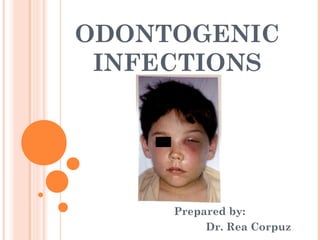
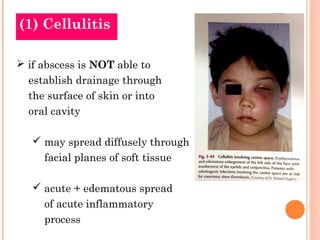
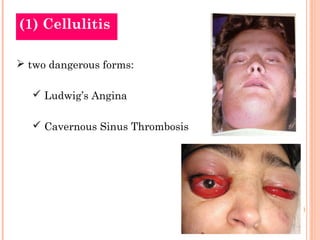
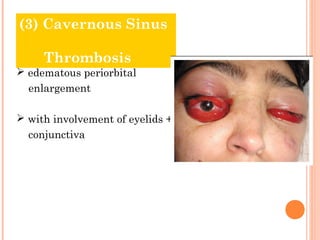
(1) The document discusses various odontogenic infections including cellulitis, Ludwig's angina, cavernous sinus thrombosis, and osteomyelitis.
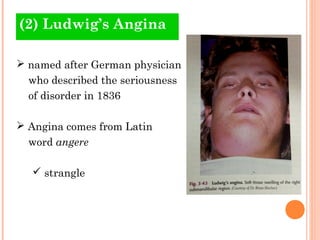
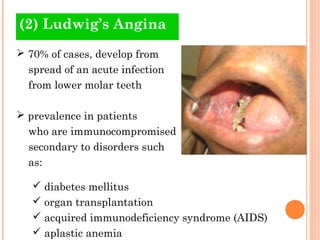
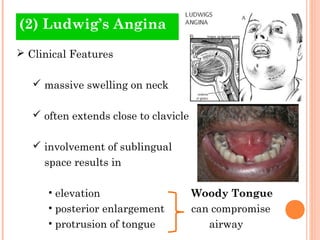
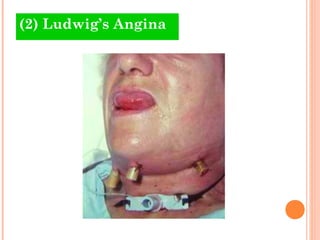
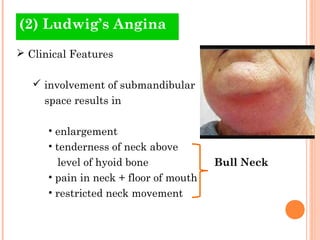
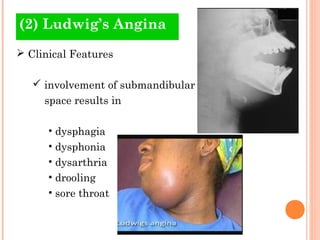
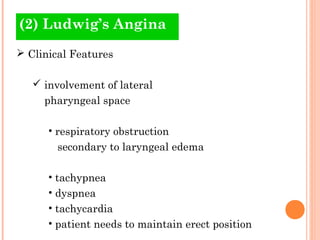
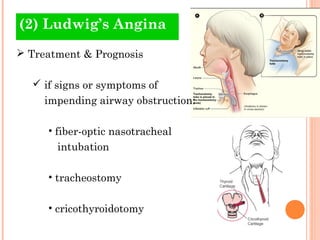
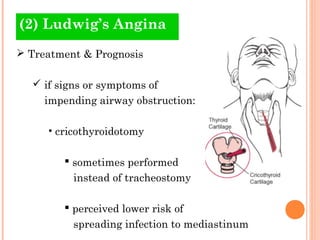
(2) Ludwig's angina is a serious bacterial infection that causes massive swelling of the neck and floor of the mouth. It develops from a dental infection and can compromise the airway.
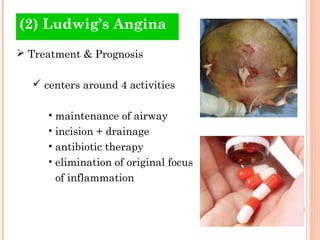
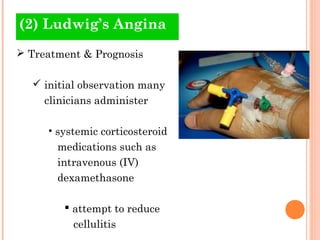
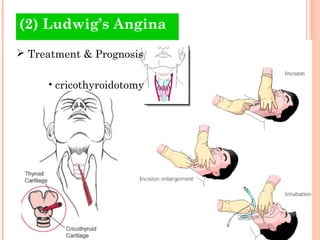
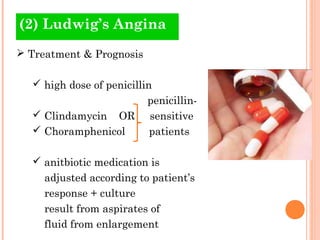
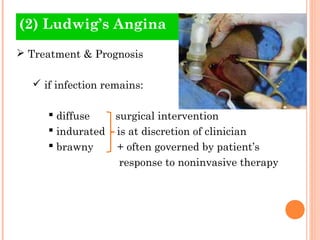
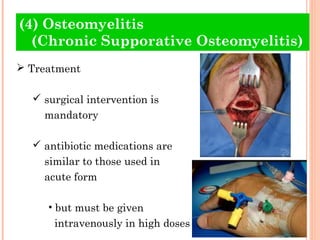
(3) Treatment for these infections involves drainage of abscesses, high-dose antibiotics, and potentially surgical intervention to maintain the airway if it becomes obstructed.