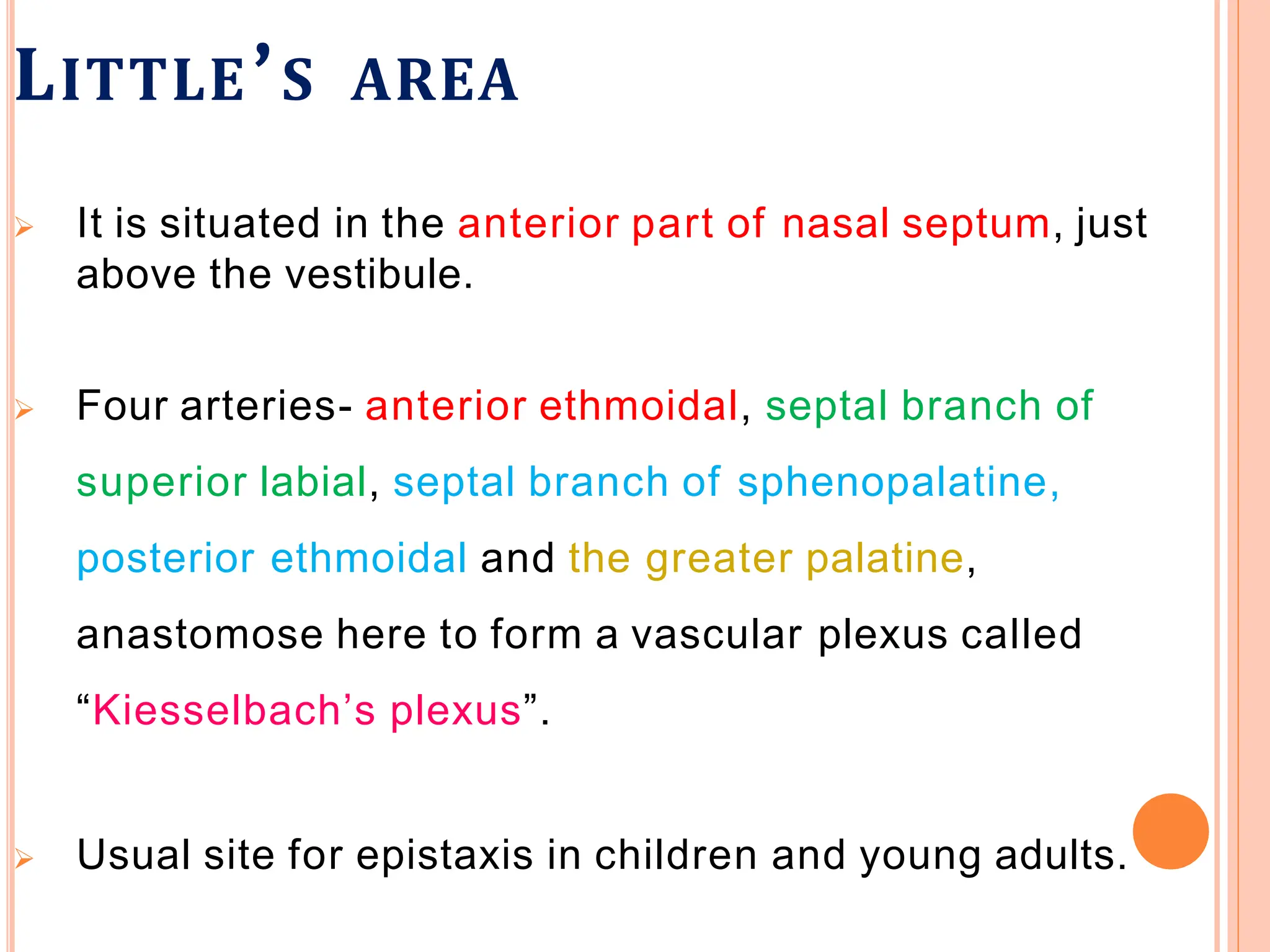
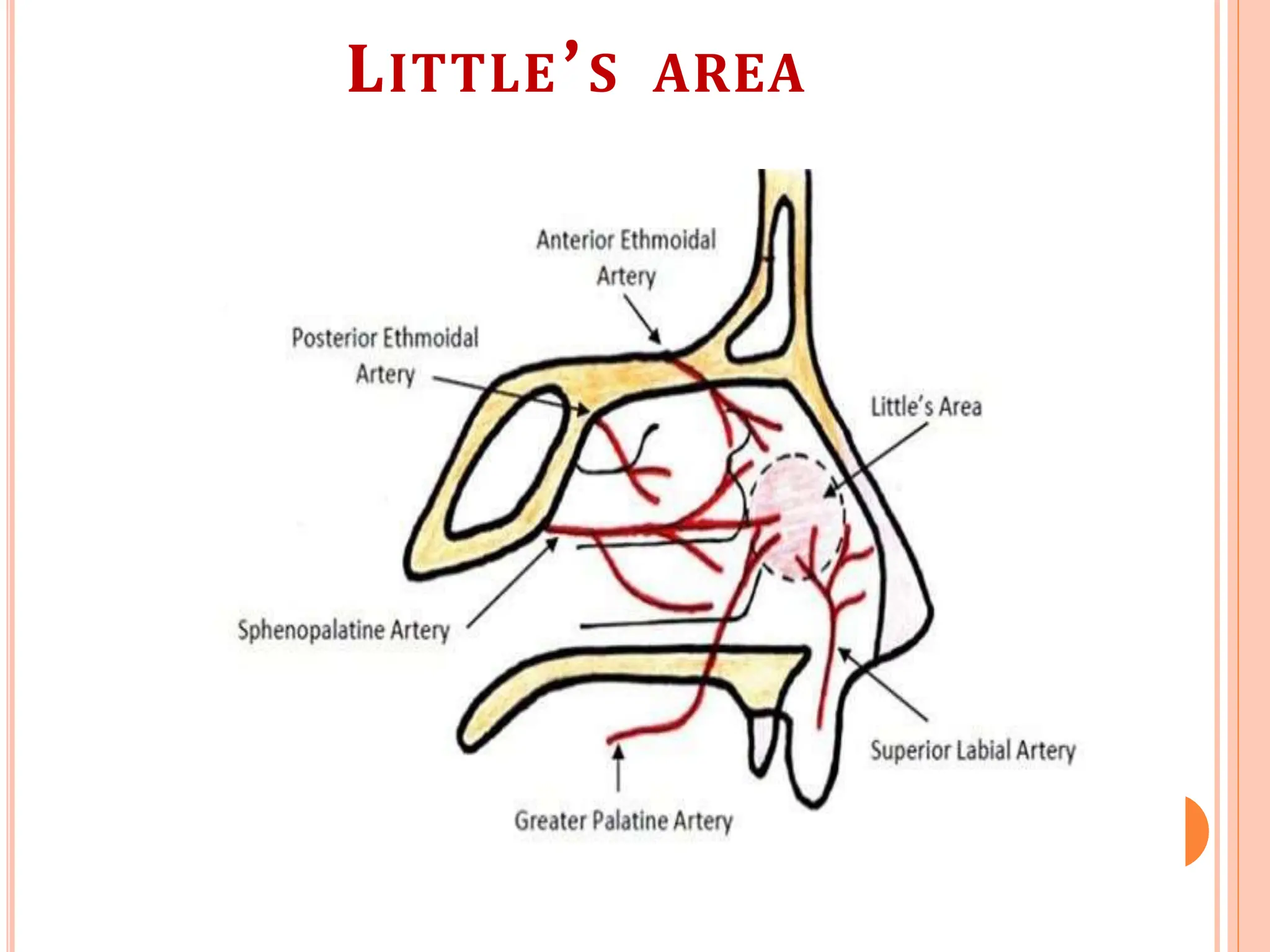
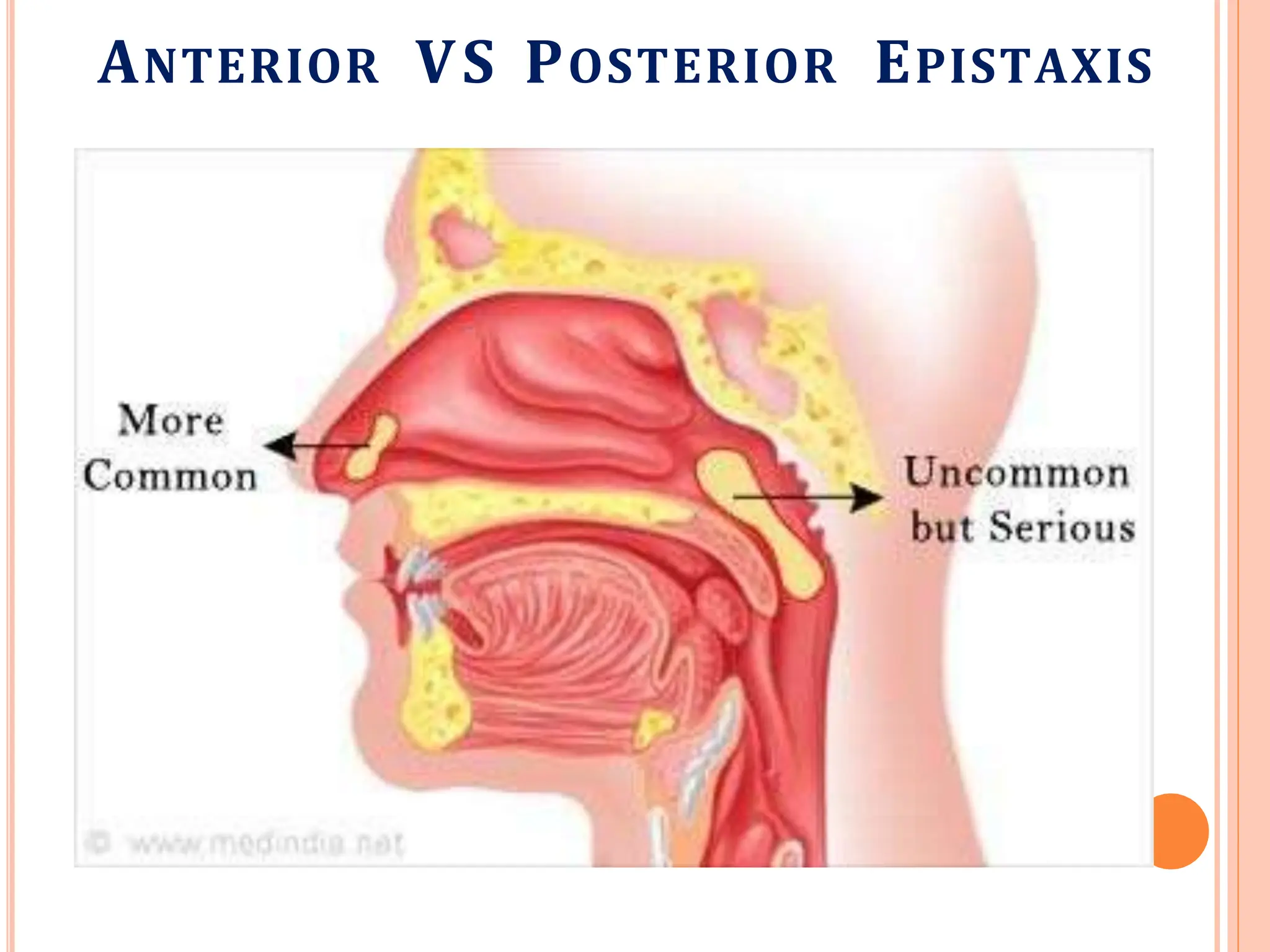
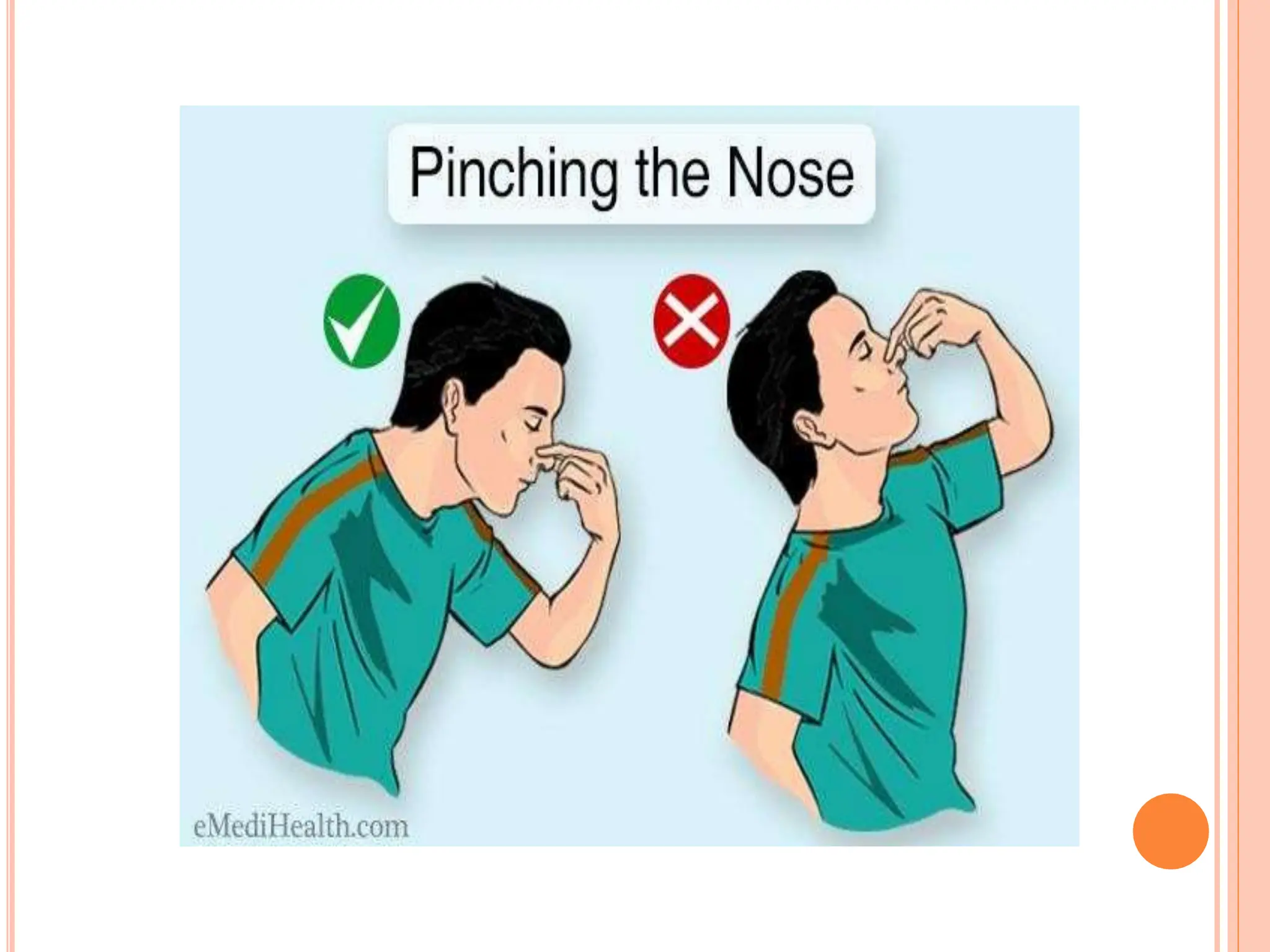
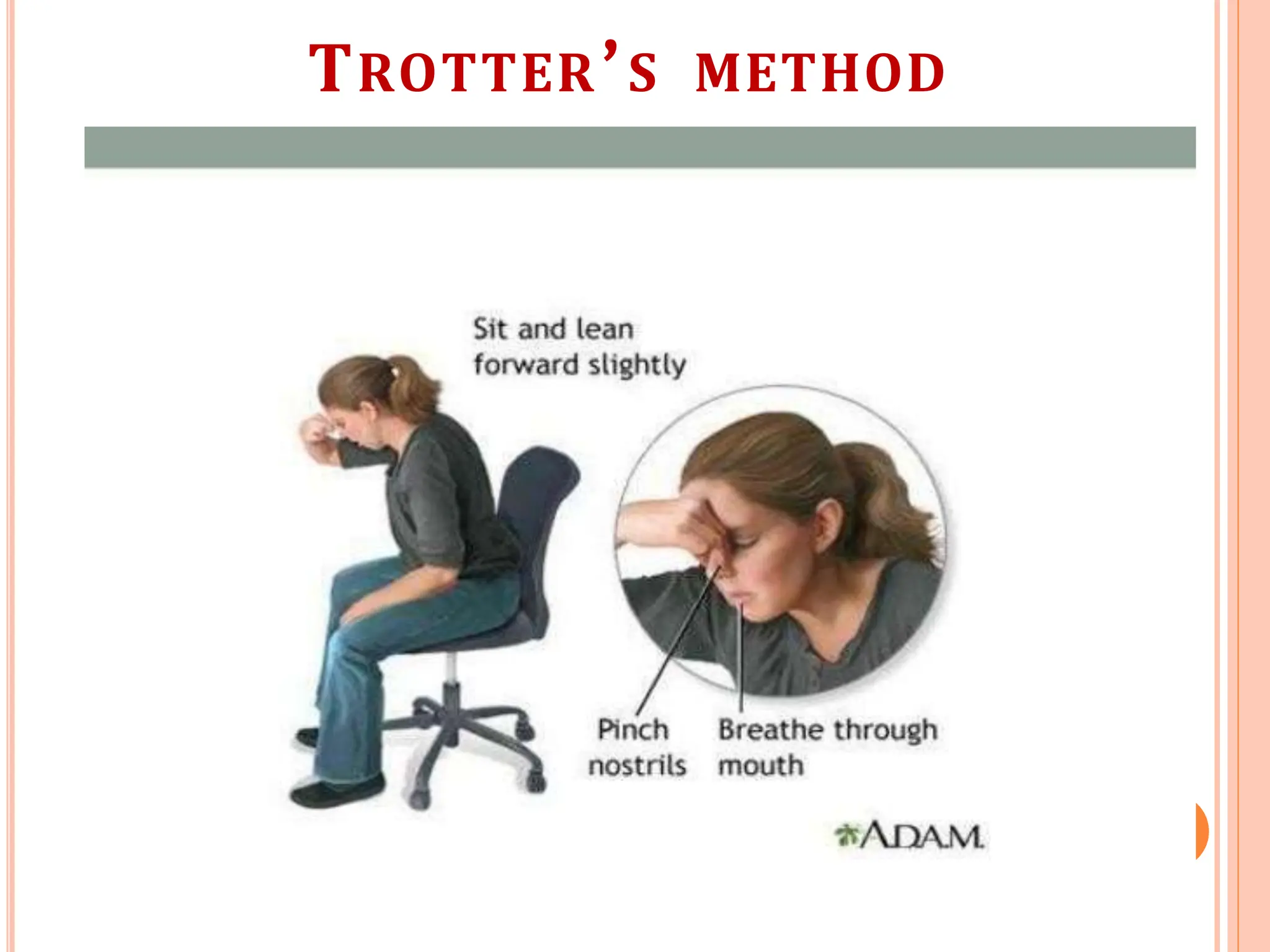
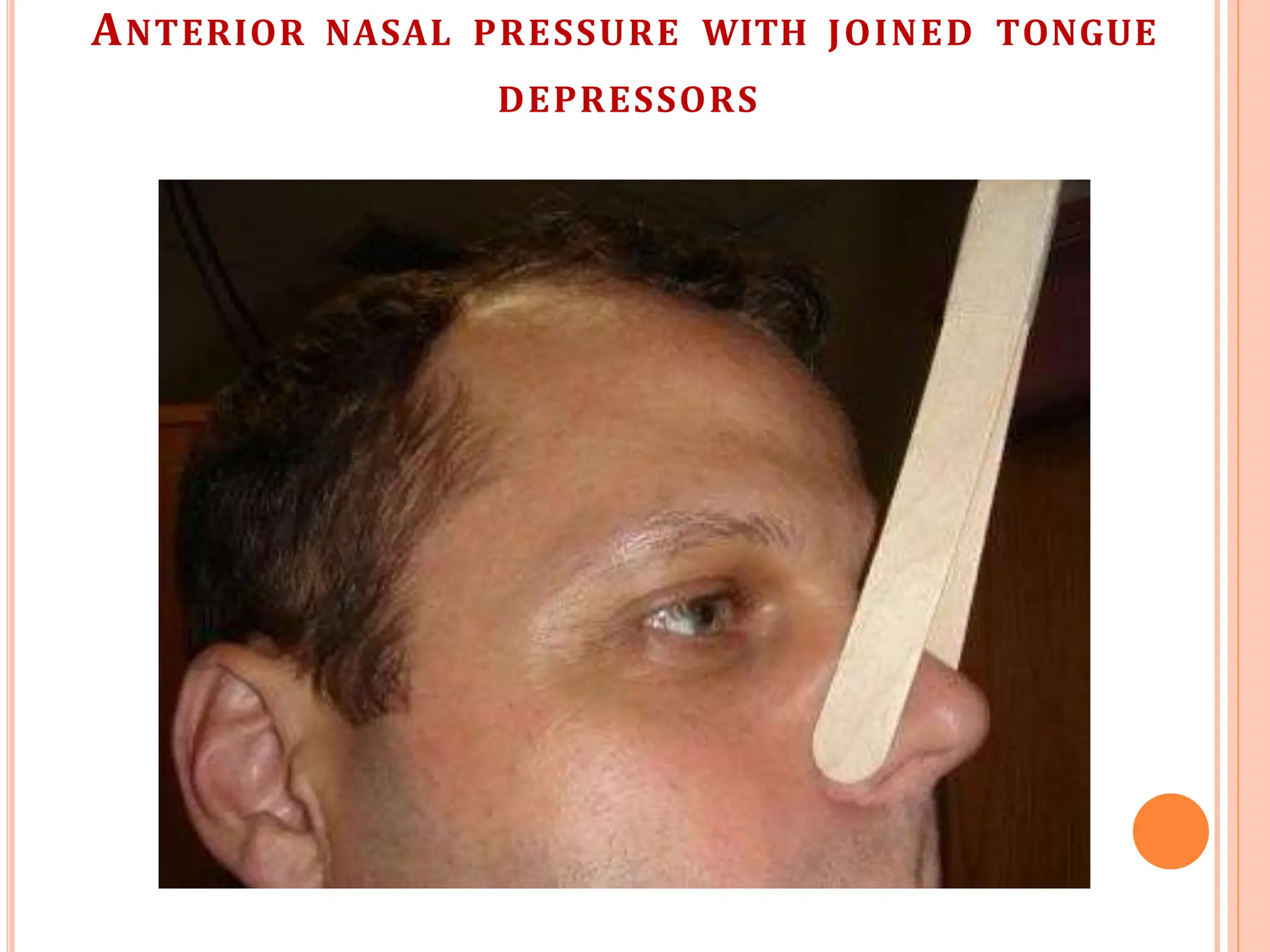
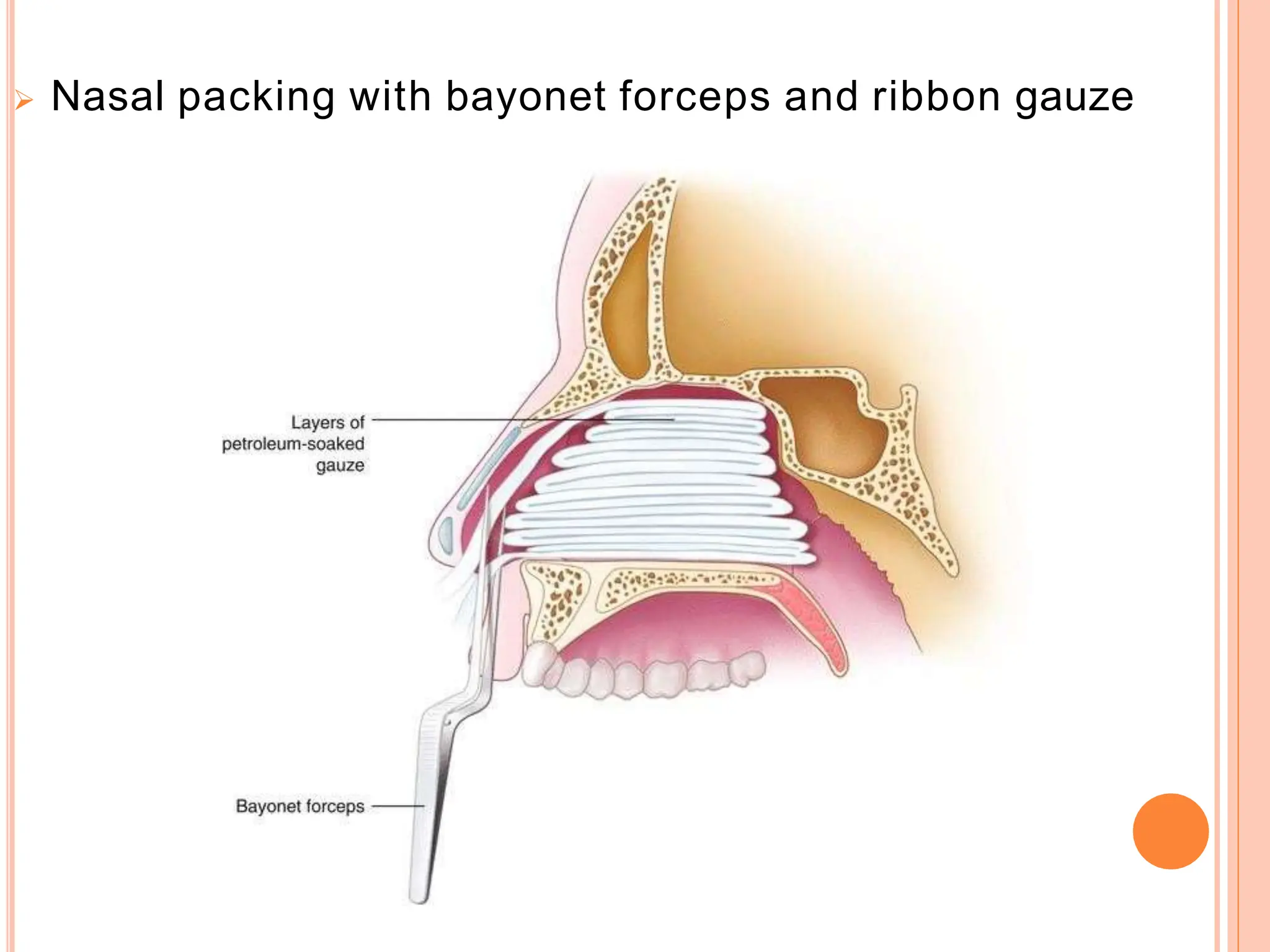
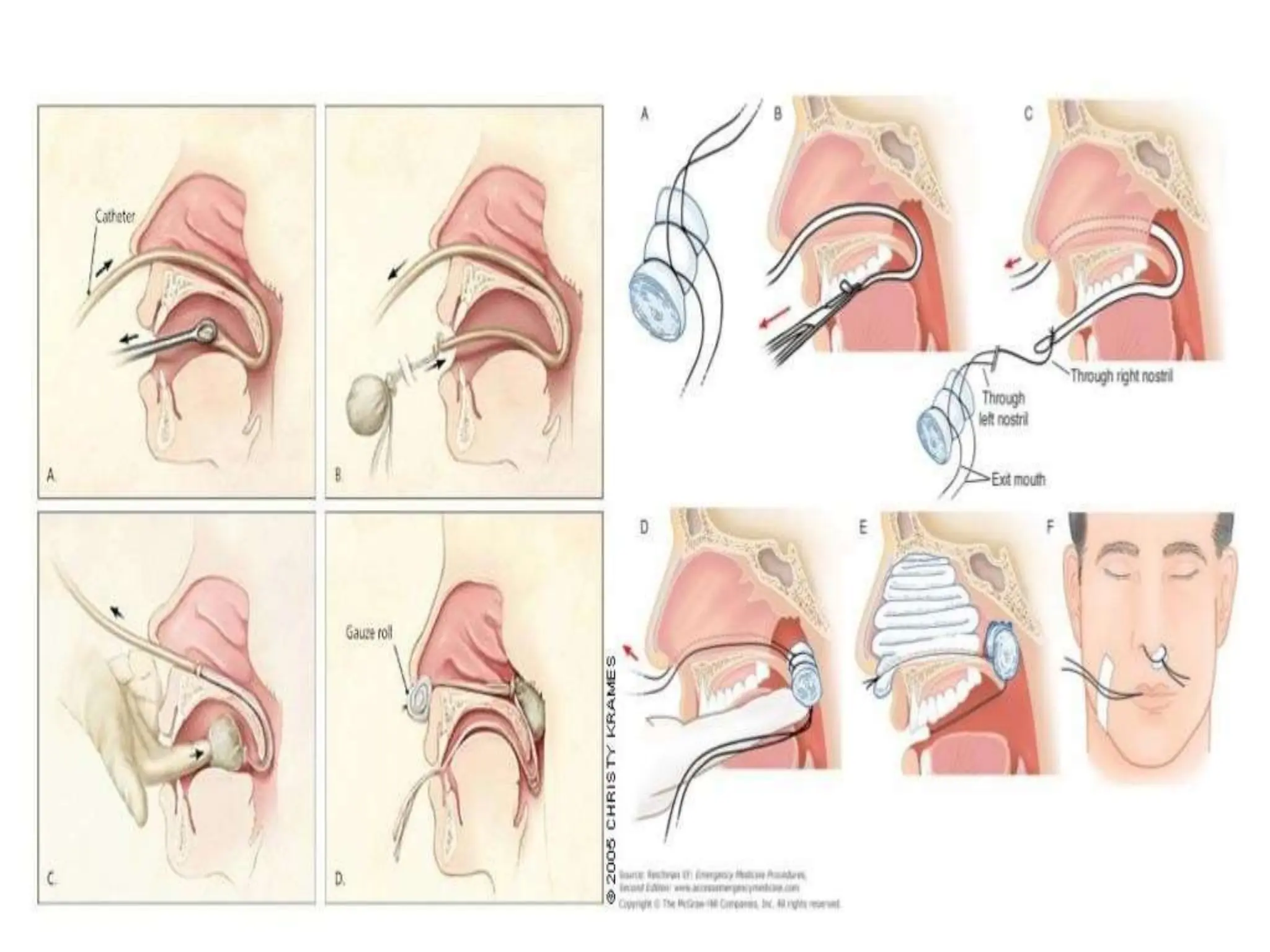
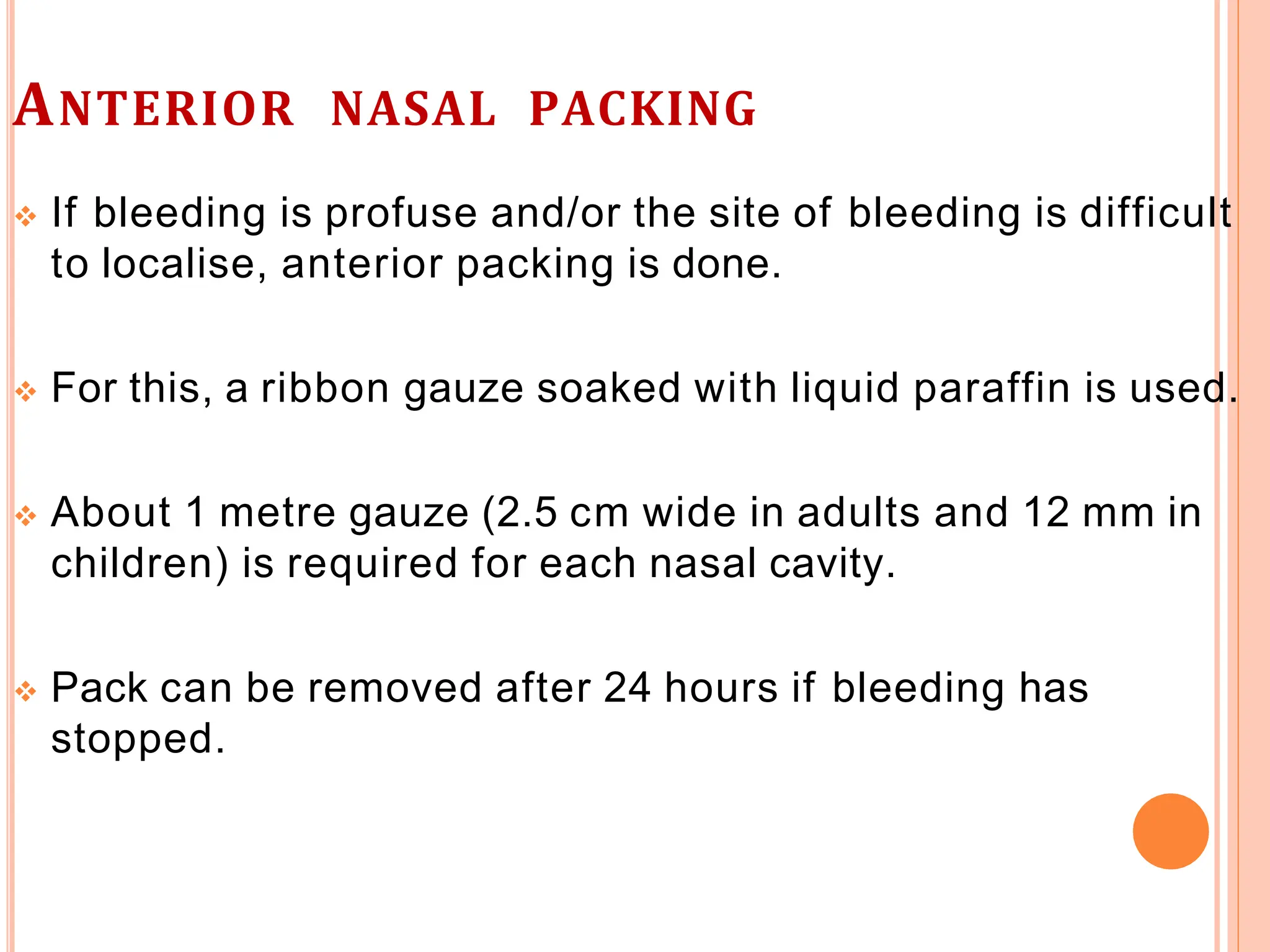
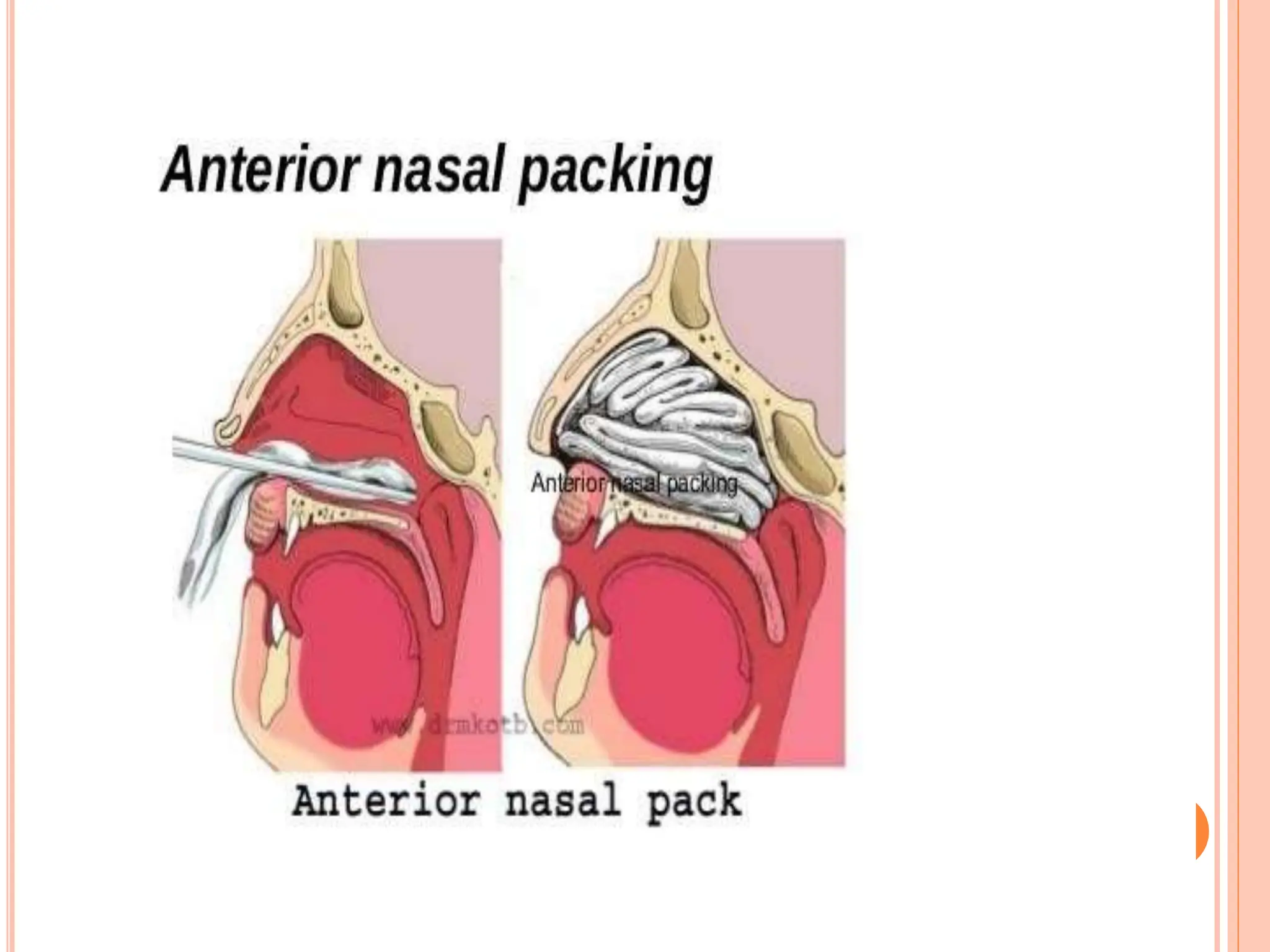
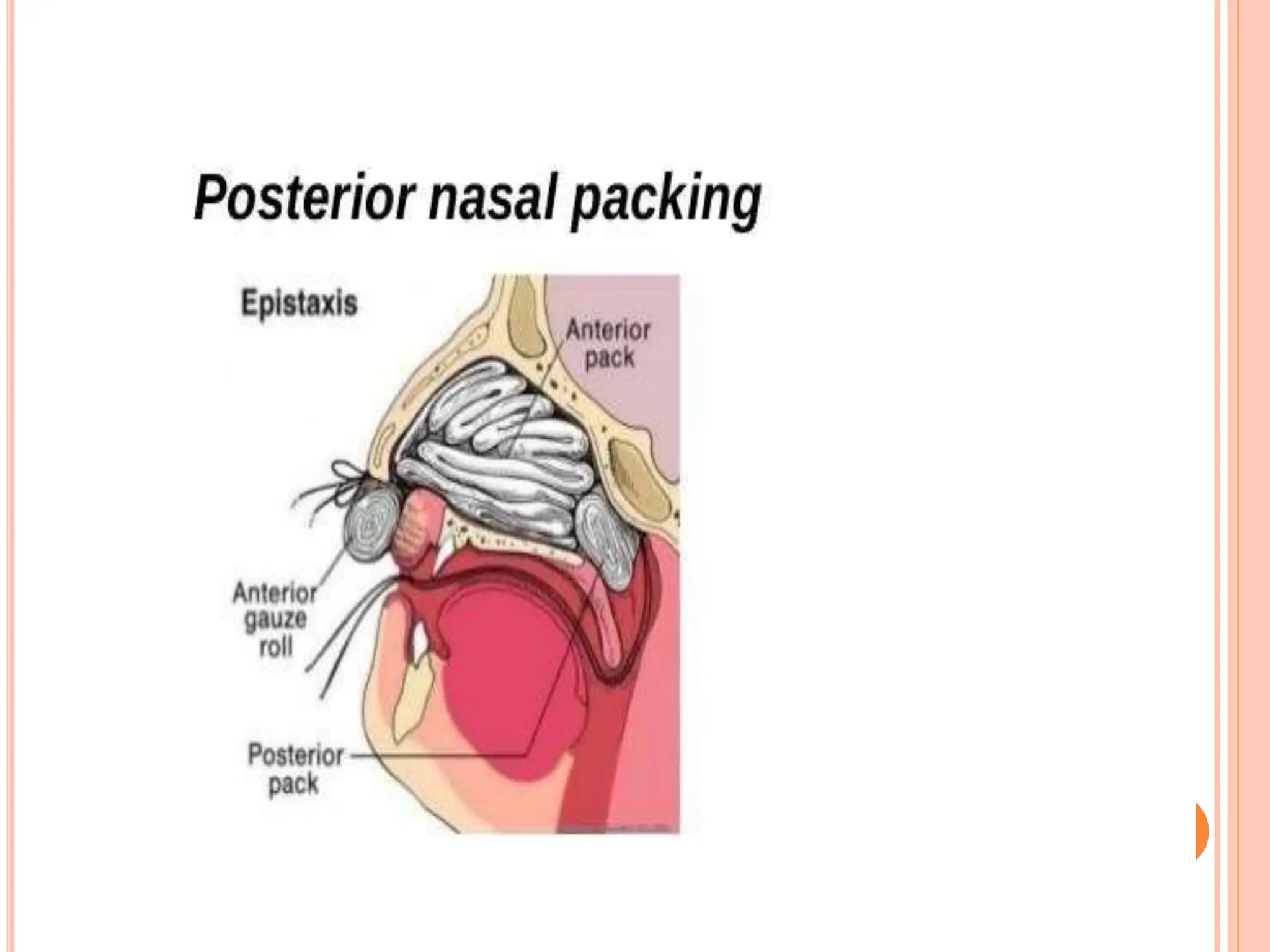
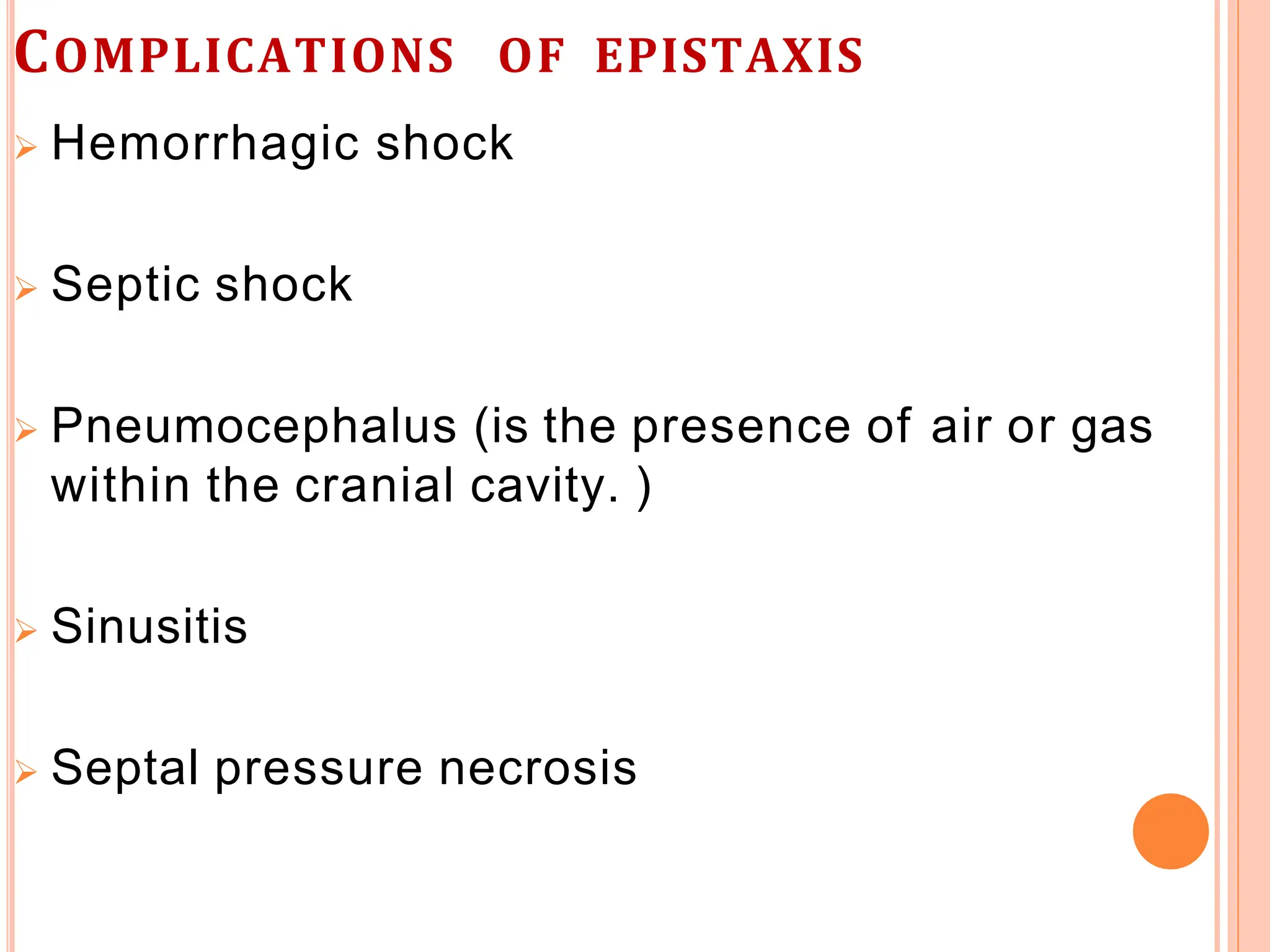
Epistaxis, or nosebleed, is commonly caused by the rupture of small blood vessels in the nasal mucosa, with Little's area being a frequent site for anterior epistaxis, primarily in children. Treatment varies based on the type and severity, ranging from conservative methods like nasal compression to more invasive approaches such as cauterization or nasal packing. Complications can arise, including hemorrhagic shock and infection, necessitating careful patient management and education to prevent recurrence.