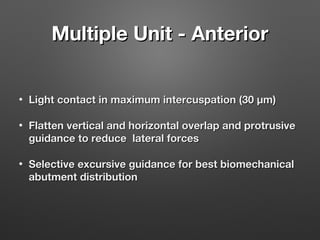
This document summarizes key concepts regarding occlusion for implant-supported fixed dental prostheses. It notes that unlike natural teeth which have periodontal ligaments to absorb forces, implants lack this and forces are concentrated at the crestal bone. As such, implant occlusion schemes aim to reduce bending moments and distribute forces axially. Recommendations include using flat fossa and grooves, narrow occlusal tables, reduced cuspal inclines, stiffer materials, and avoiding excursive contacts to protect the implant and surrounding bone.