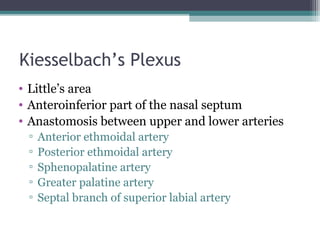
Epistaxis, or nosebleed, occurs due to the unique anatomy of the nasal cavity and is classified into anterior and posterior types, with anterior being more common. Management includes identifying the cause, controlling bleeding, and various interventions like nasal packing and cauterization, with surgical interventions considered in persistent cases. Preventive measures focus on controlling underlying conditions and maintaining nasal moisture.