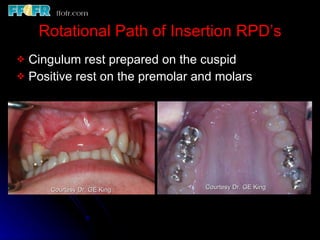
This document summarizes information from a lecture on removable partial dentures (RPDs), attachments, and rotational path RPDs. It discusses the advantages and disadvantages of different types of attachments, including ERA attachments, magnetic attachments, and overlay dentures. It also describes rotational path RPDs and lateral rotational path RPDs, highlighting how they can eliminate visible clasps while providing retention and stability. Examples are provided of different RPD designs incorporating various attachments and rotational paths of insertion.