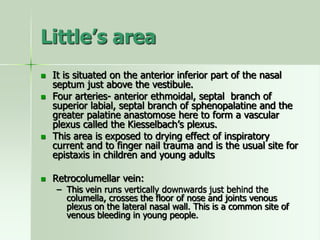
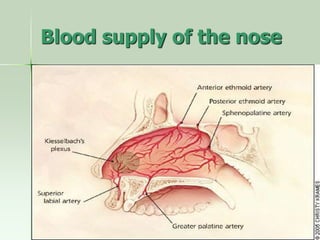
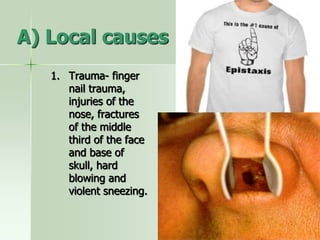
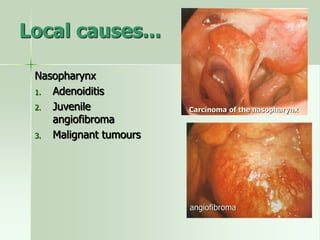
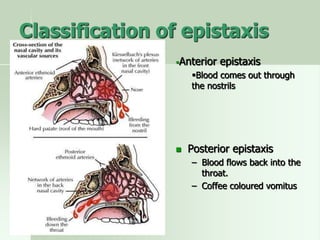
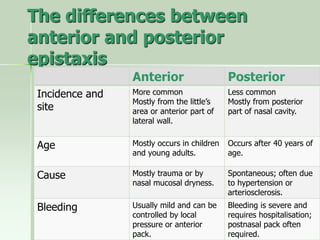
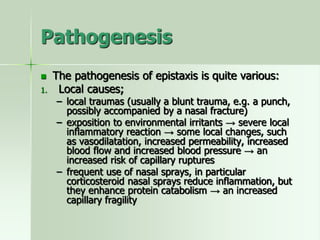
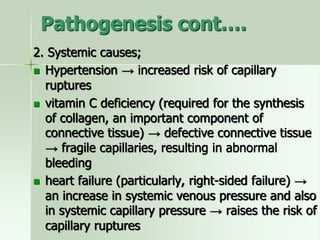
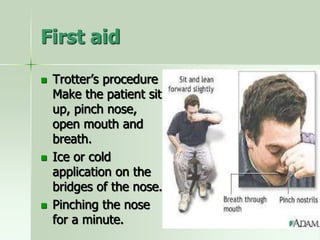
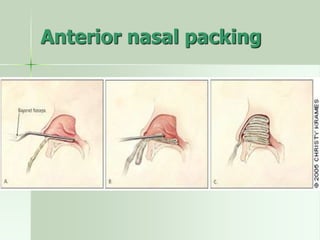
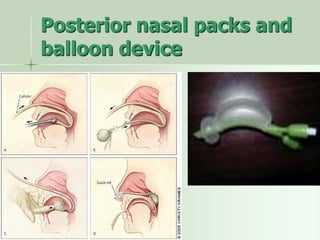
Epistaxis, or nosebleed, is bleeding from the nose or nasal cavity. It is common and can occur at any age. The nose has a highly vascularized mucosa to warm and humidify air, placing it at risk for bleeding from minor trauma or irritation. The anterior septum area called Little's area is a common site of epistaxis due to its anastomosis of arteries. Epistaxis can be anterior, bleeding visible in the nose, or posterior, bleeding draining back internally. Management involves cauterization, nasal packing, or ligation of arteries in severe cases.