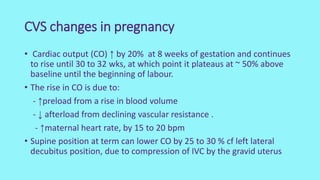
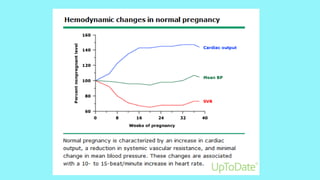
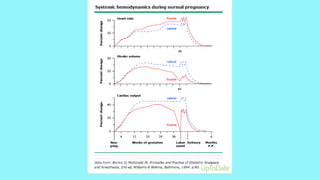
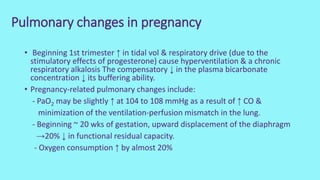
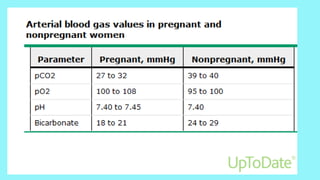
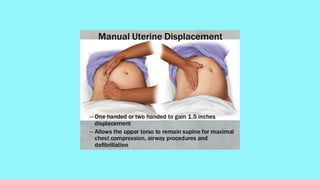
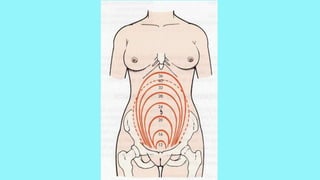
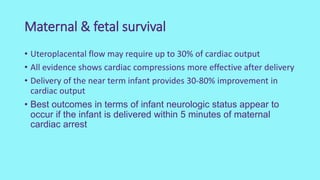
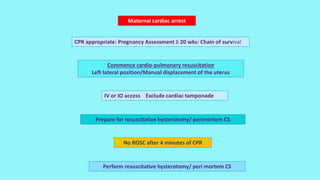
Cardiac output increases by 50% during pregnancy due to a rise in blood volume, decreased vascular resistance, and increased heart rate. Pulmonary changes include hyperventilation, upward displacement of the diaphragm reducing lung capacity by 20%, and increased oxygen consumption. Perimortem cesarean section improves maternal resuscitation by removing aortocaval compression and allowing blood to reperfuse the systemic circulation.