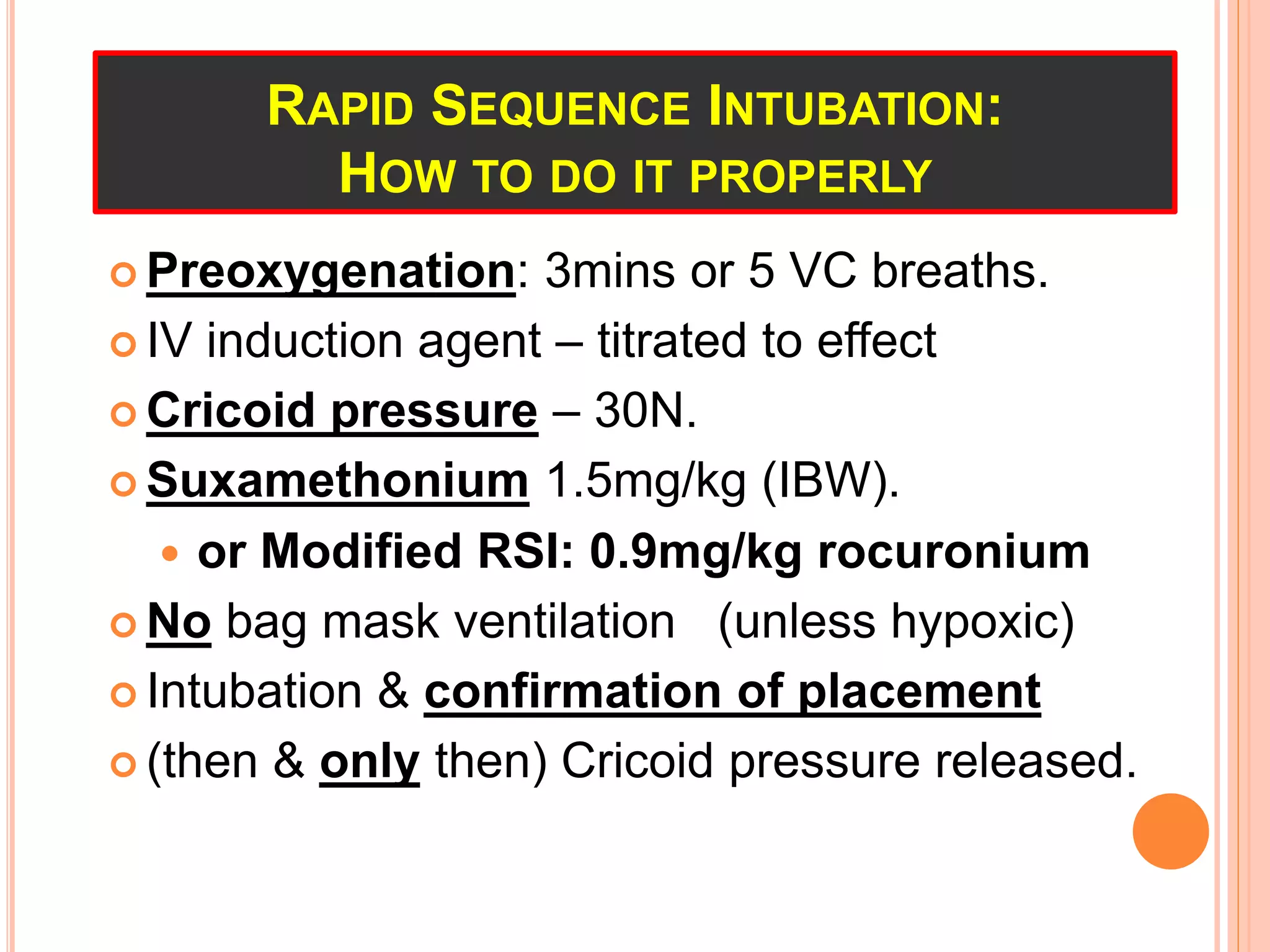
This document serves as a study guide for the anaesthetics involved in gynaecological laparoscopic procedures, highlighting a case of a 25-year-old woman with polycystic ovaries undergoing a laparoscopic cystotomy. It discusses anaesthetic management, equipment, and airway control methods, emphasizing the risks and protocols for maintaining patient safety during anaesthesia, particularly in ensuring adequate ventilation and analgesia. Various airway management techniques and anaesthetic circuits are also detailed, stressing the importance of preparedness for potential complications.
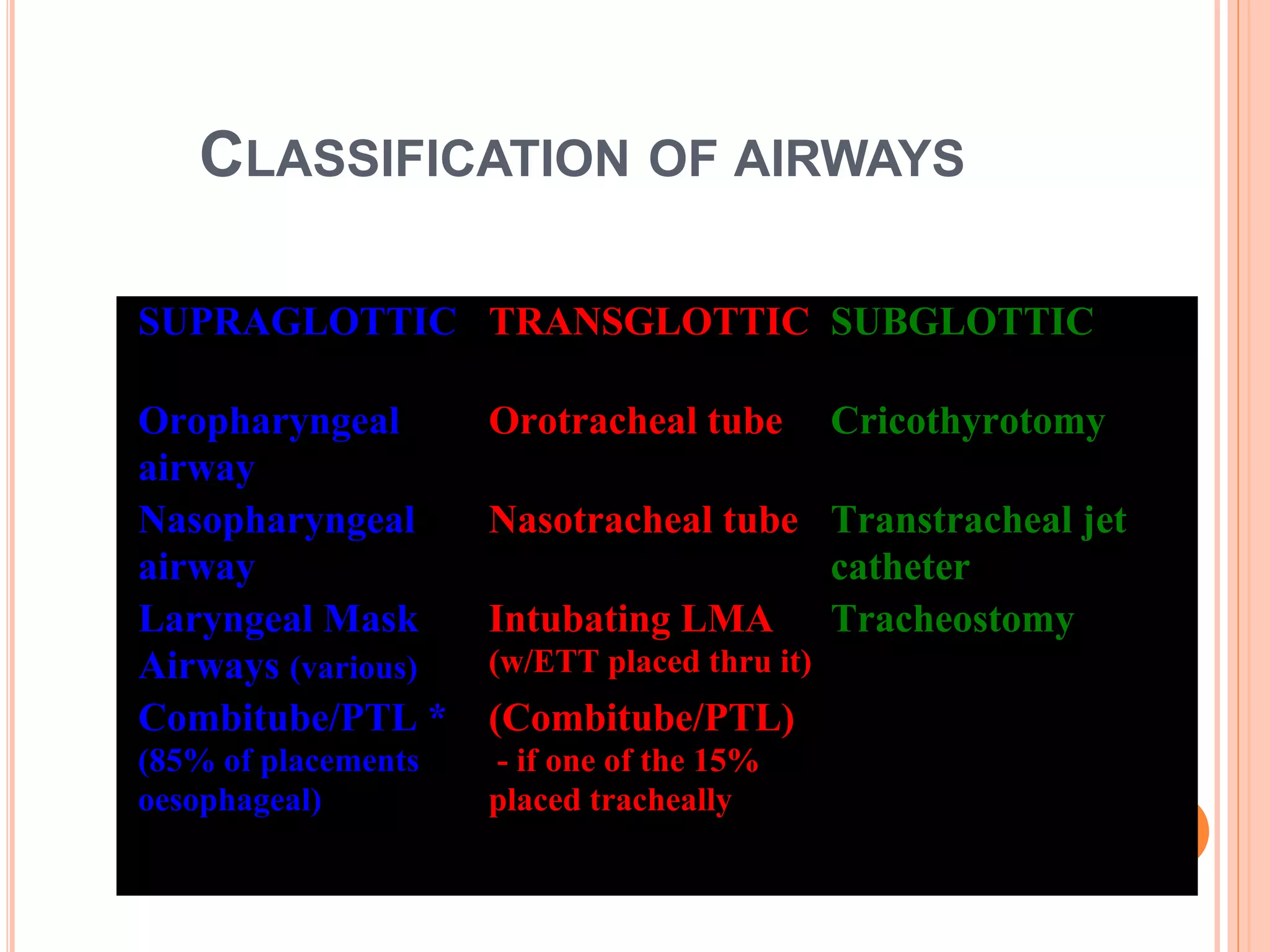
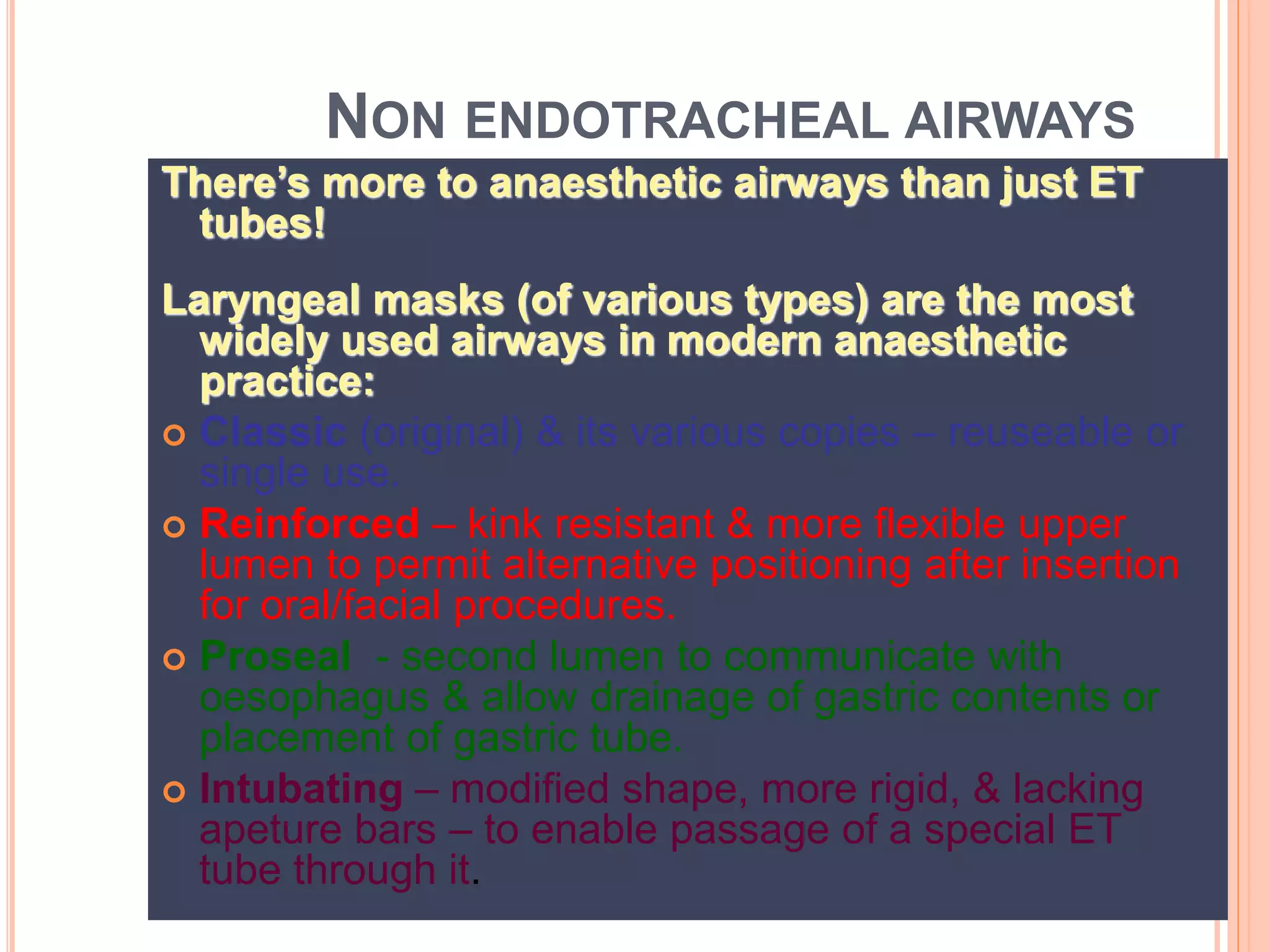
![EMERGENCY AIRWAY MANAGEMENT
(IN ANAESTHESIA & RESUSCITATION)
Rapid sequence
intubation
[or unmodified
(“cold”) intubation if
apnoeic & arreflexic]
Other
techniques:
Fibreoptic intubation
Supraglottic airway
Surgical airway
>90% <10%](https://image.slidesharecdn.com/drrowanmolnaranaestheticsstudyguidepartiii-151028063723-lva1-app6891/75/Dr-rowan-molnar-anaesthetics-study-guide-part-iii-20-2048.jpg)
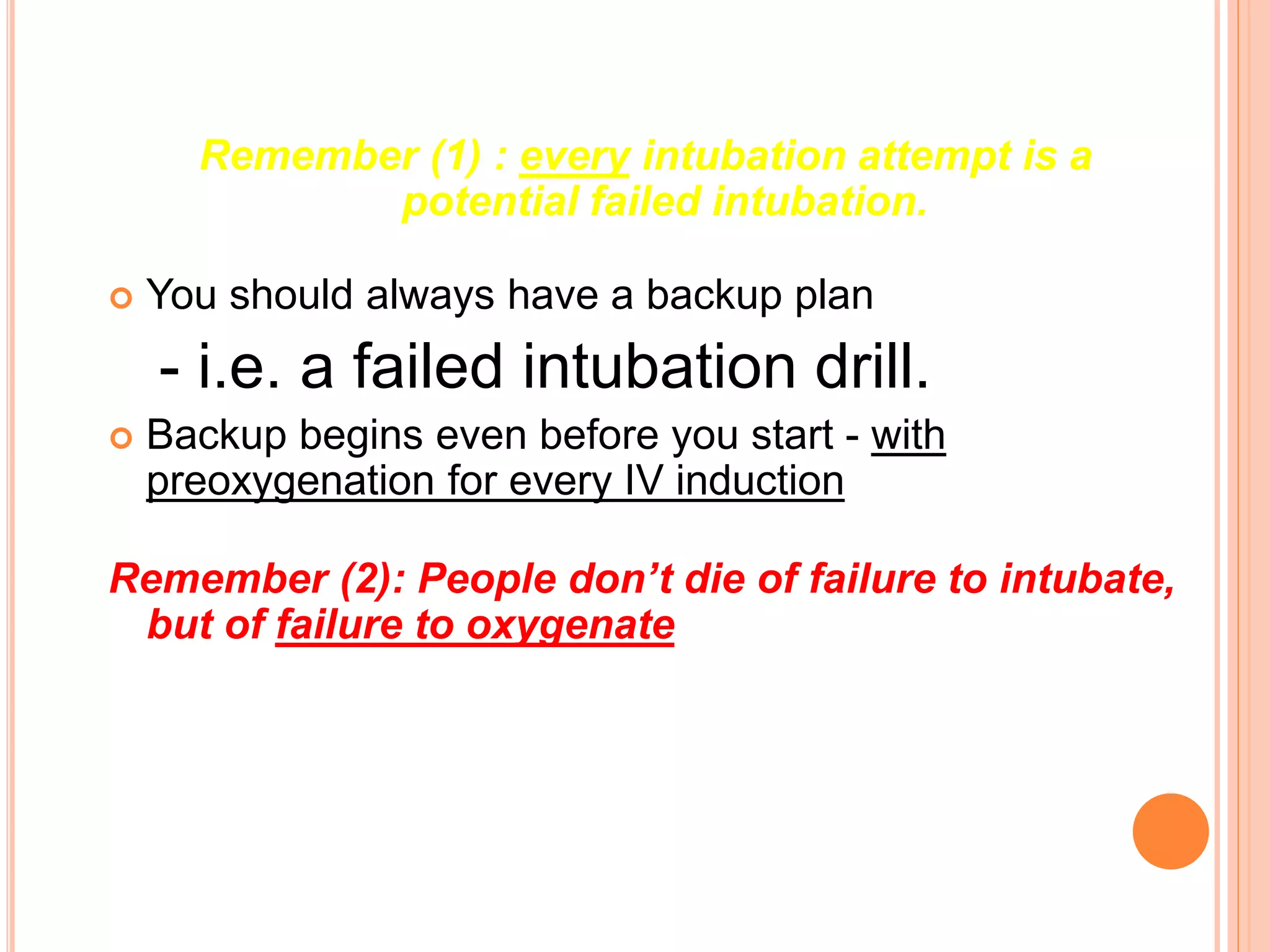
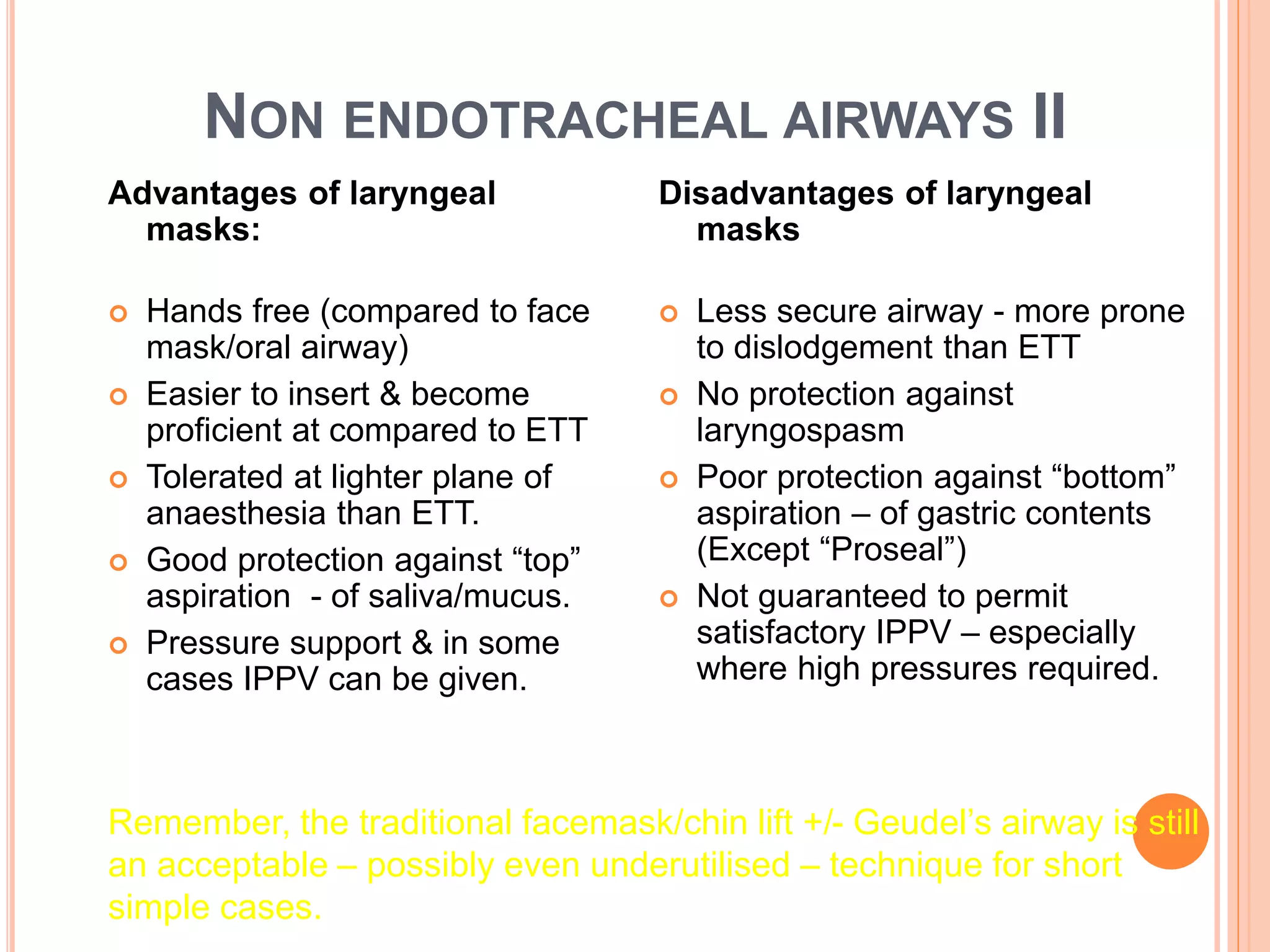
![Supraglottic rescue airway
e.g. LMA
SUCCESSFUL?
Subglottic (surgical) airway
1. Bag mask ventilation
2. Repeat attempt &/or
alternate technique to
intubate
SUCCESSFUL?
FIRSTLY MAINTAIN
OXYGENATION!
FAILED INTUBATION DRILL
CAN YOU MASK VENTILATE? [With
Geudels &/or nasopharyngeal airway if
necessary]
NO
NO
YES
NO](https://image.slidesharecdn.com/drrowanmolnaranaestheticsstudyguidepartiii-151028063723-lva1-app6891/75/Dr-rowan-molnar-anaesthetics-study-guide-part-iii-23-2048.jpg)