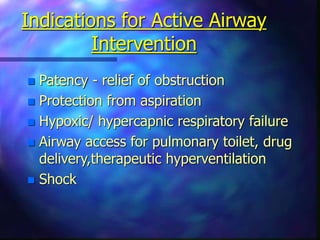
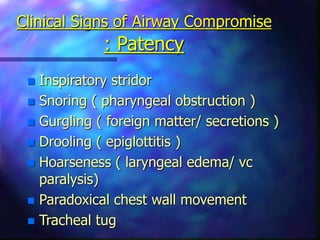
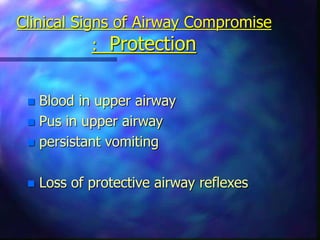
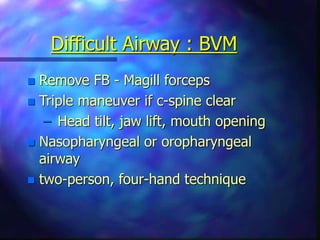
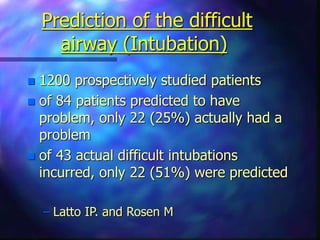
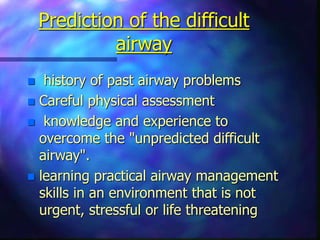
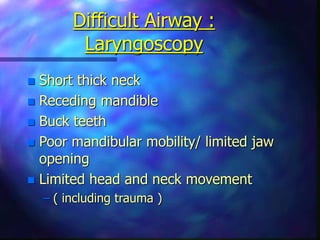
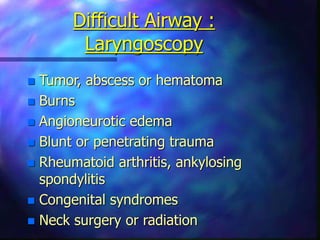
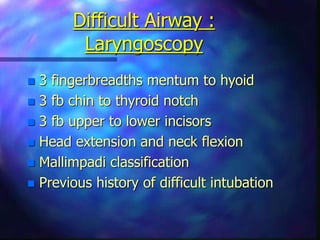
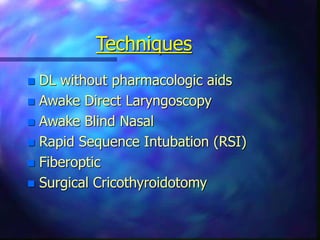
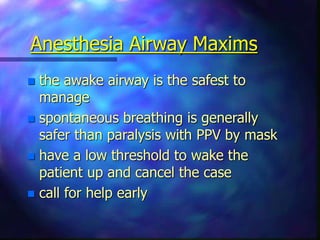
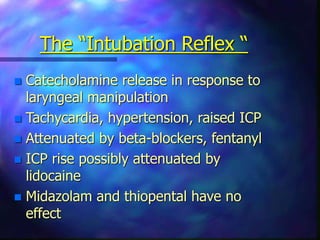
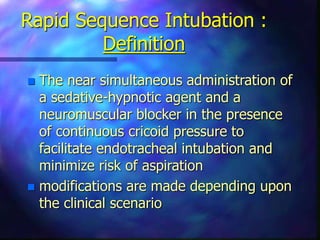
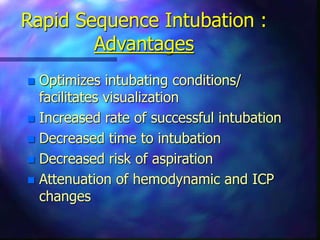
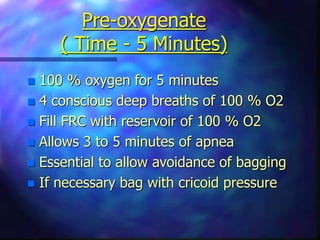
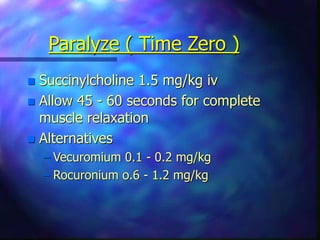
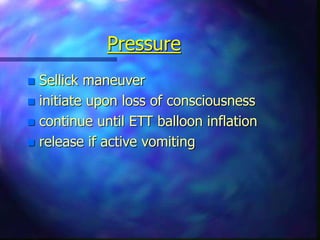
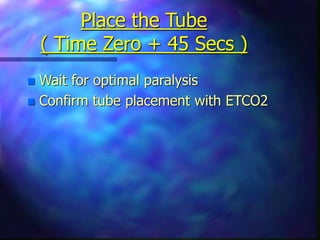
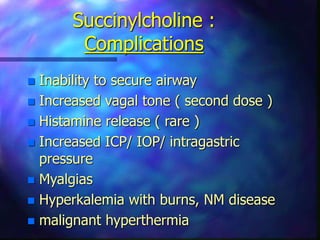
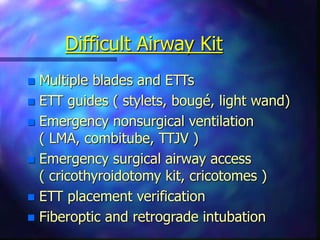
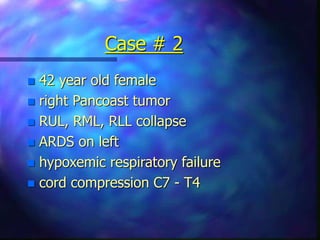
This document discusses emergency airway management. It outlines the importance of assessing the airway and developing a primary plan and backup plan. It describes signs of airway compromise related to patency, protection, and oxygenation/ventilation. Techniques for managing difficult airways include bag-valve-mask ventilation, endotracheal intubation, and alternate methods. Rapid sequence intubation involves preoxygenating, preparing, premedicating, paralyzing, applying cricoid pressure, and intubating the patient. Surgical airways are a last resort but are preferable to an unventilated patient.