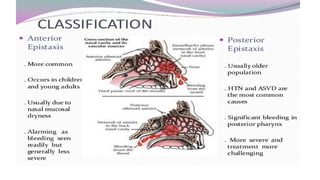
Epistaxis, or nosebleeding, is a common condition that can affect individuals of all ages, often originating from the anterior nasal cavity due to the rupture of small blood vessels. It is classified into anterior epistaxis, which is more prevalent and easier to manage, and posterior epistaxis, which is less common but more severe and often requires hospitalization. Management involves determining the bleeding site, applying direct pressure, and employing treatments like vasoconstrictors or nasal packing, with careful monitoring for potential complications.