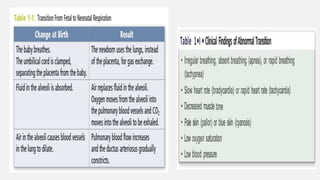
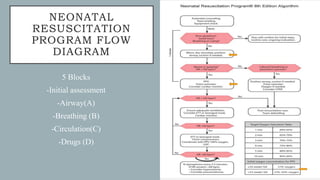
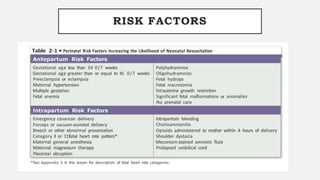
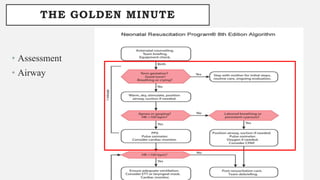
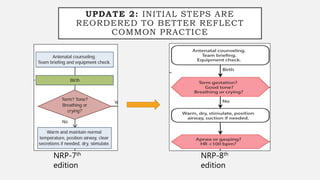
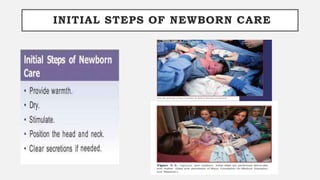
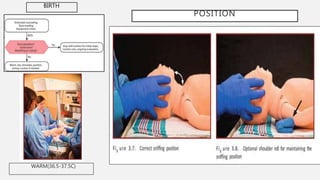
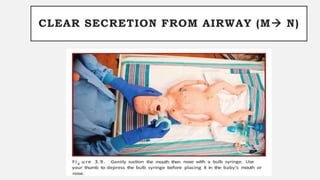
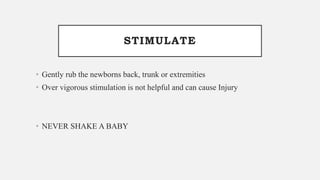
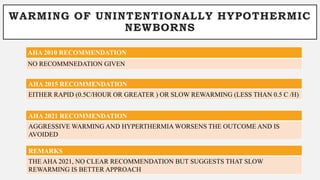
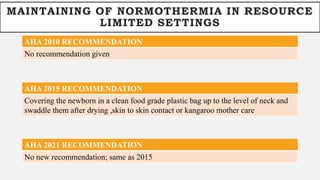
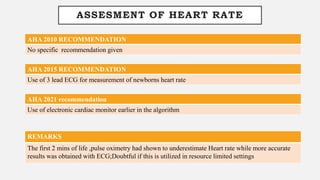
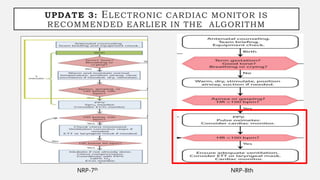
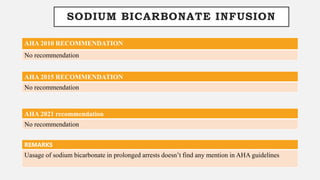
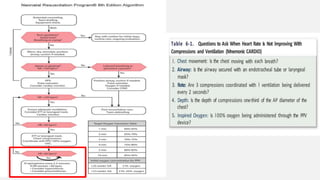
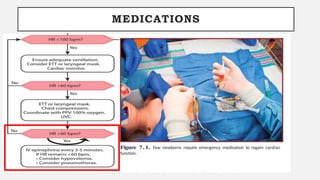
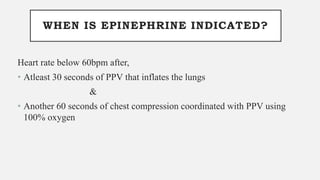
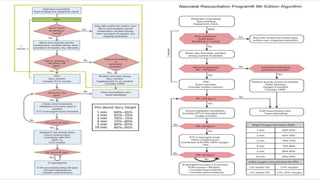
1. The document discusses updates to the Neonatal Resuscitation Program 8th edition, including changes to initial steps, umbilical cord management, temperature management, use of alternative airways, assessment of heart rate, and administration of medications like epinephrine.
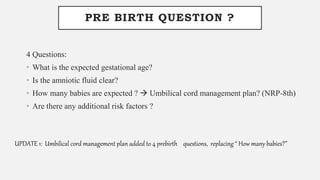
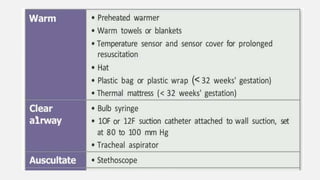
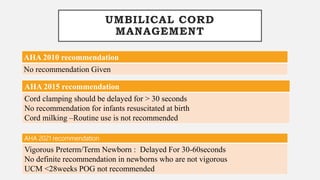
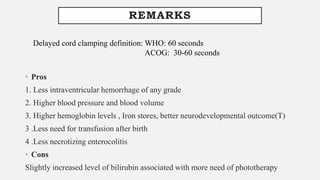
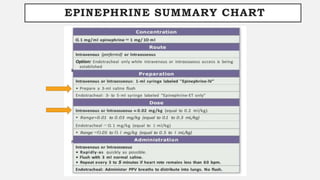
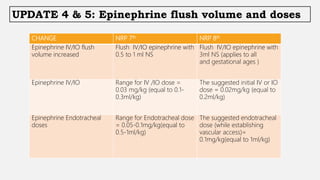
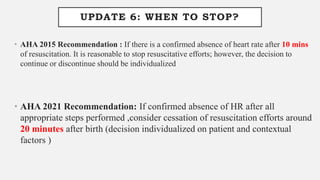
2. Key updates include reordering initial steps, recommending delayed umbilical cord clamping for at least 30-60 seconds, use of electronic cardiac monitors earlier, and changes to epinephrine flush volumes and doses.
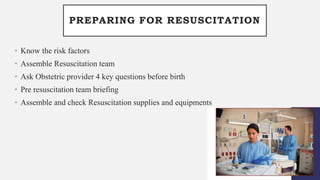
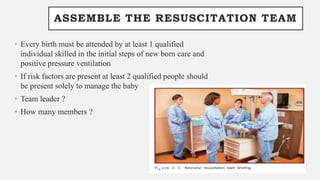
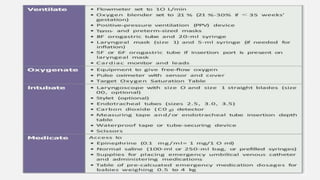
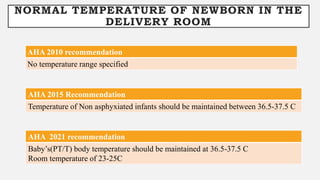
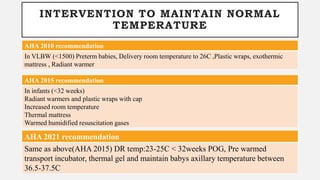
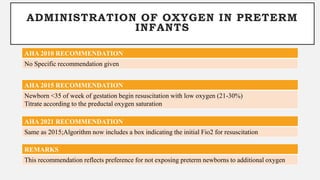
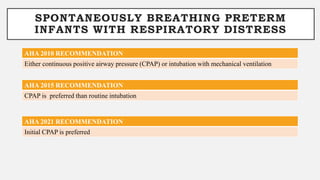
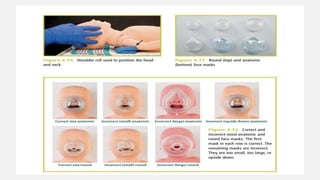
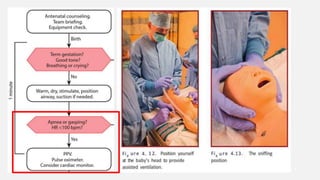
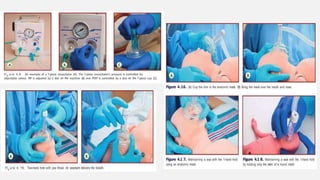
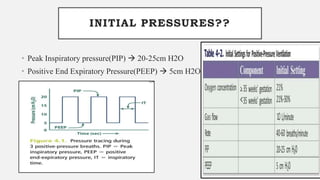
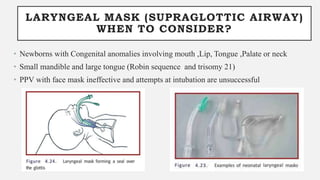
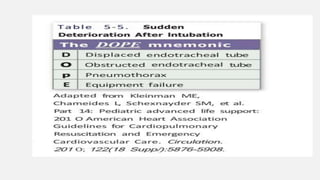
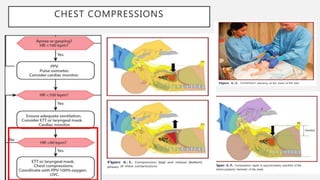
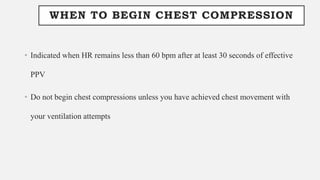
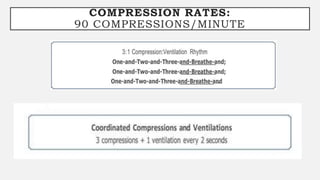
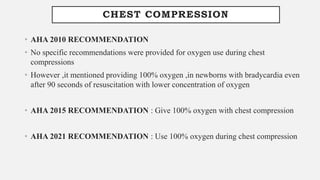
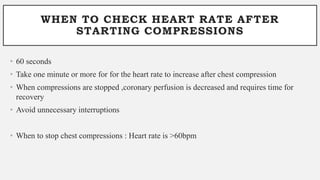
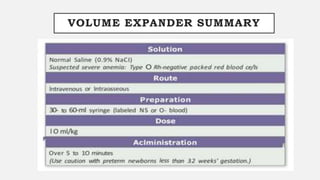
3. The presentation reviews various aspects of newborn resuscitation including preparation, assessment, ventilation, chest compressions, and medications in line with the latest American Heart Association guidelines.