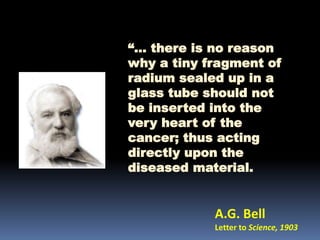
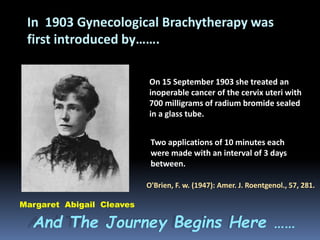
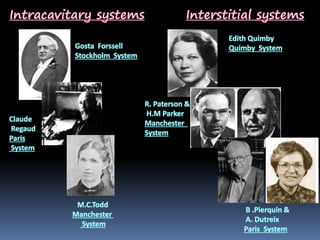
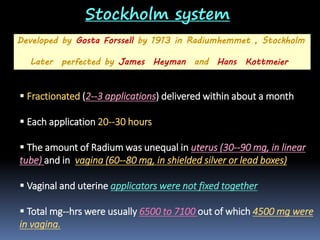
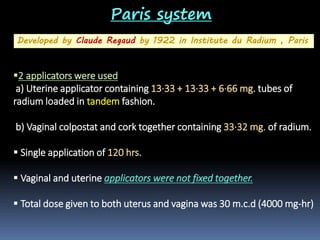
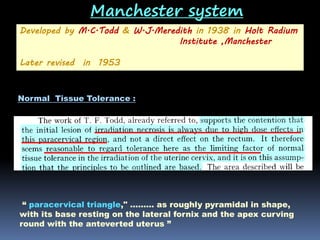
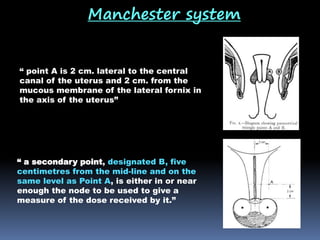
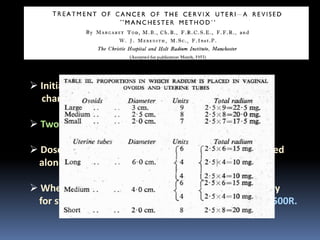
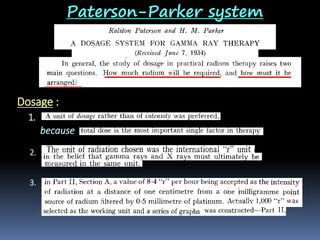
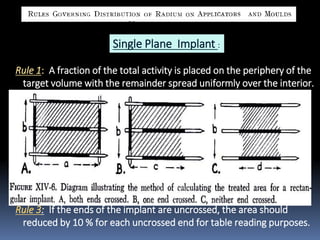
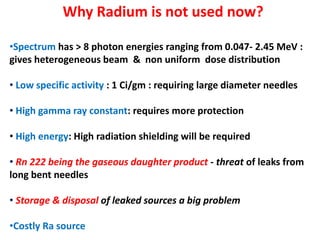
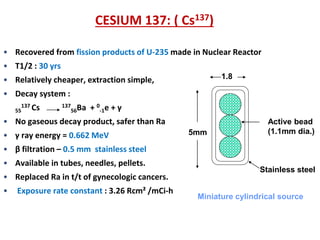
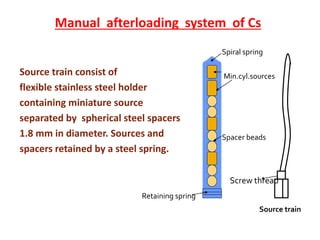
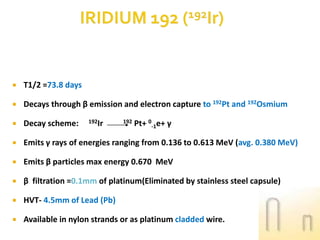
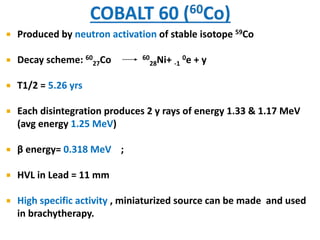
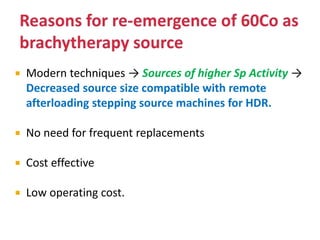
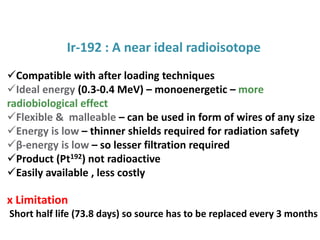
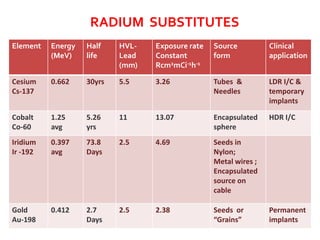
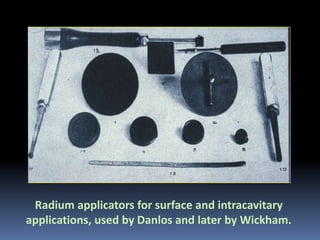
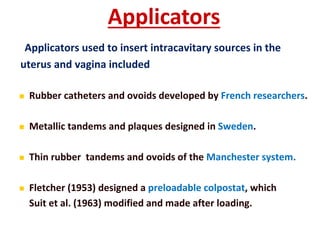
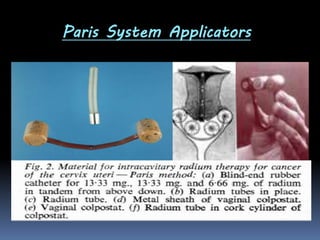
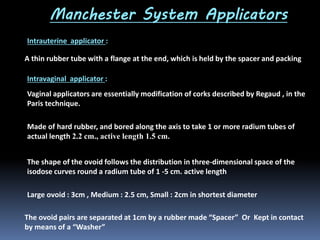
This document provides a historical overview of brachytherapy and the evolution of radiation sources used. It discusses some of the early discoveries in x-rays and radioactivity in the 1890s. It then describes some of the early uses of radium to treat skin lesions and cervical cancer in the early 1900s. The document outlines several early brachytherapy systems developed between 1913-1953, including the Stockholm, Paris, Manchester, and Paterson-Parker systems. It also discusses the introduction of the Quimby system using radium needles. The document notes the evolution of brachytherapy sources over time from radium to cesium-137 to iridium-192 to improve dosimetry, specific activity,