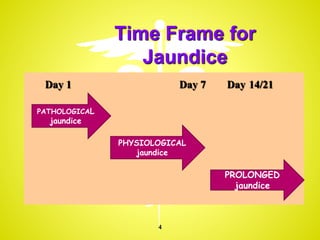
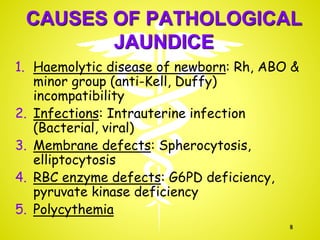
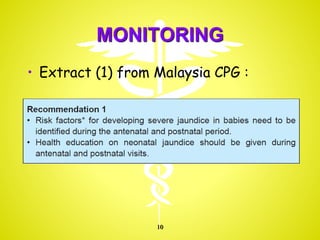
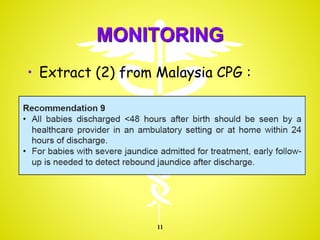
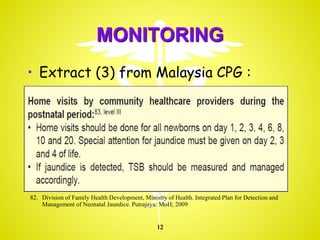
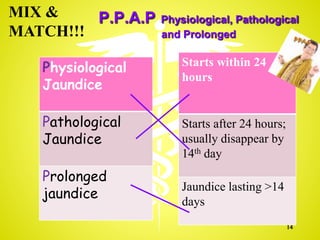
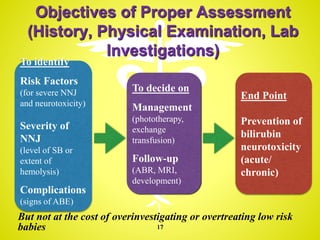
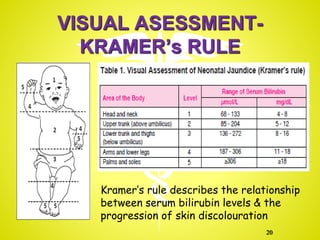
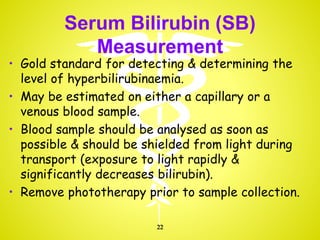
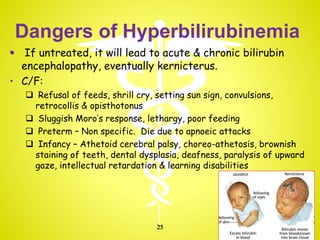
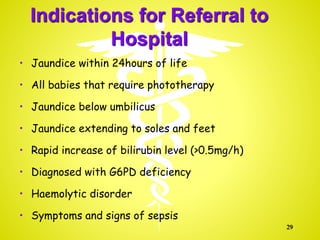
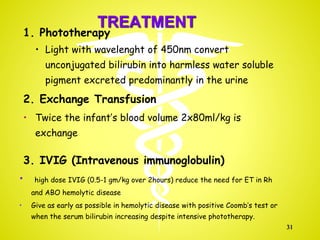
Neonatal jaundice is one of the most common conditions in newborns. It is caused by high levels of bilirubin in the blood which causes yellowing of the skin. Physiological jaundice is common and appears after 24 hours, peaks by days 3-5, and resolves by 14 days without treatment. Pathological jaundice appears within 24 hours and requires treatment. Proper assessment includes history, physical exam, and lab tests to determine severity and risk of complications like acute bilirubin encephalopathy. Treatment may include phototherapy or exchange transfusion in severe cases. Close monitoring is important to prevent bilirubin neurotoxicity in newborns.