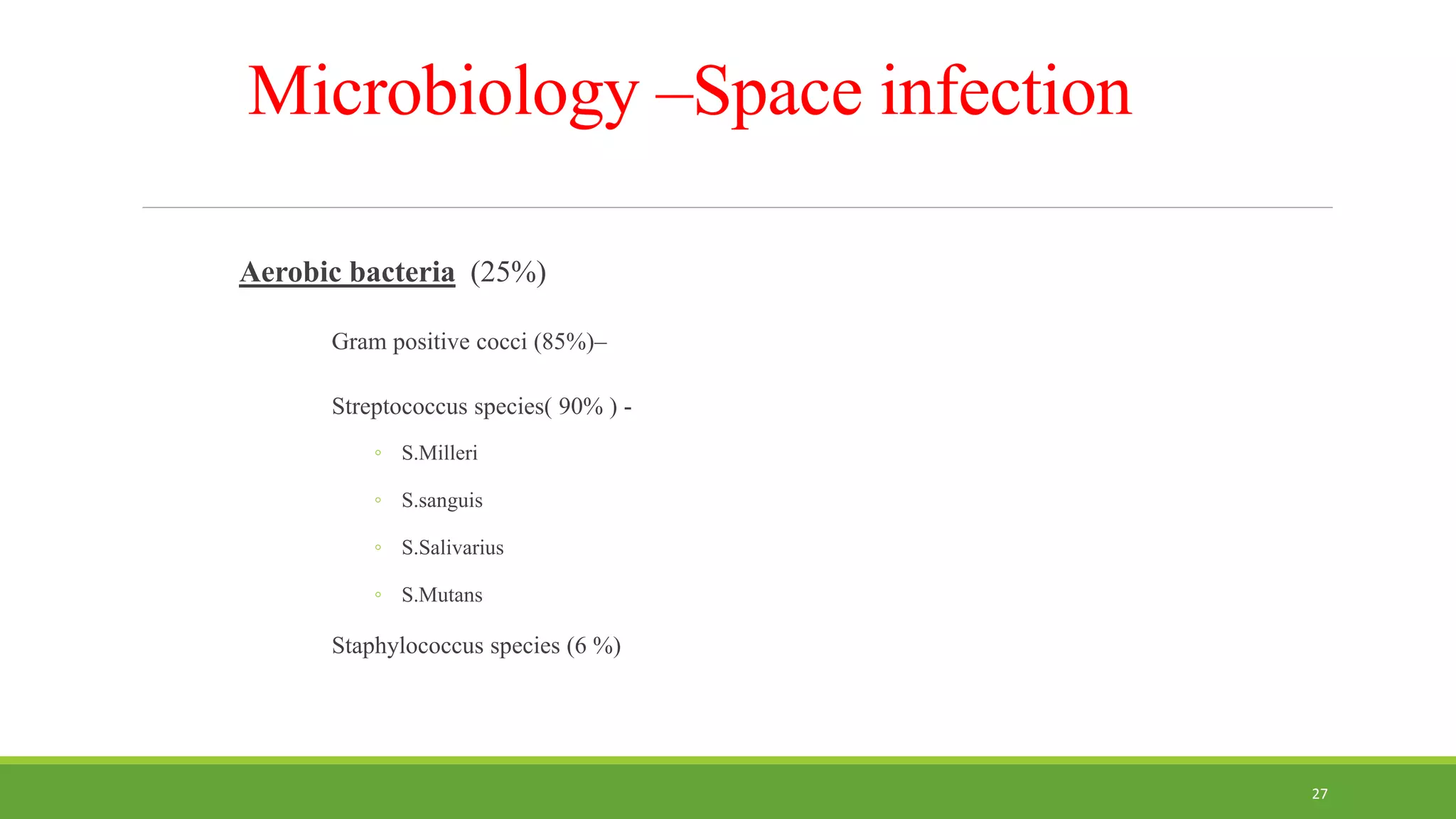
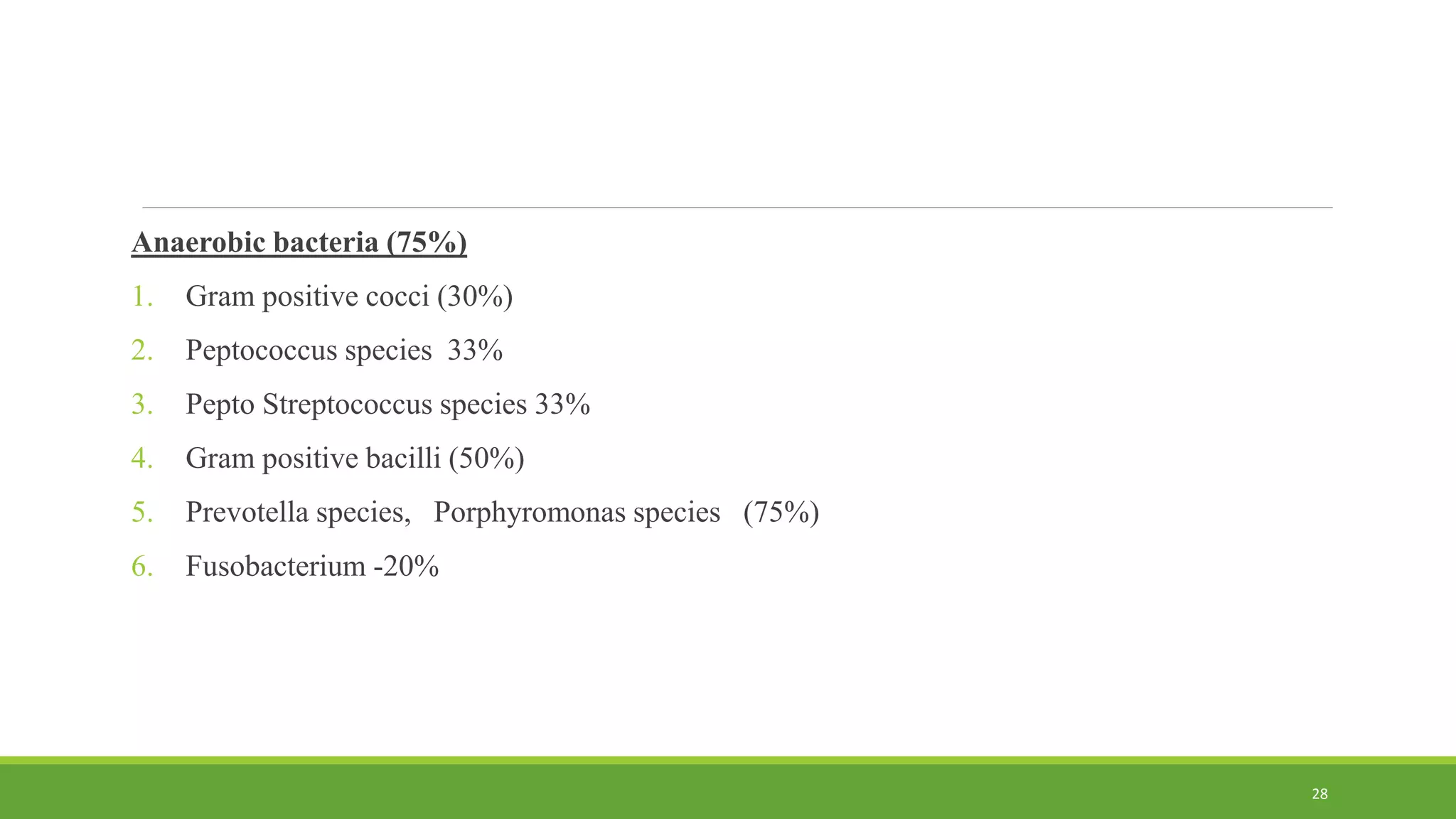
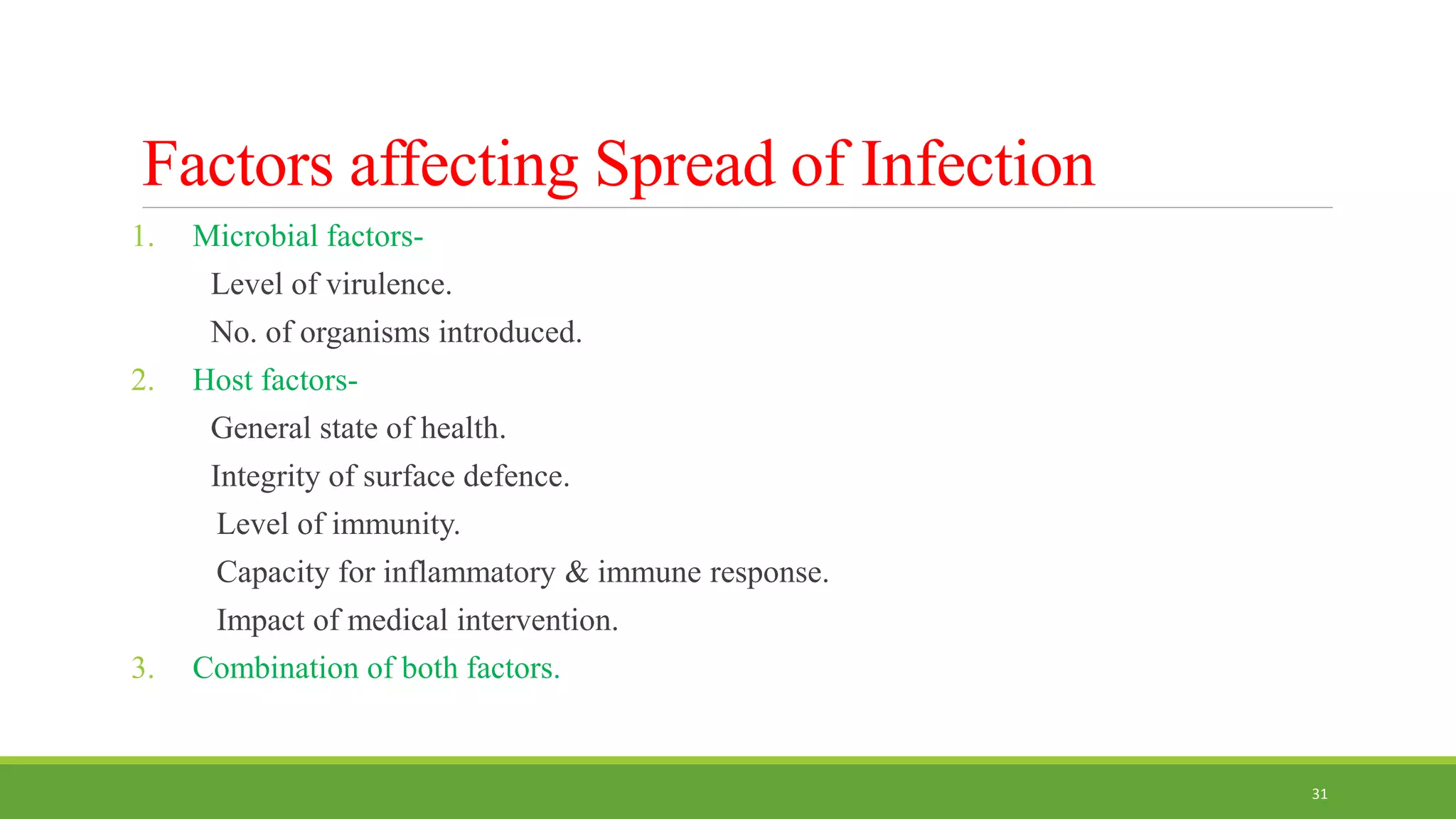
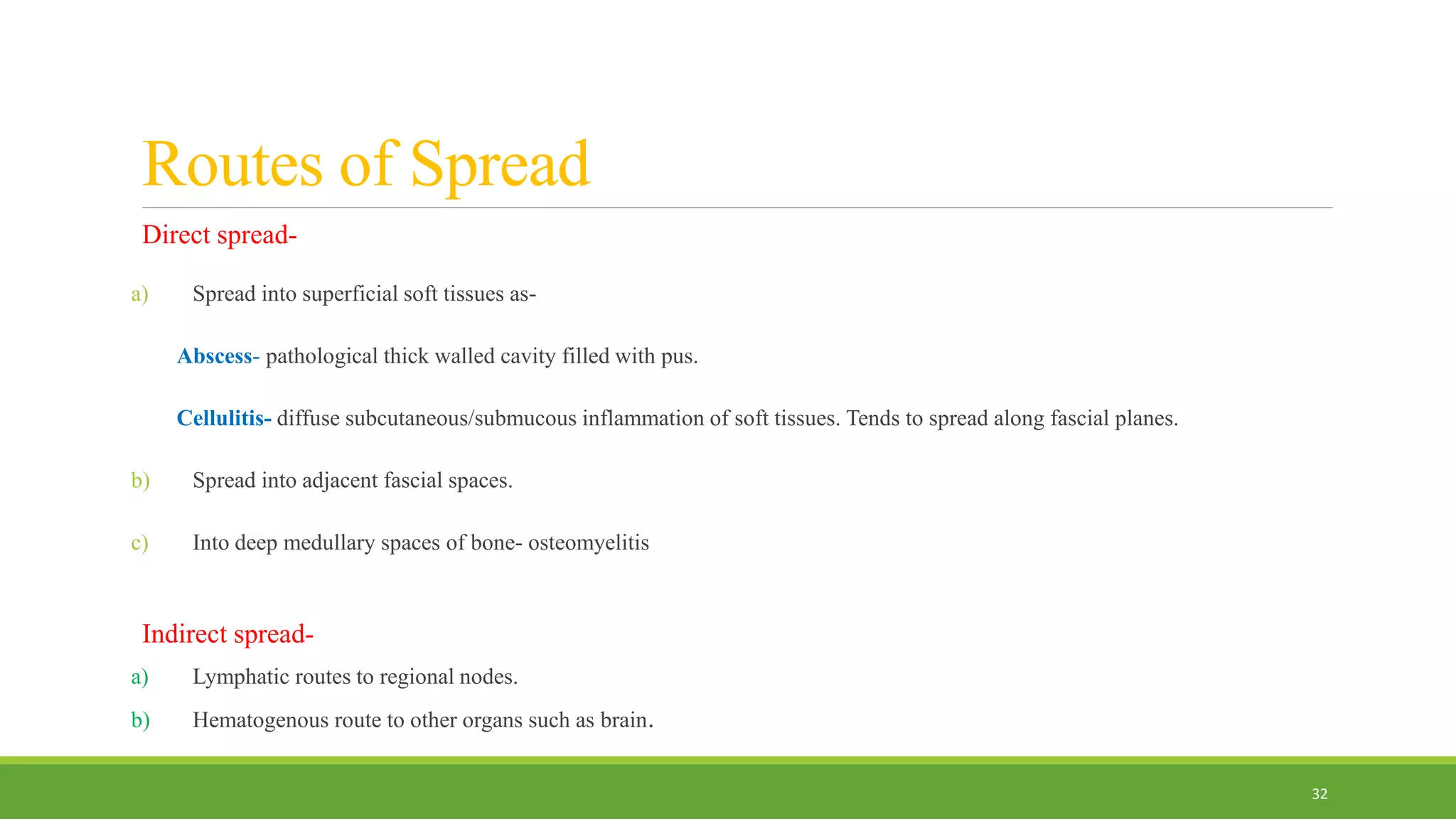
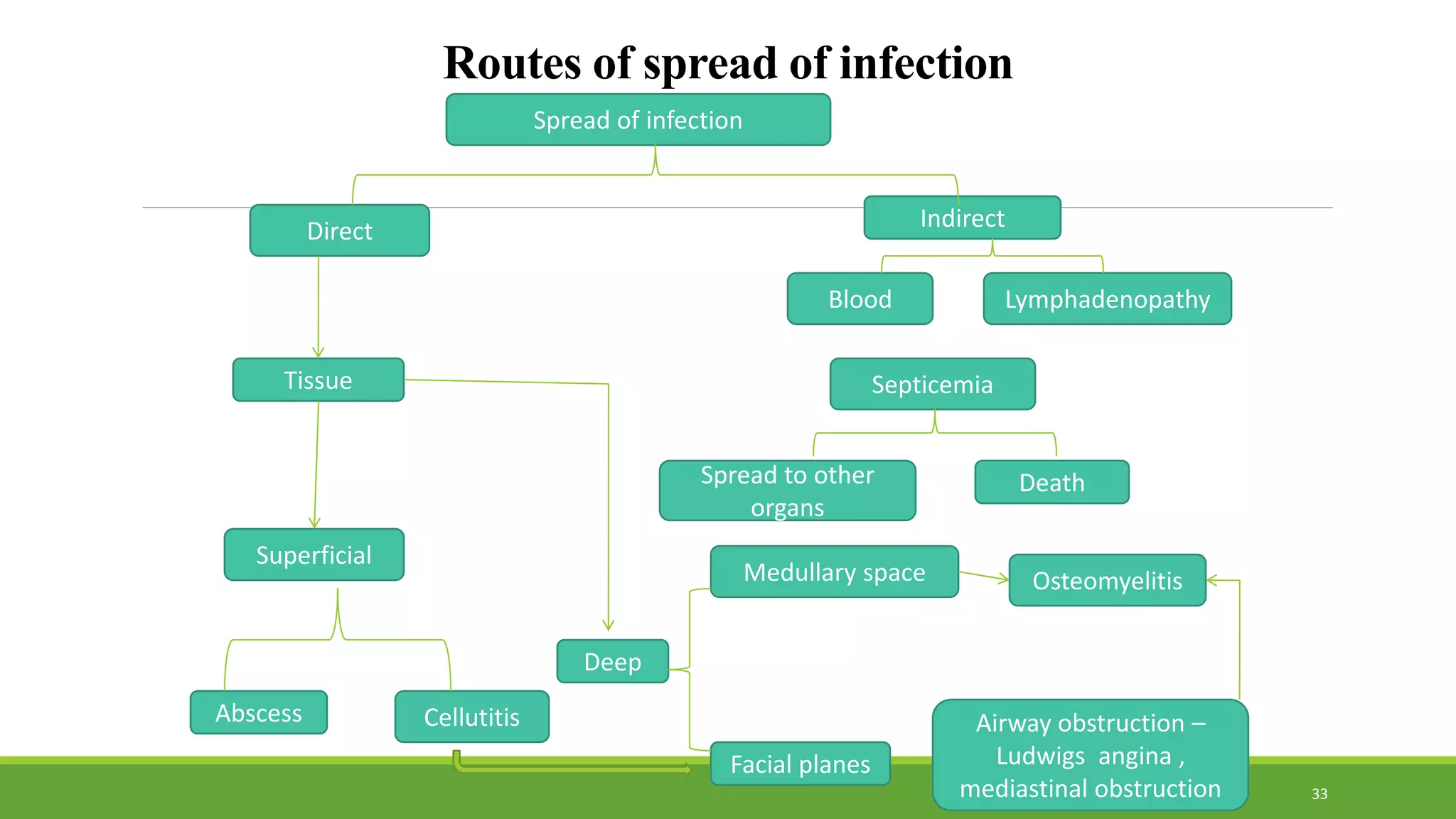
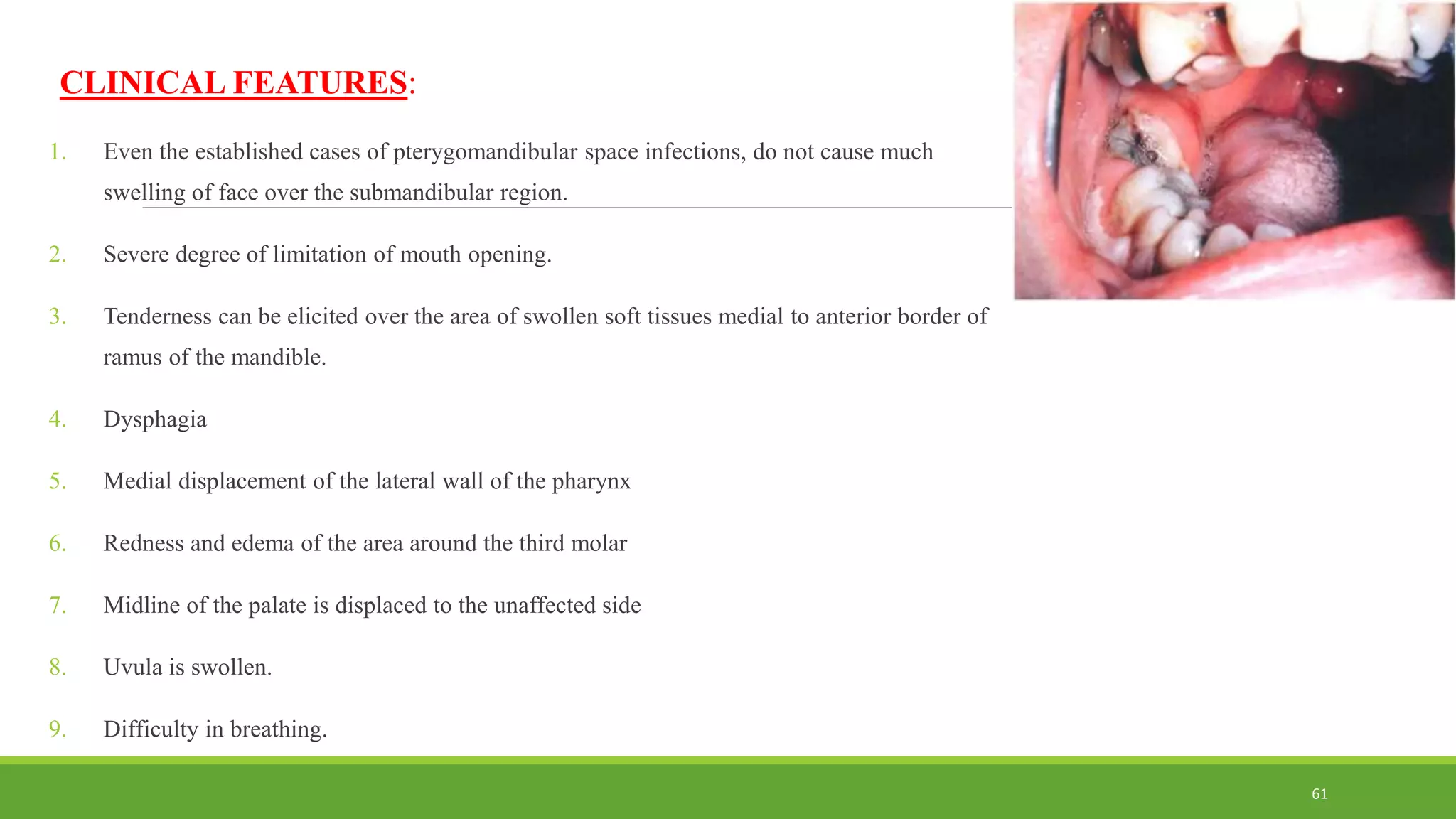
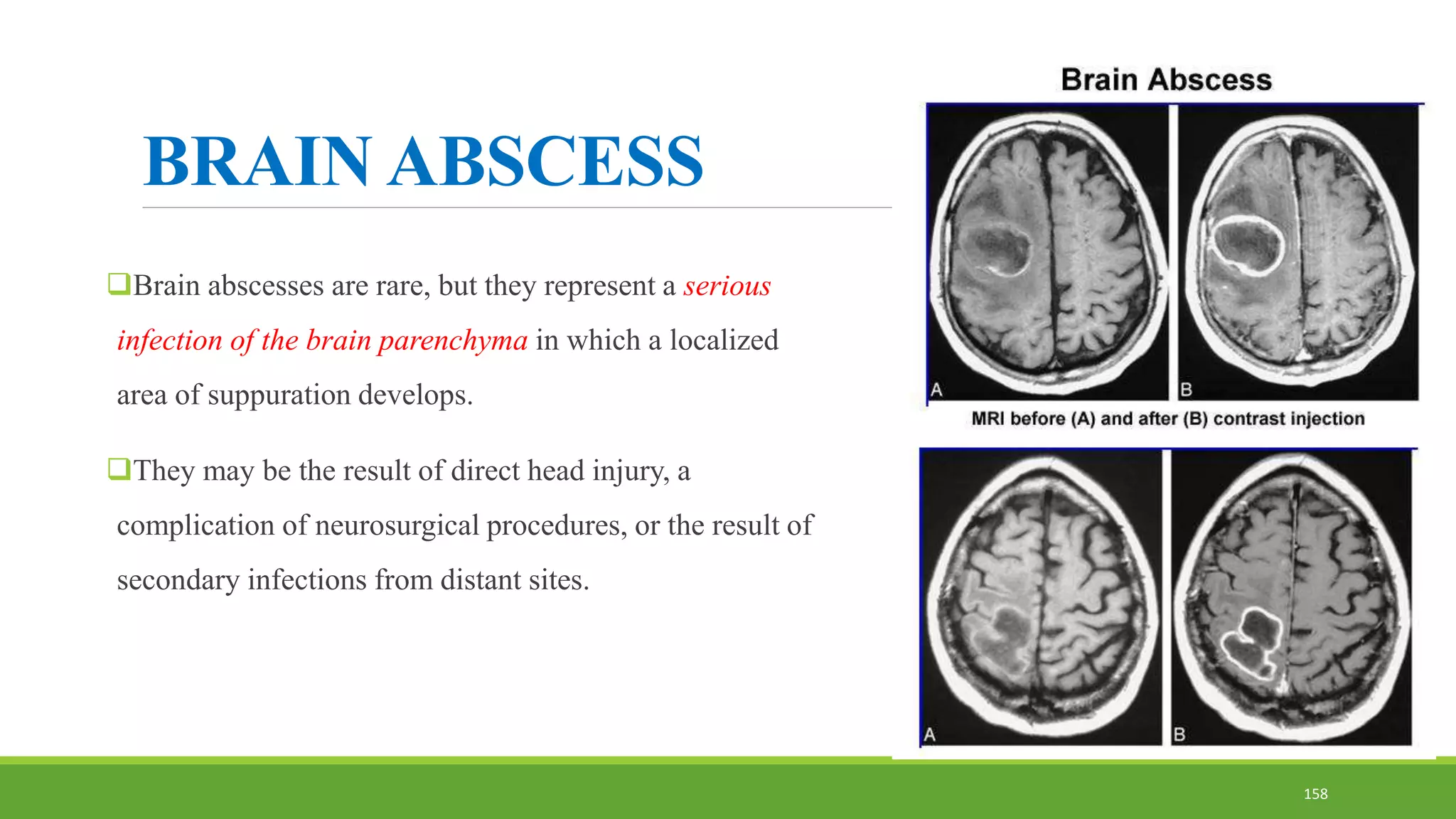
2. Odontogenic infections most commonly involve aerobic bacteria that spread from the site of infection through the path of least resistance in fascial planes.
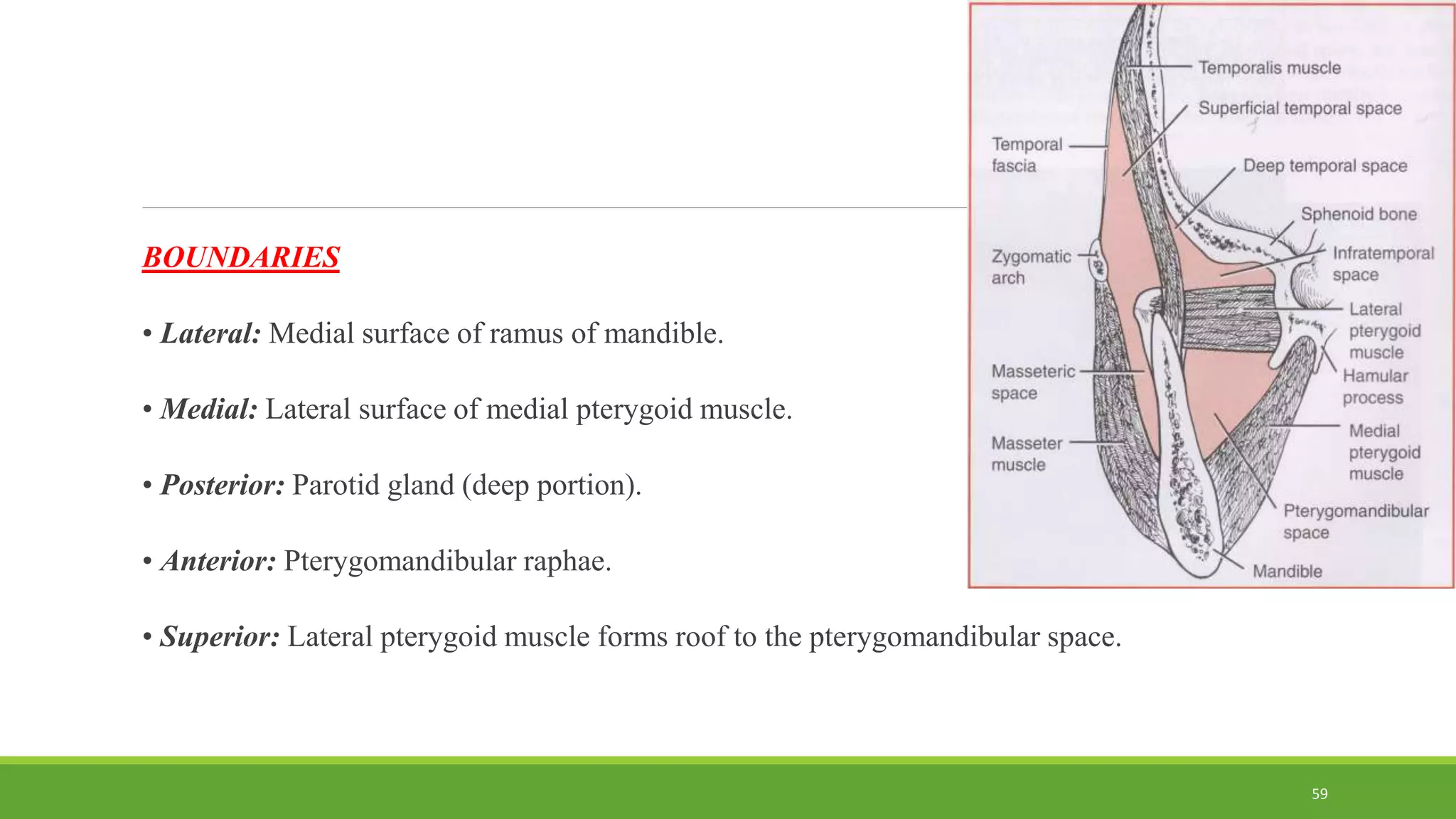
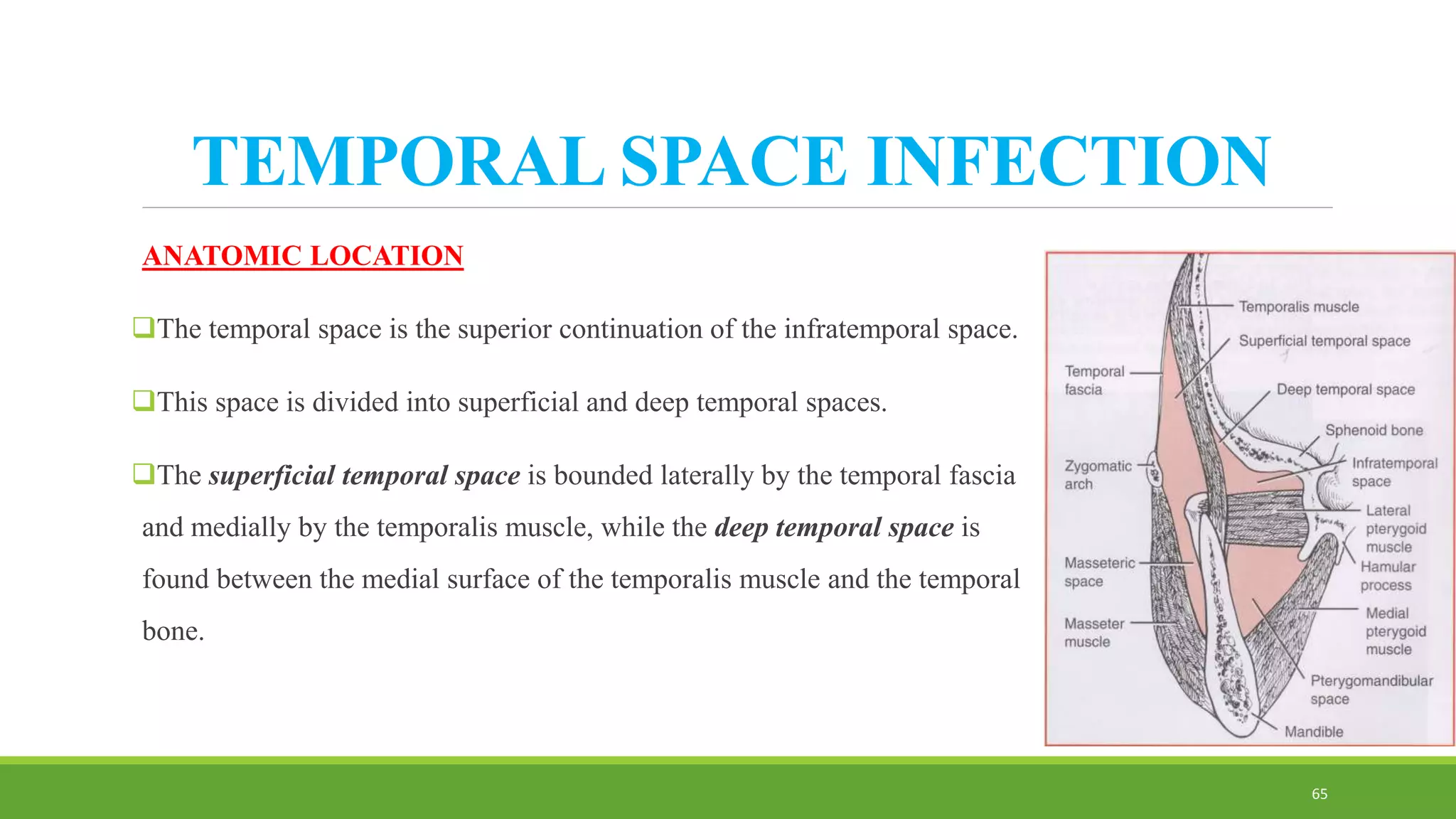
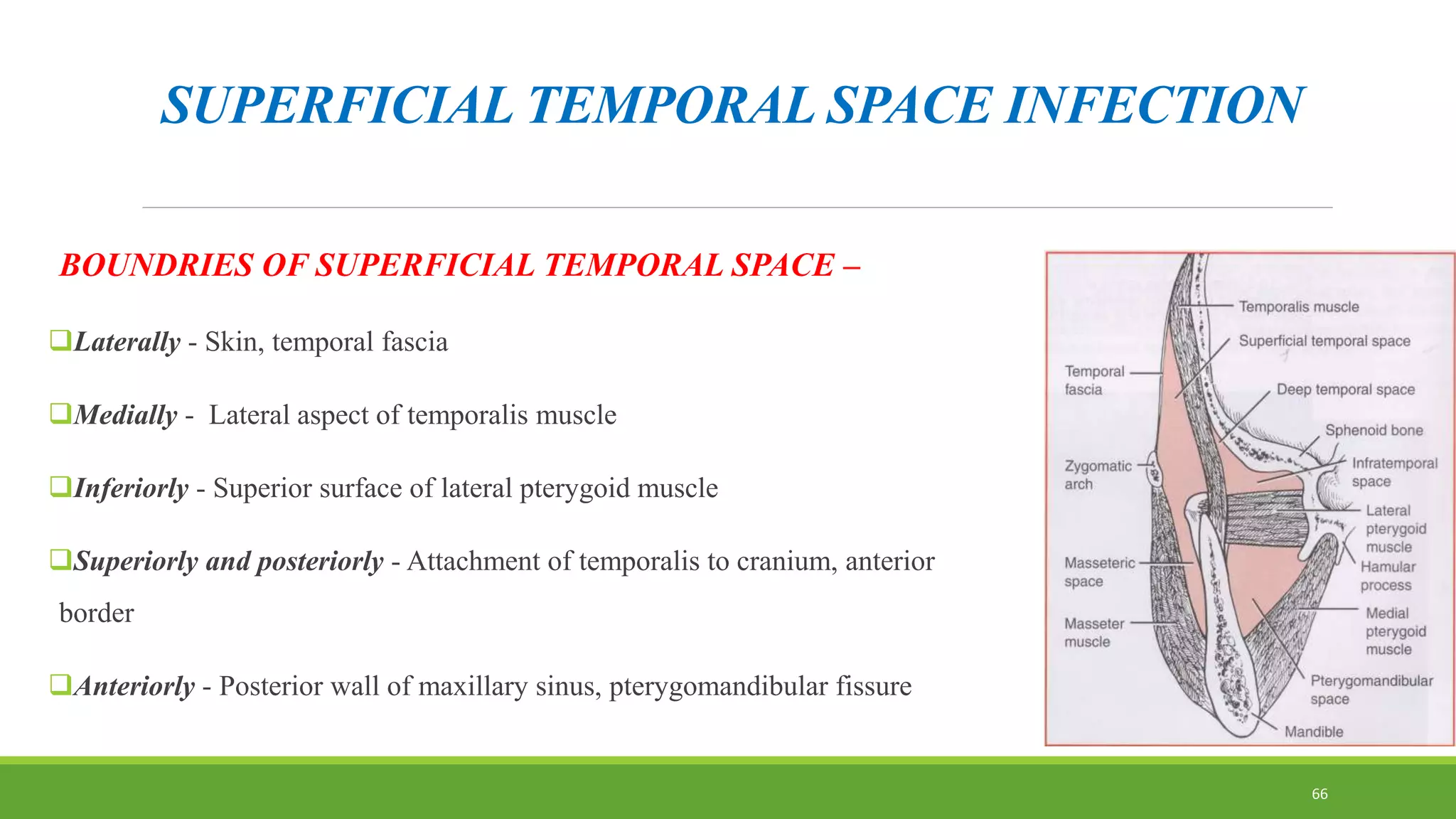
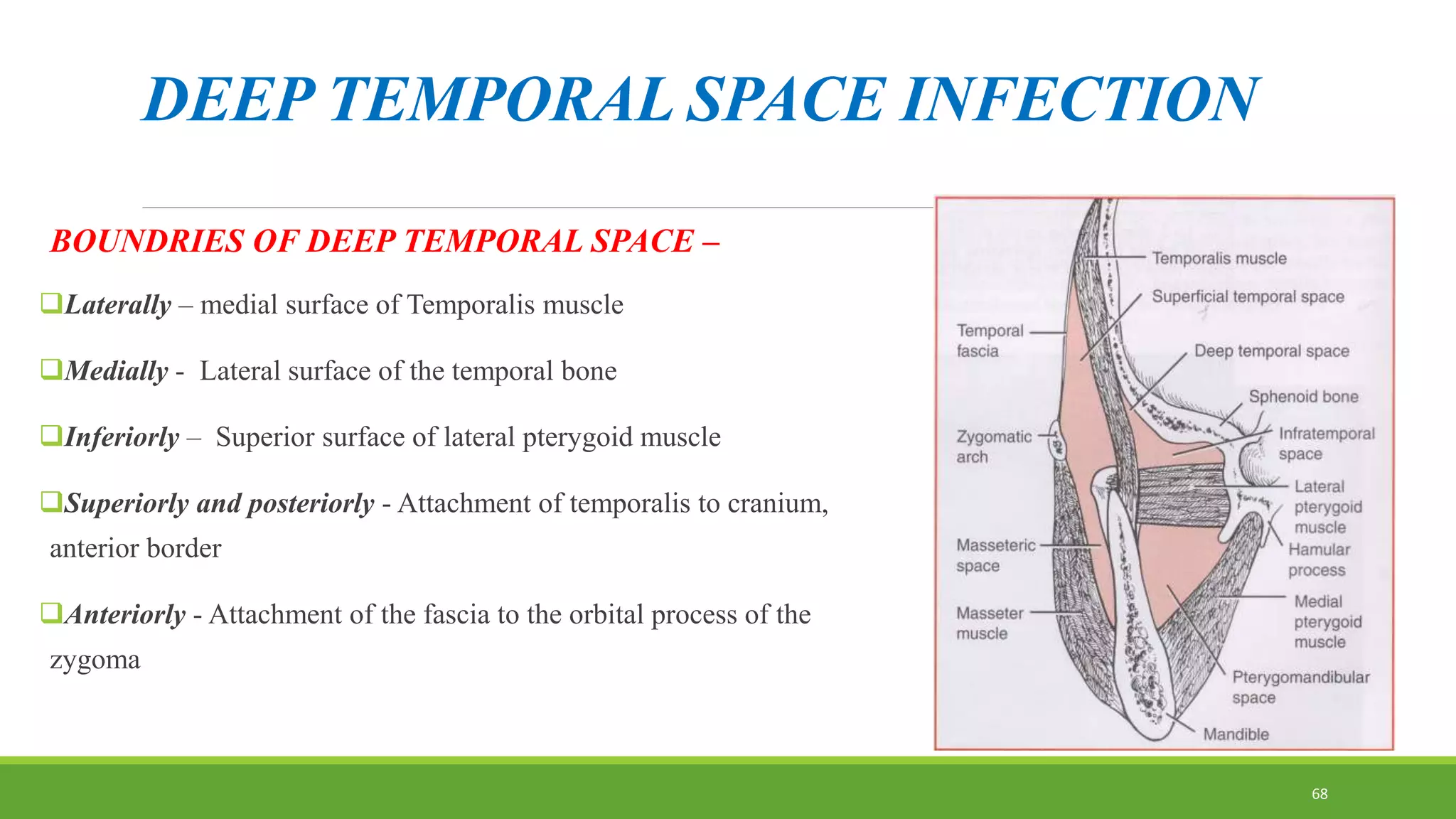
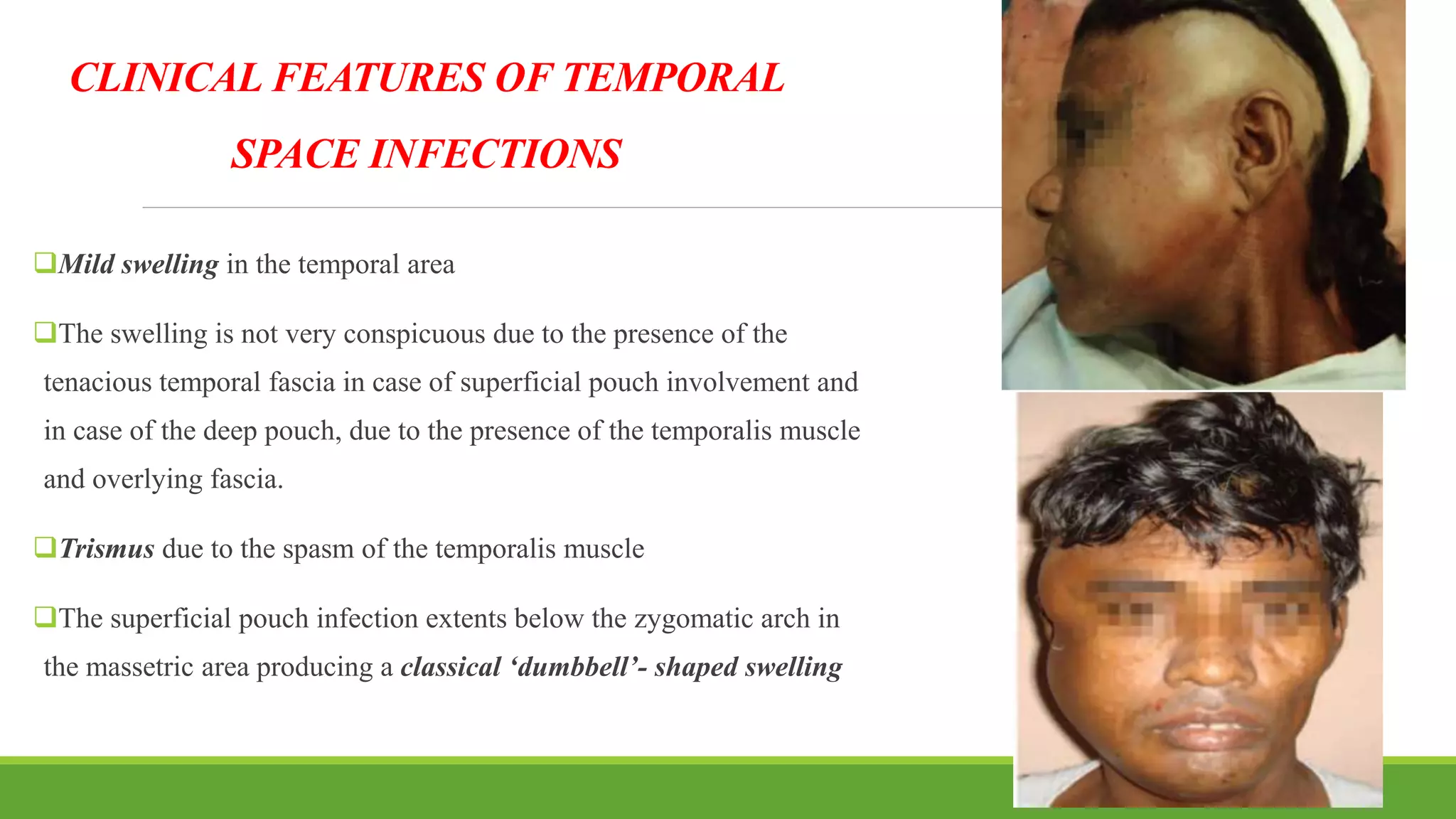
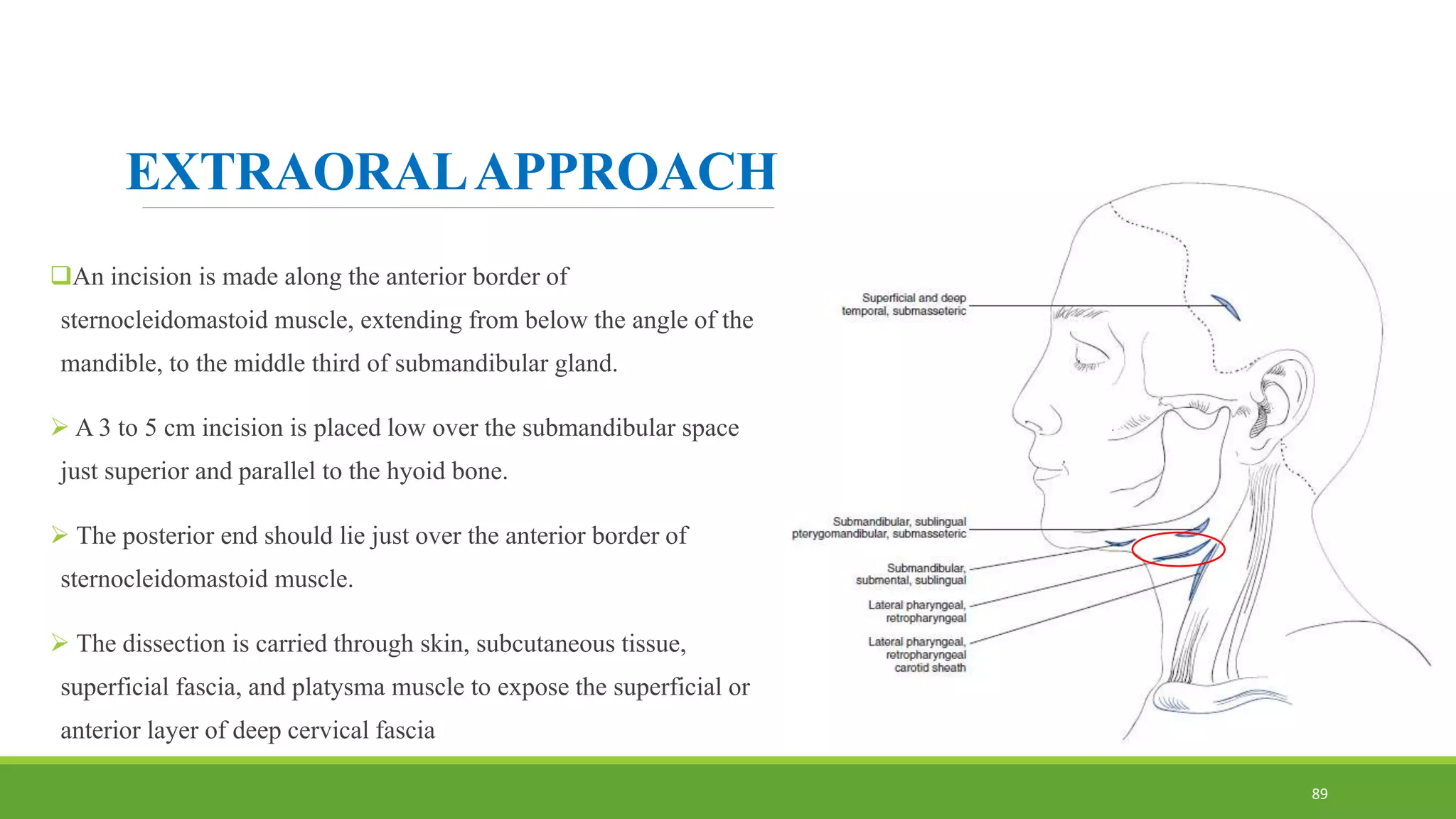
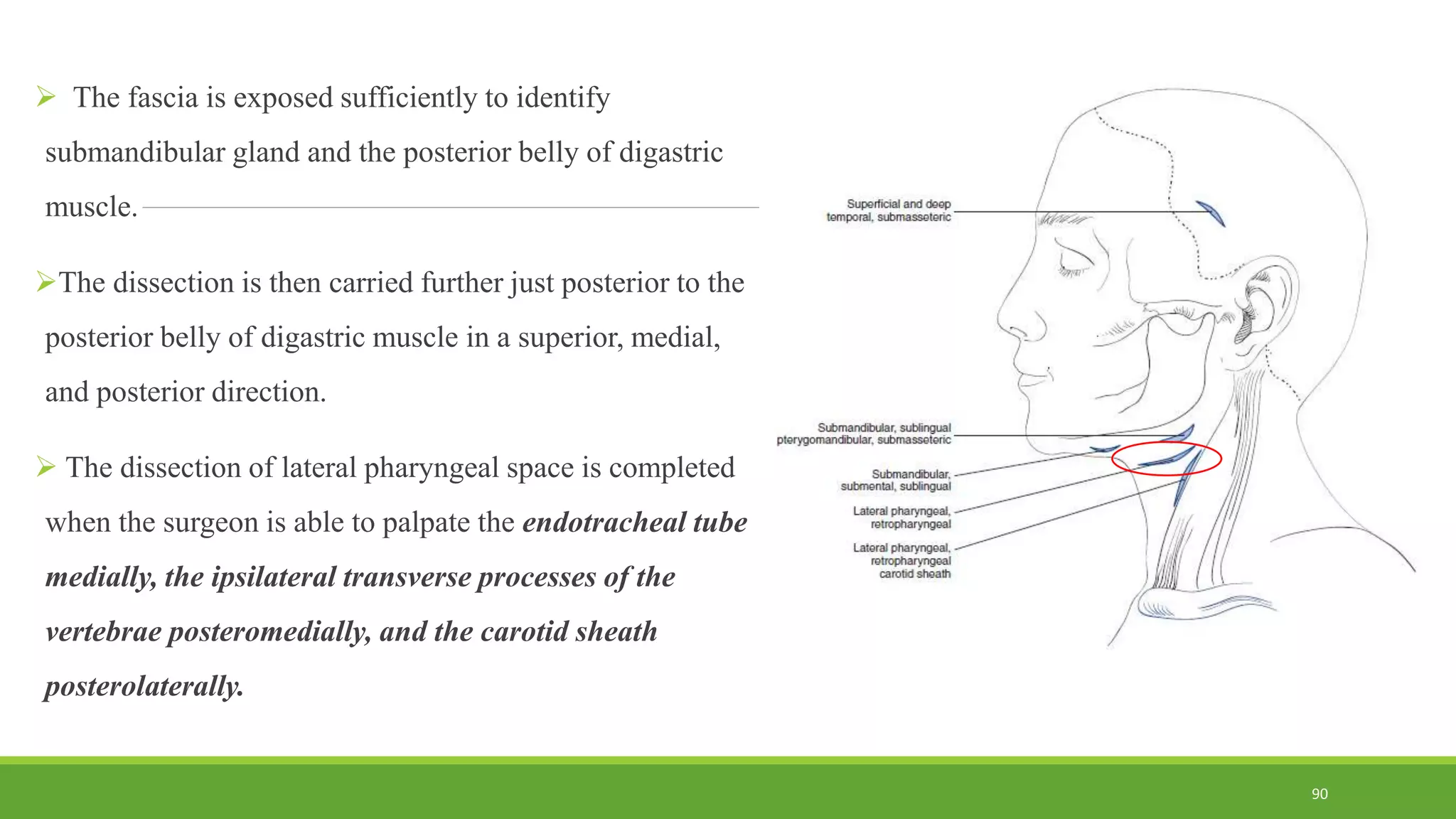
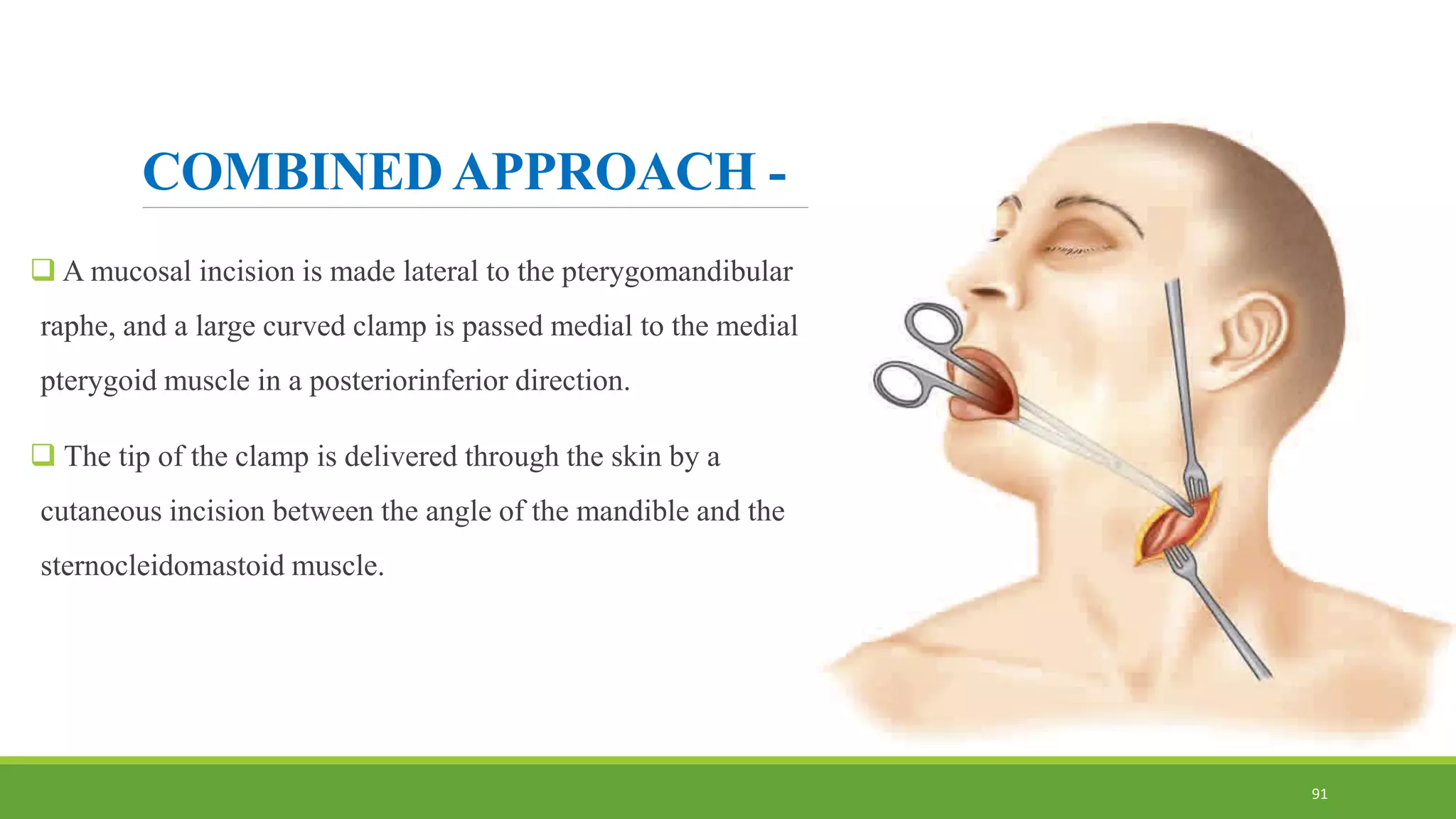
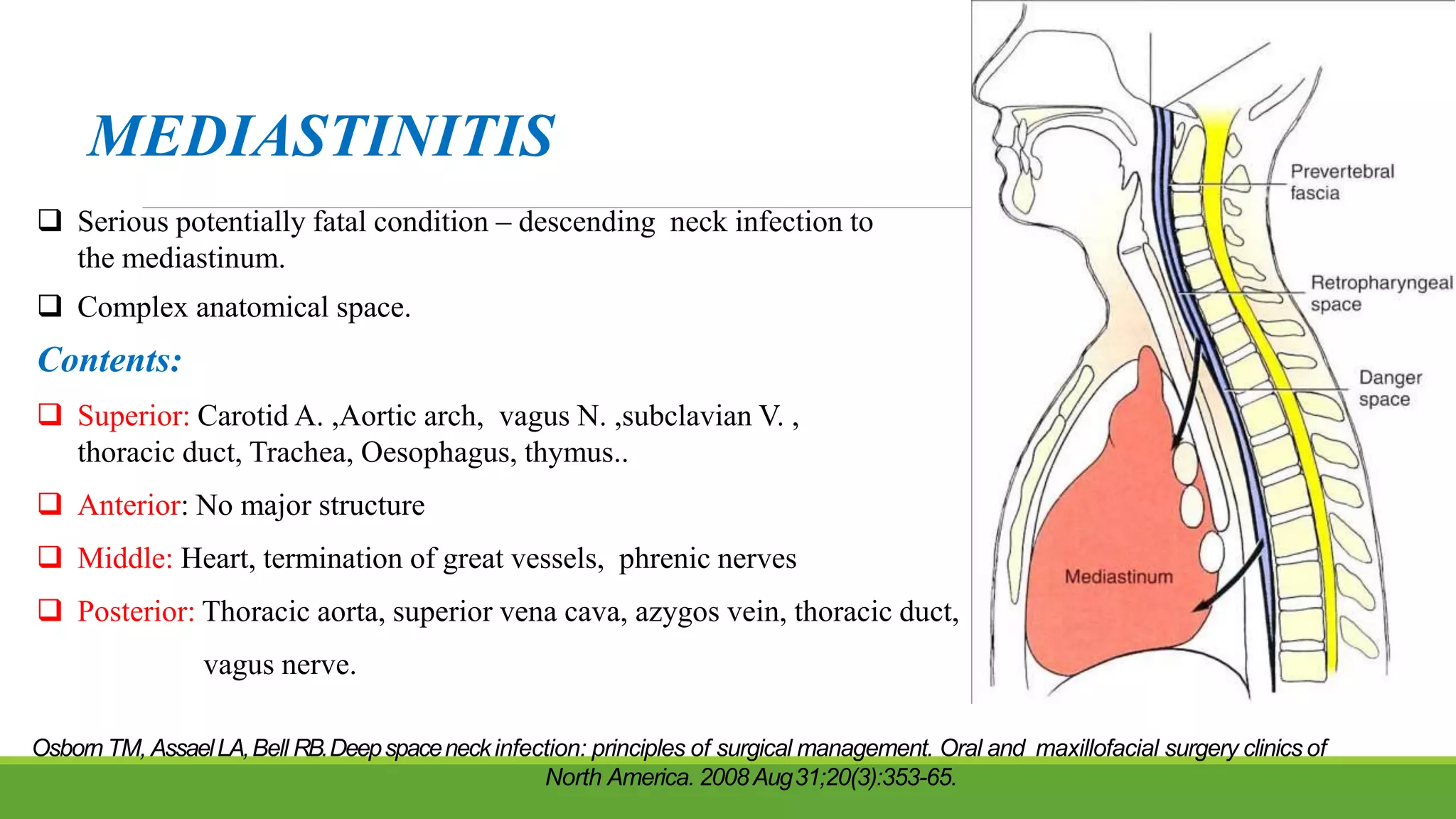
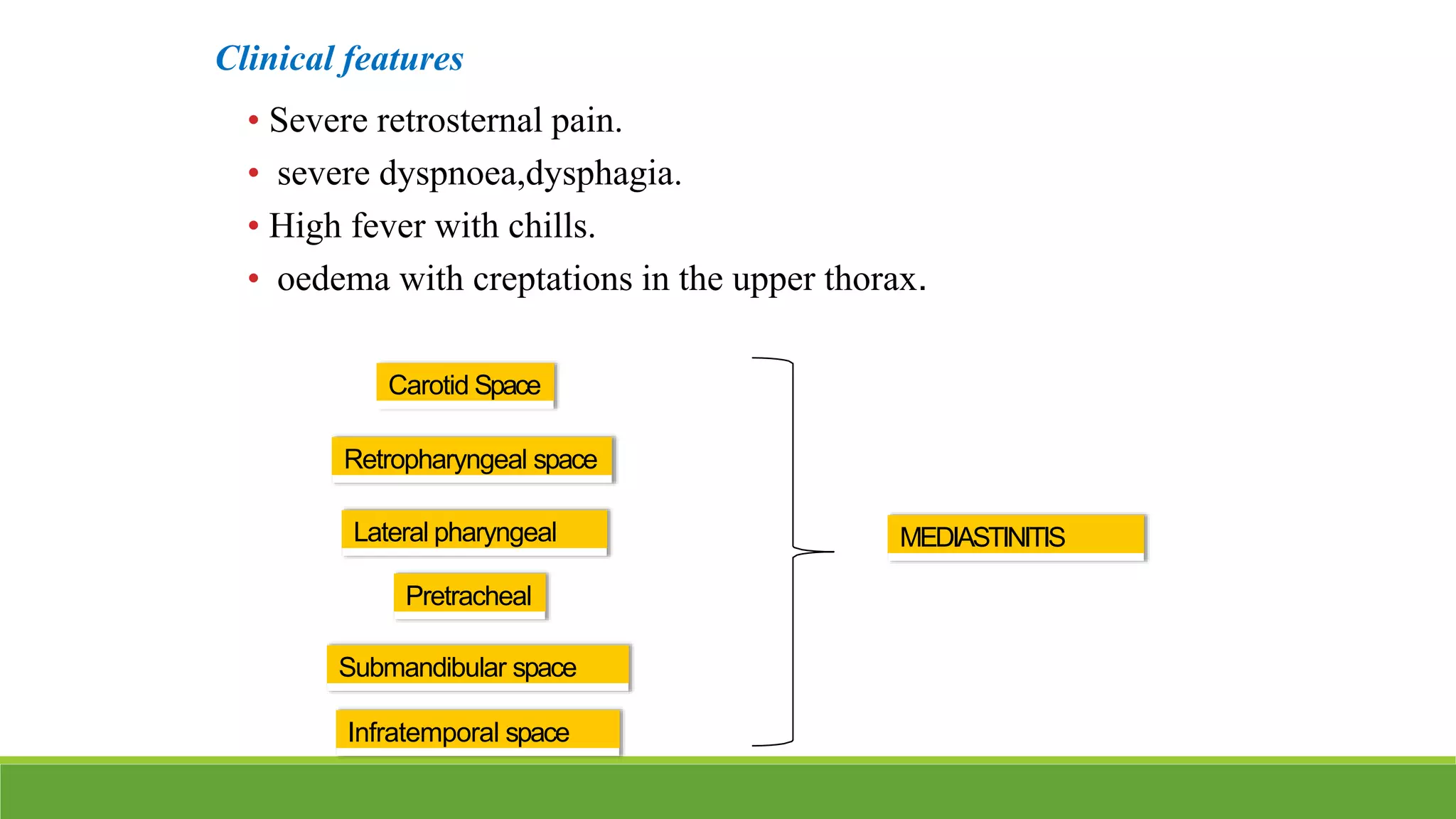
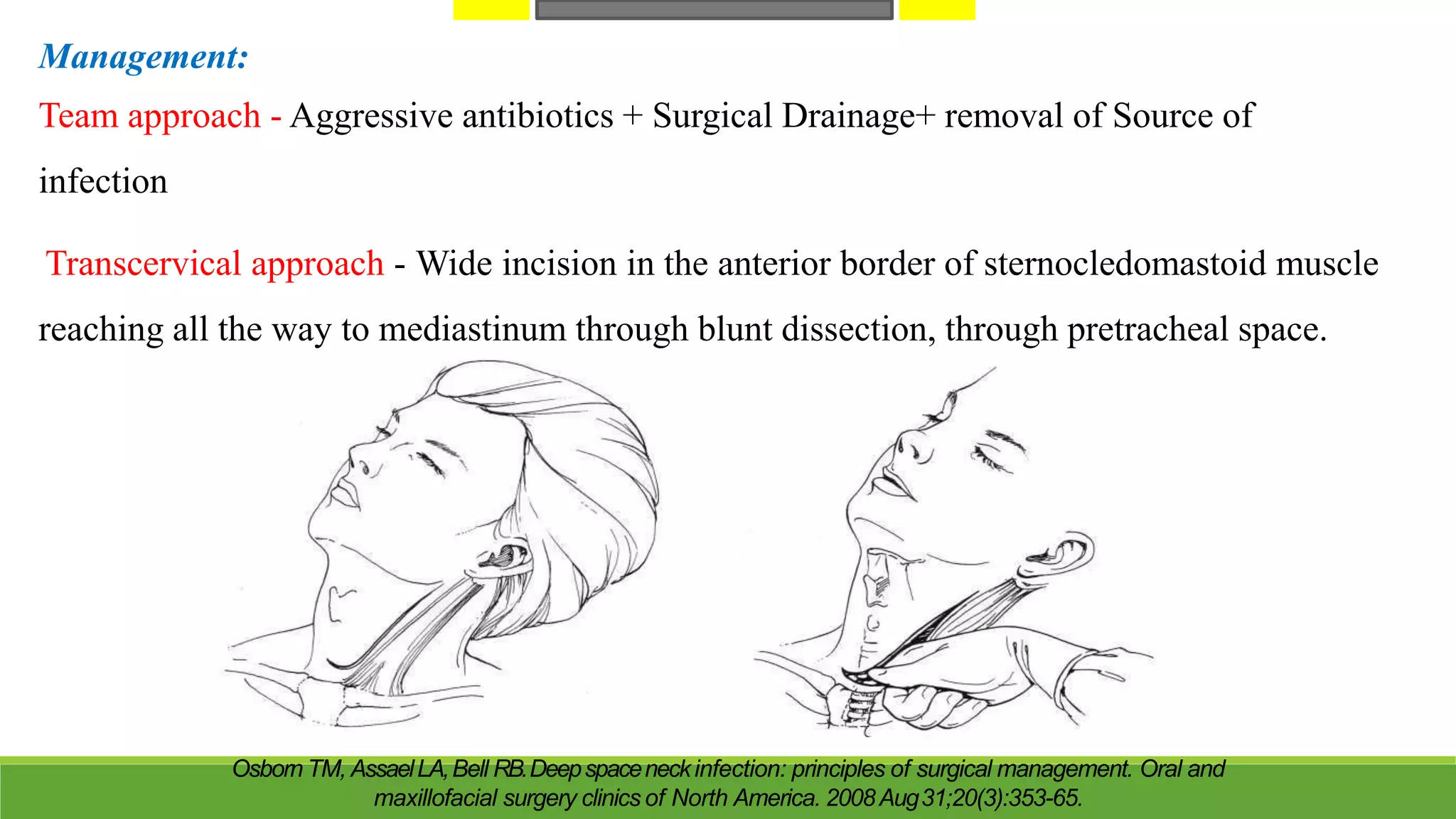
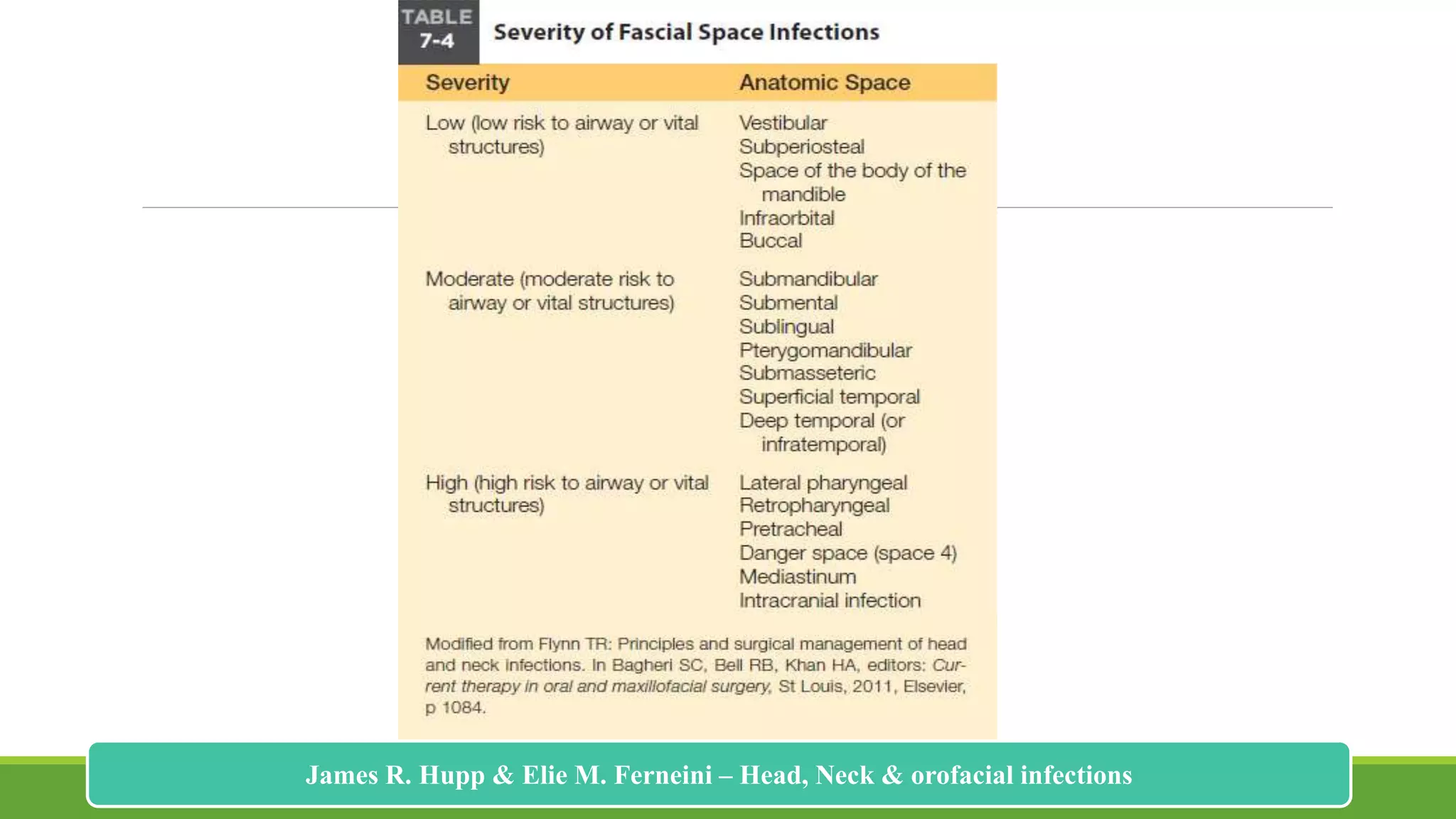
3. Understanding the anatomy of fascial spaces is important for maxillofacial surgeons to properly manage and treat odontogenic infections to prevent complications from spread.