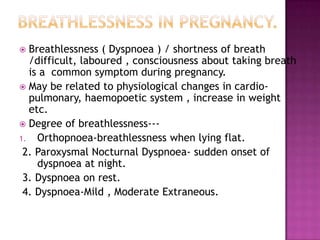
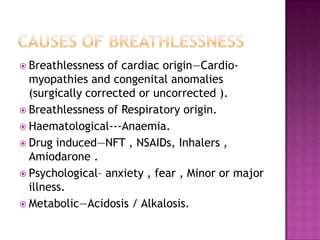
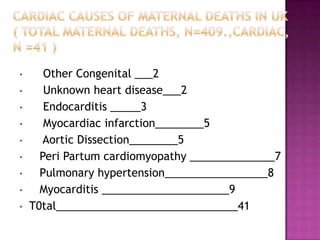
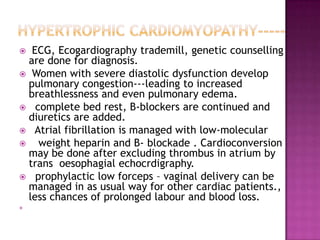
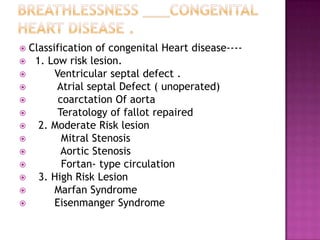
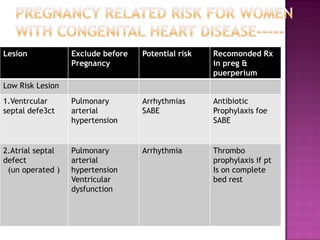
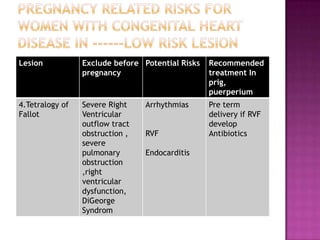
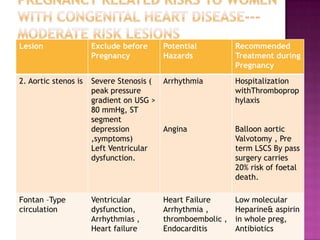
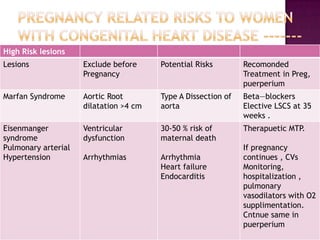
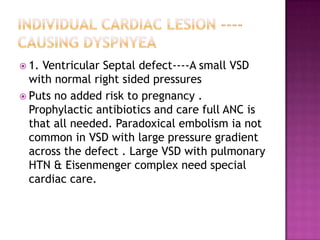
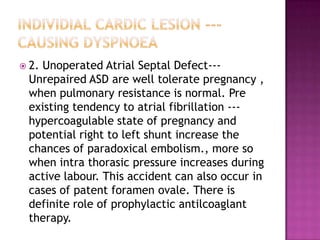
This document discusses various cardiac conditions that can cause breathlessness during pregnancy, including cardiomyopathies, congenital heart diseases, and other issues. It provides details on evaluating and managing common conditions like peripartum cardiomyopathy, dilated cardiomyopathy, hypertrophic cardiomyopathy, ventricular septal defects, and more. The document aims to help clinicians understand the potential risks these conditions pose during pregnancy and recommend appropriate treatment approaches.