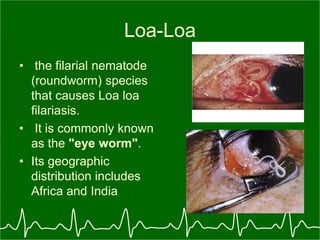
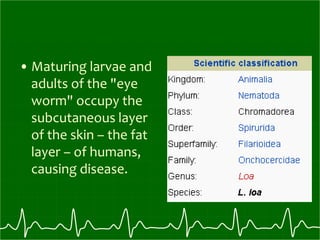
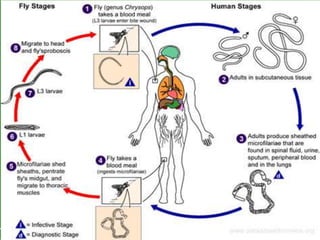
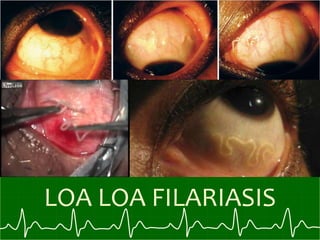
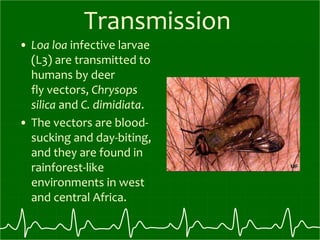
Loa loa, commonly known as the eye worm, is a parasitic filarial nematode transmitted by deer flies and mango flies. It causes loiasis or Calabar swelling in humans in parts of Africa and India. The adult worms live in subcutaneous tissues under the skin and can sometimes be seen moving under the eye or skin, giving it the name "eye worm". Microfilariae produced by the adult female worms can be found in blood, urine and other tissues. The life cycle involves transmission between humans and flies. Diagnosis is by finding microfilariae in blood samples and treatment involves diethylcarbamazine or ivermectin.