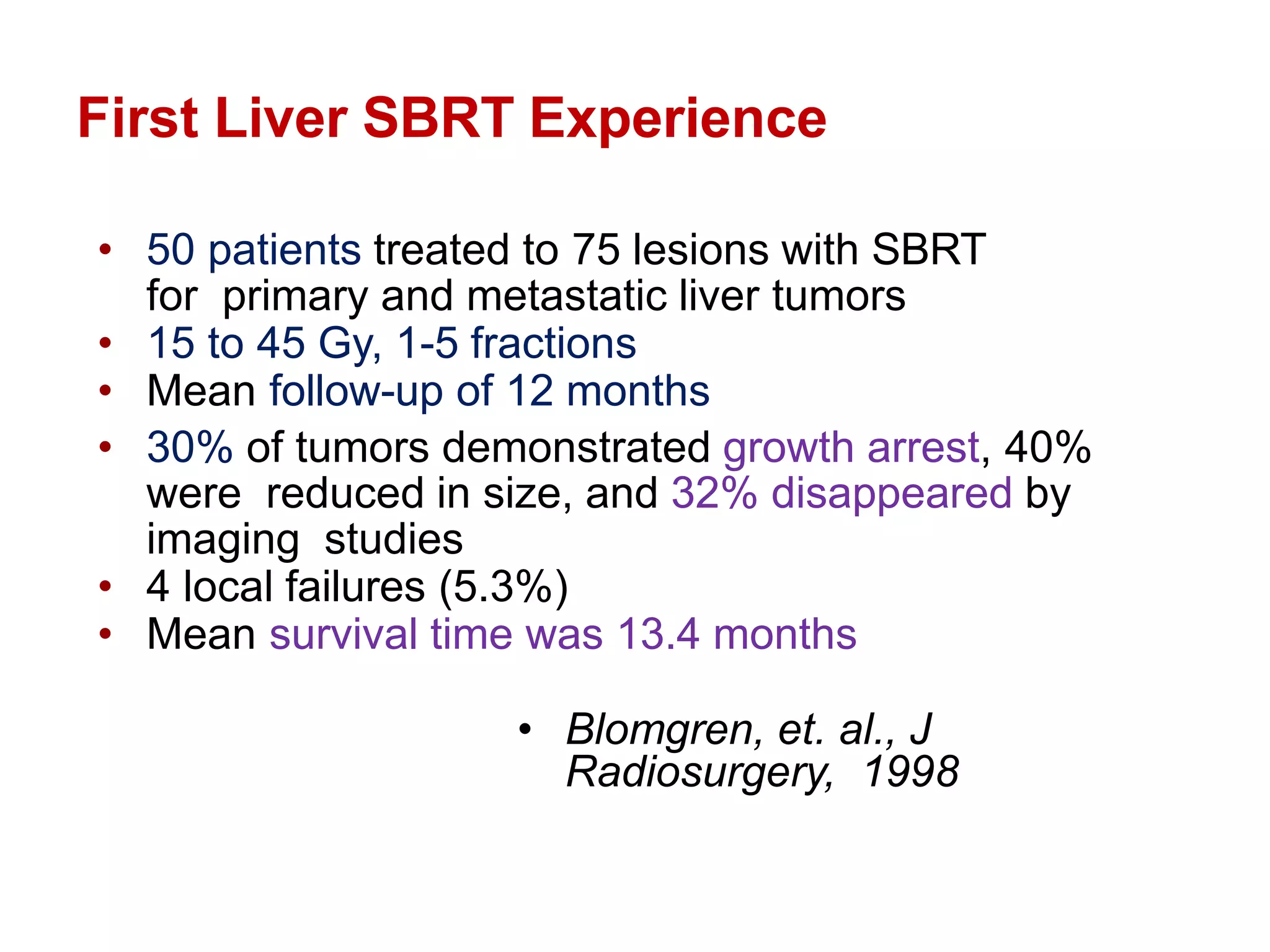
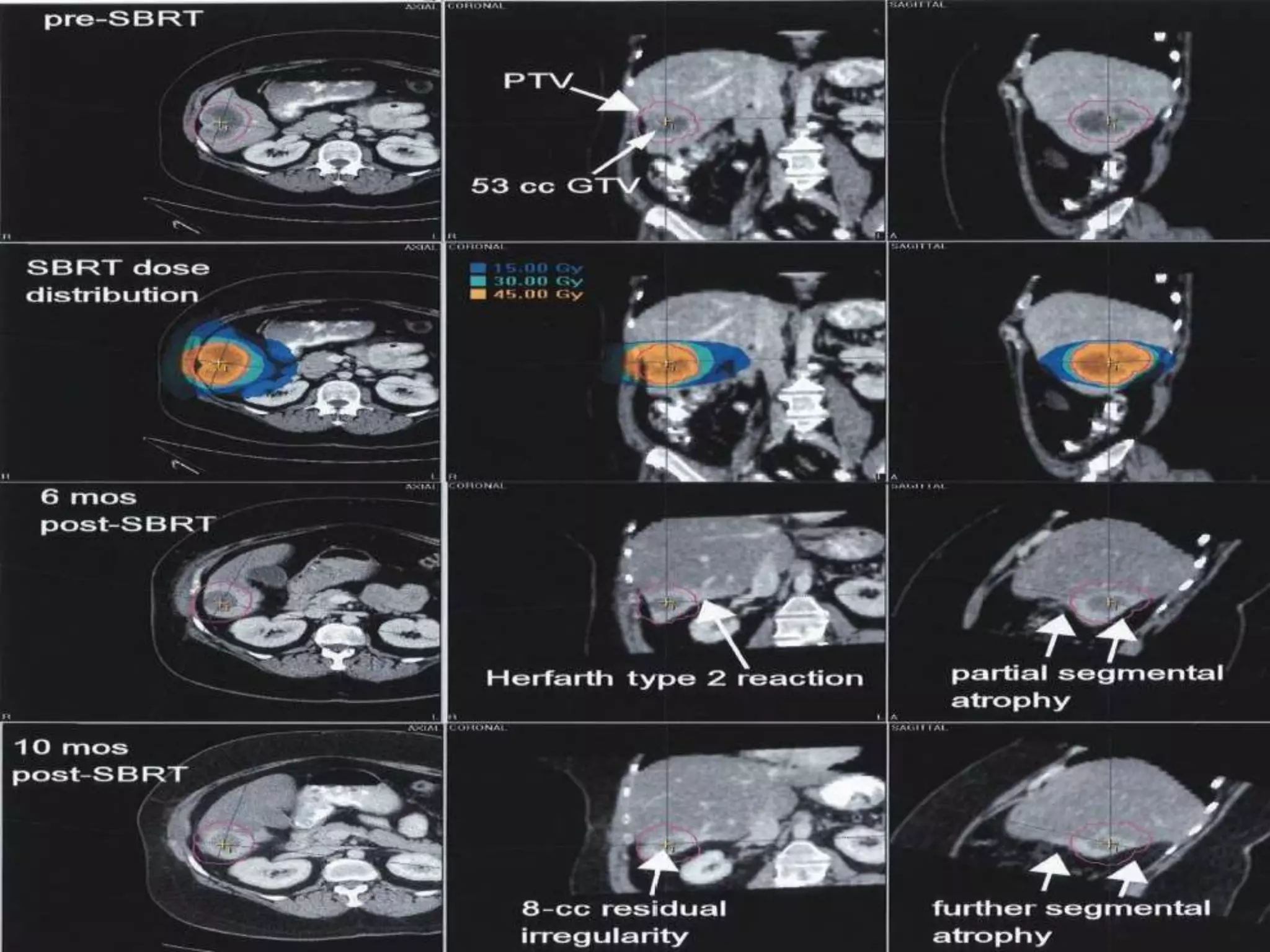
This document provides an overview of stereotactic body radiotherapy (SBRT). It begins with the history and introduction of SBRT, explaining how it differs from other radiotherapy modalities. It describes how SBRT works through its biological effects on tumor cells and blood vessels. Simulation, planning, patient immobilization and motion management are discussed. Common SBRT dose fractions and indications for various tumor sites are summarized, including lung, liver, spine, prostate and pancreas. Key challenges and dose constraints for each site are highlighted.