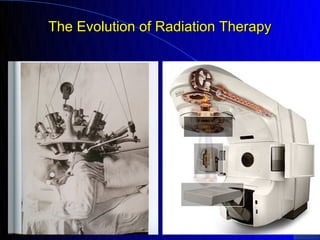
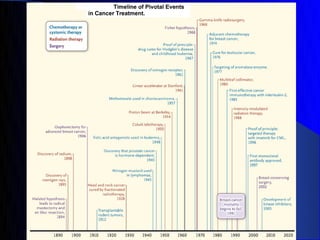
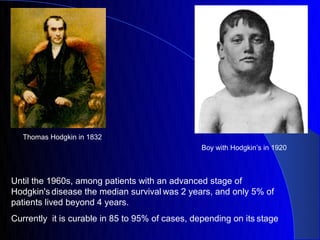
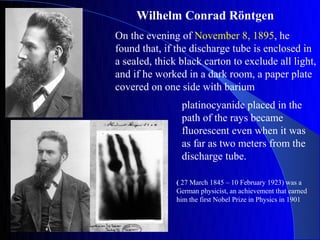
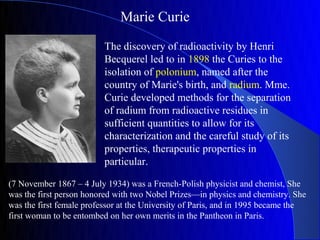
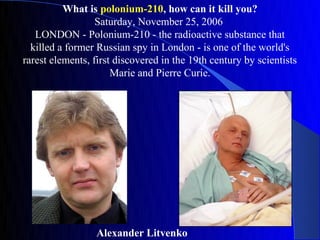
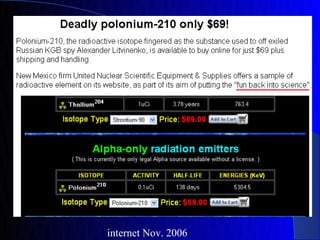
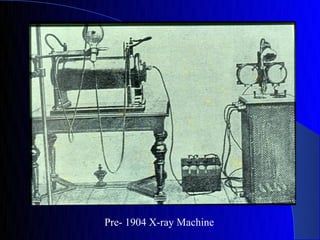
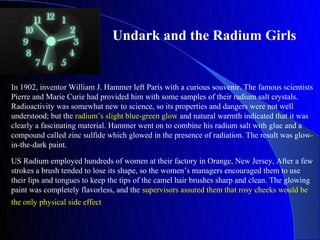
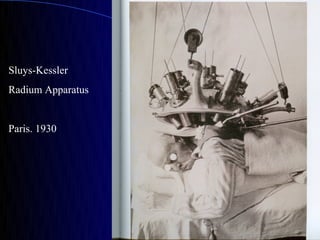
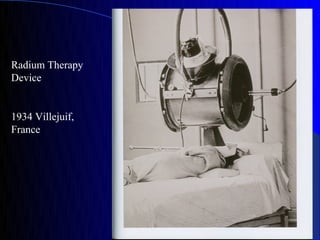
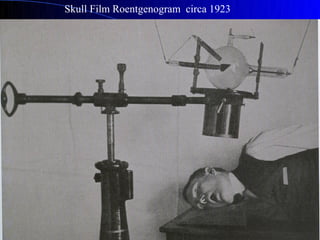
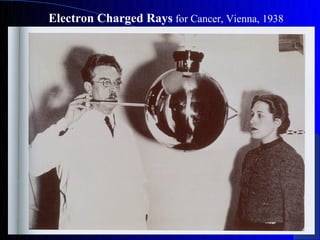
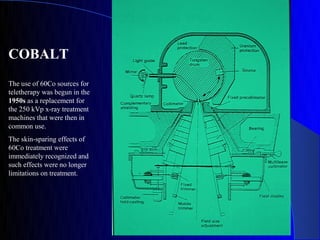
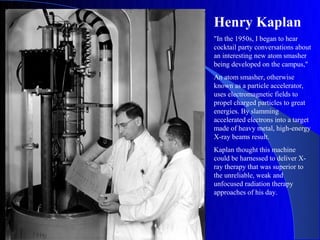
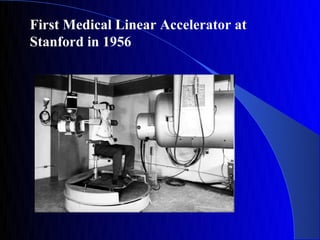
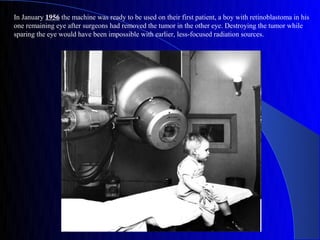
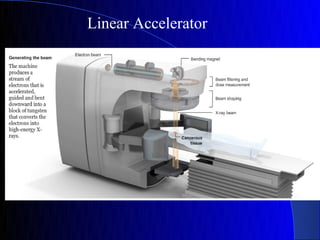
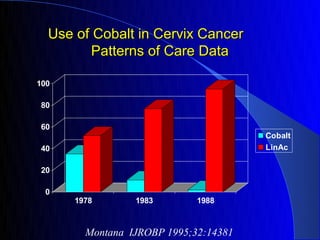
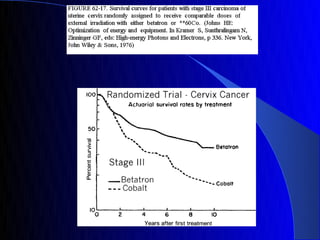
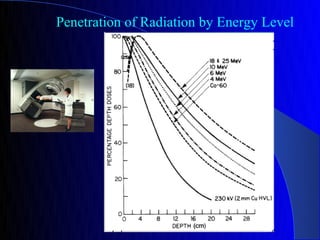
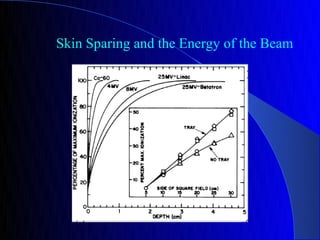
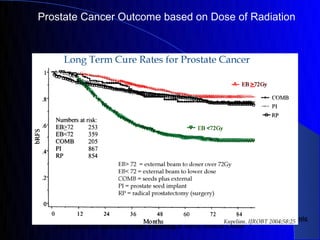
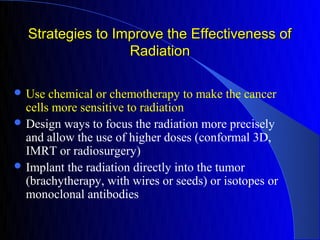
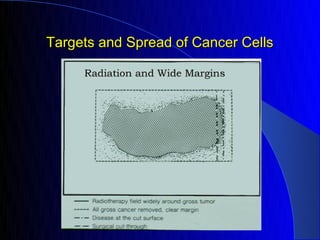
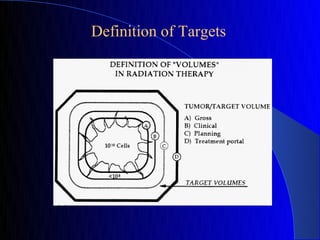
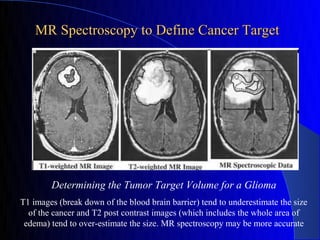
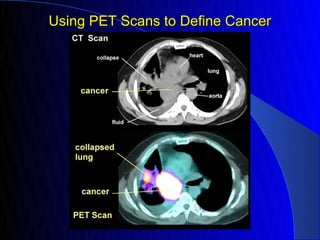
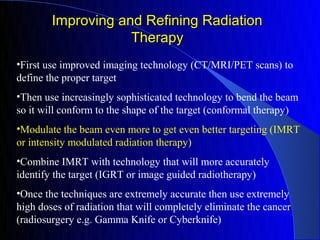
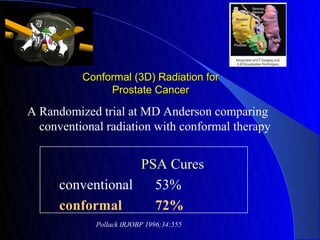
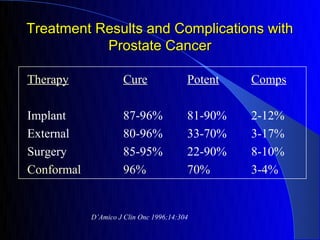
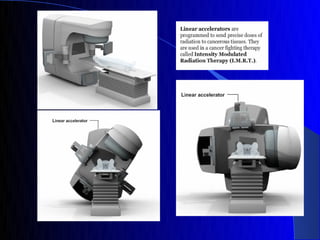
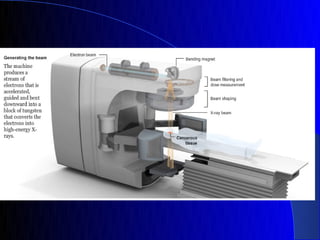
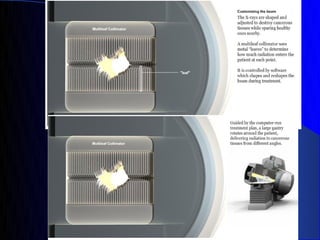
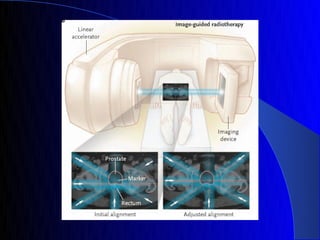
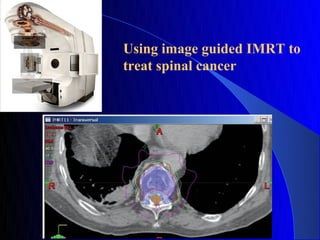
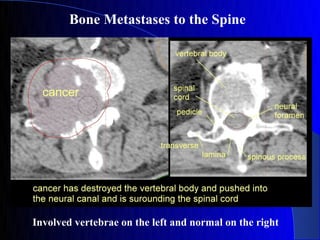
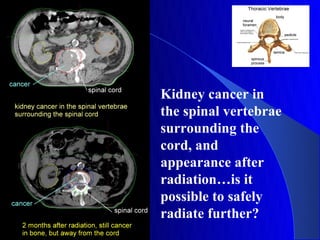
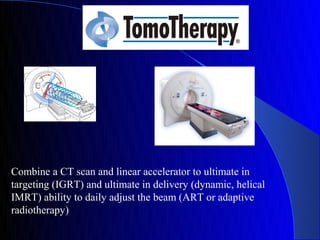
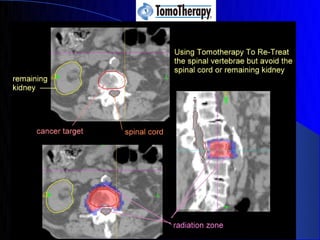
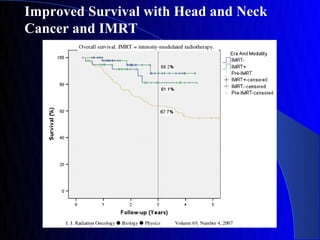
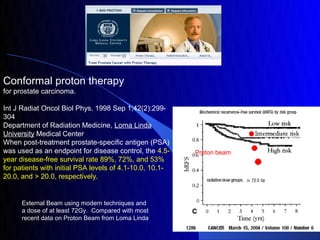
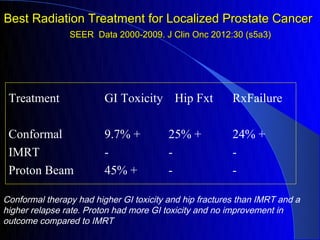
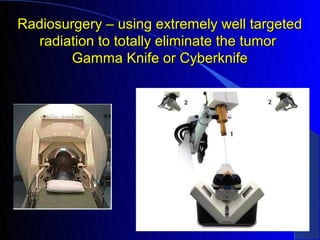
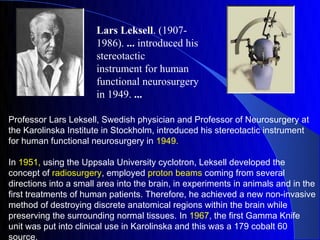
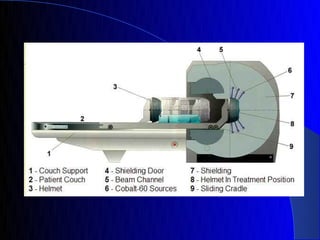
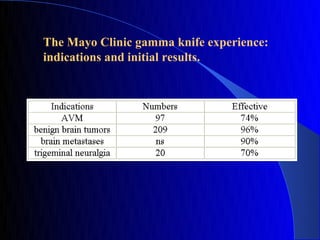
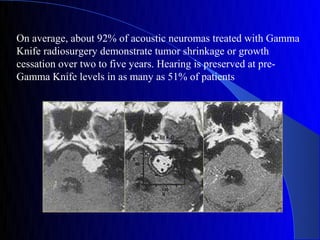
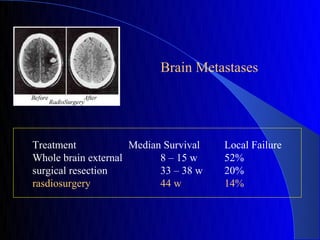
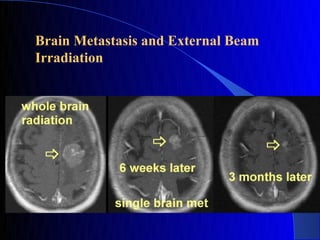
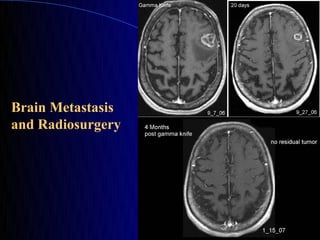
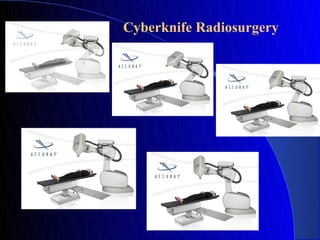
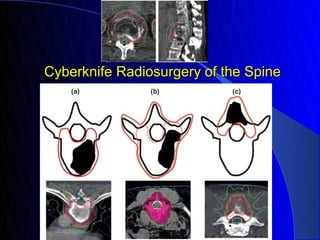
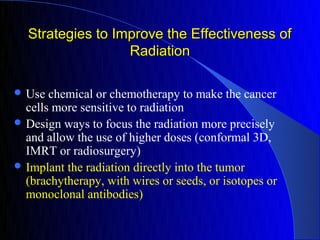
This document discusses the evolution of radiation therapy from its discovery in the late 19th century to modern techniques. It traces developments such as the discovery of x-rays and radioactivity, early radium and x-ray therapies, and the introduction of cobalt-60 and linear accelerators to improve targeting ability. Modern advances discussed include intensity-modulated radiation therapy (IMRT), image-guided radiation therapy (IGRT), proton beam therapy, and radiosurgery techniques like Gamma Knife and Cyberknife which allow extremely precise high dose radiation treatments.