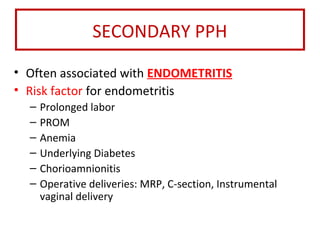
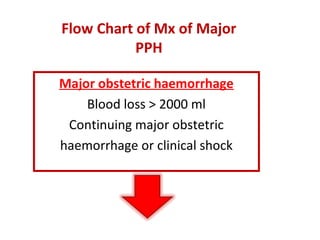
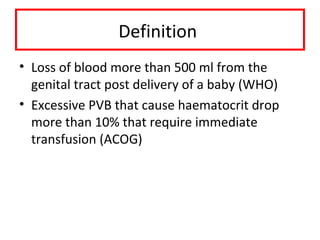
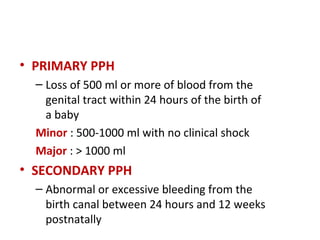
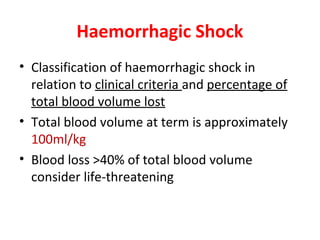
1. Postpartum haemorrhage (PPH) is defined as blood loss greater than 500 ml within 24 hours of delivery. It can be primary (within 24 hours) or secondary (24 hours to 12 weeks).
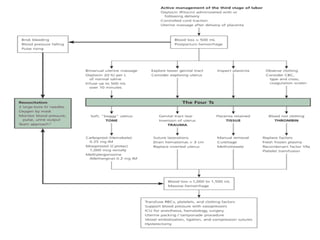
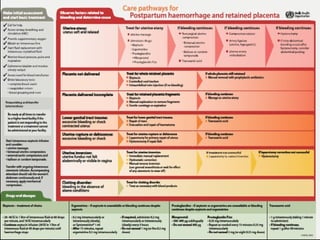
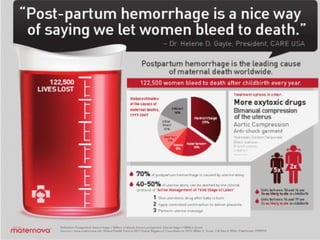
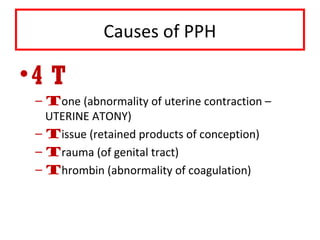
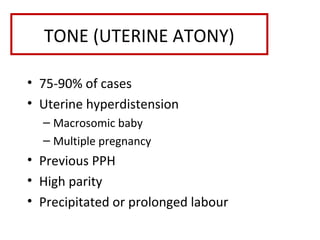
2. Causes of PPH include uterine atony, retained placenta, genital tract trauma, and coagulation disorders. Uterine atony accounts for 75-90% of cases.
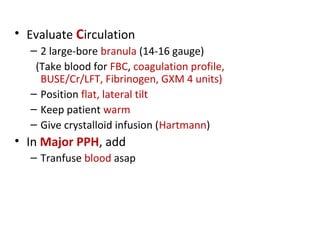
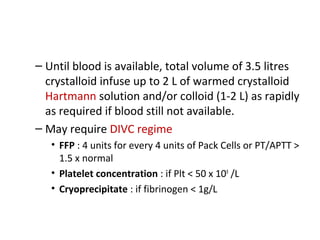
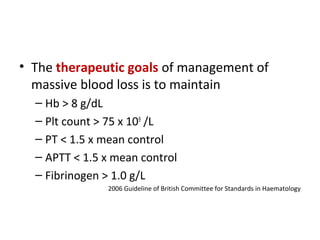
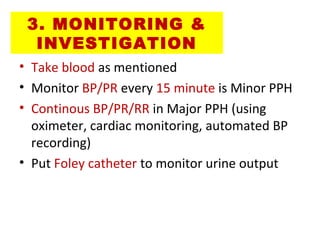
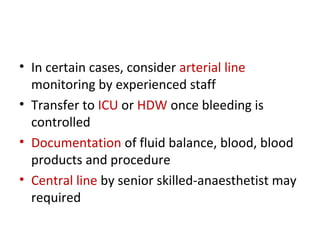
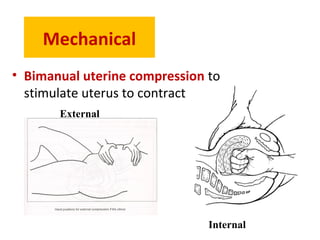
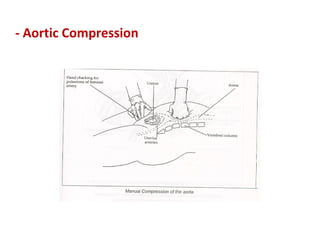
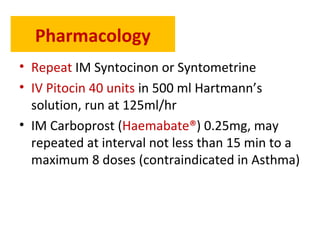
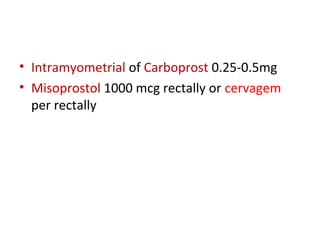
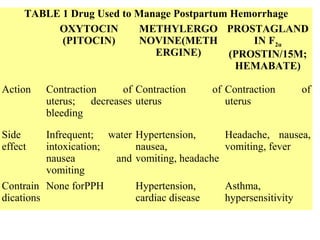
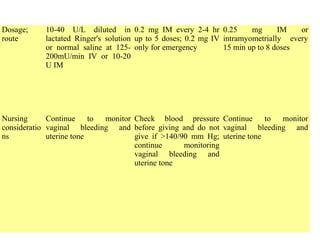
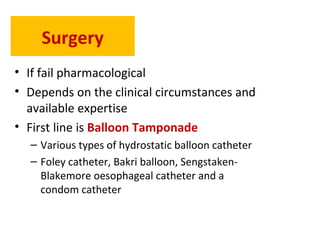
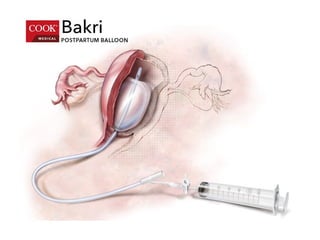
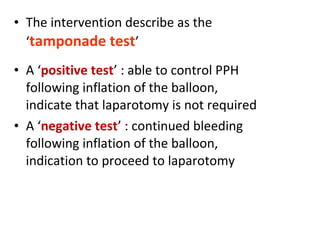
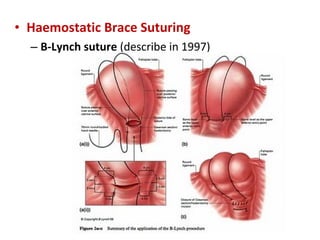
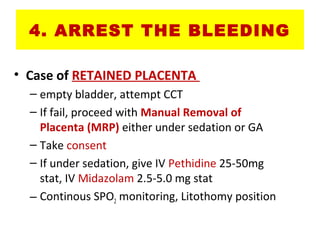
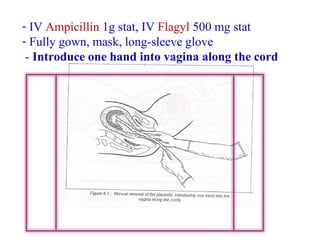
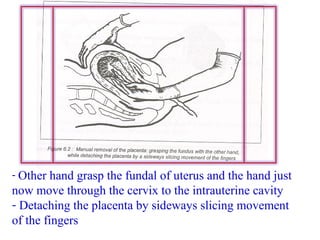
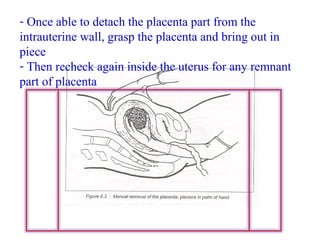
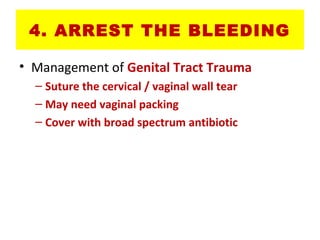
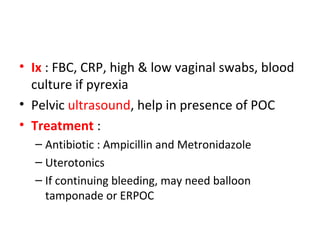
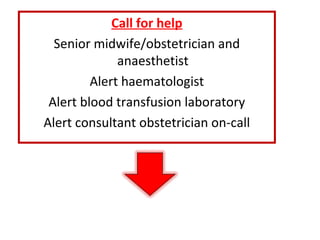
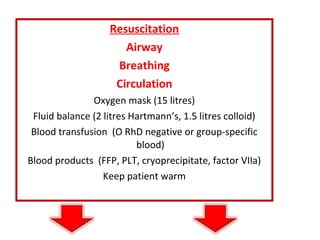
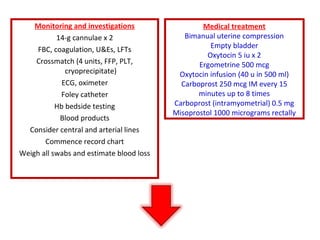
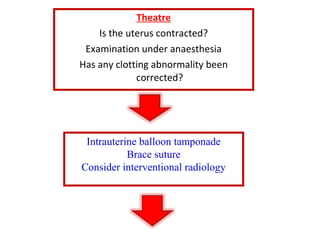
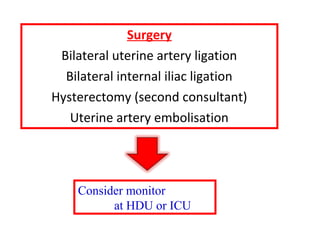
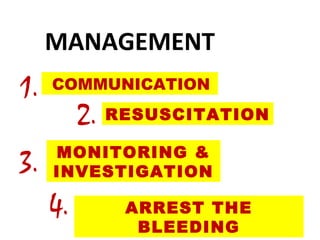
3. Management involves communication, resuscitation, monitoring, arresting the bleeding. Resuscitation focuses on airway, breathing, circulation, transfusions and fluid resuscitation. Arresting bleeding uses uterotonics, tamponade, compression sutures,
![2.
RESUSCITATION
• A B C
• The measurement for resuscitation depend
on condition and degree of shock
• Assess Airway and Breathing
– Give oxygen 10-15 L/min via face mask
regardless the maternal [O2]
– If airway is compromised due to impaired
conscious level, need to intubate with
anaesthetic assistance](https://image.slidesharecdn.com/pph-130718103052-phpapp02/85/Post-partum-Haemorrhage-29-320.jpg)