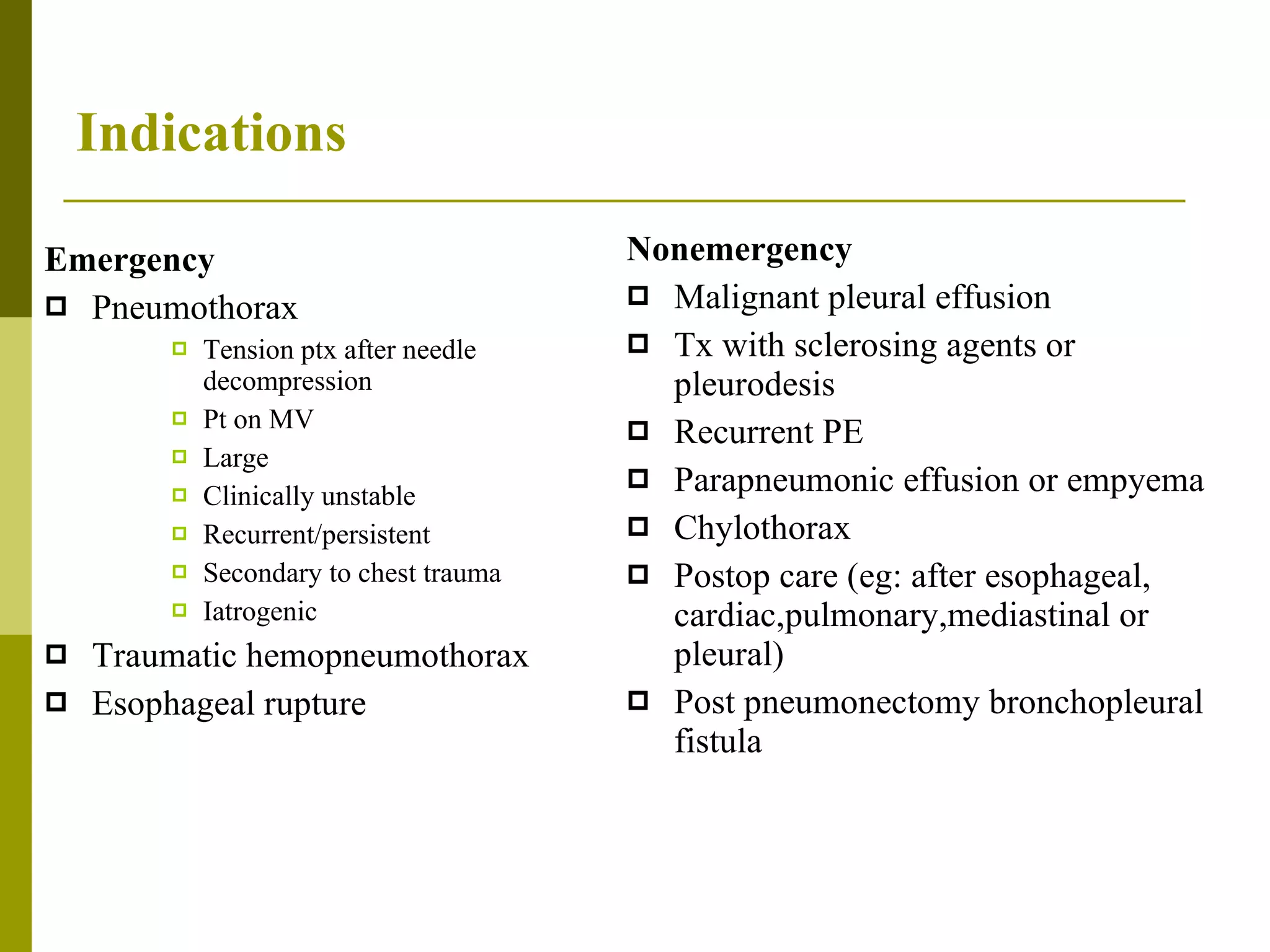
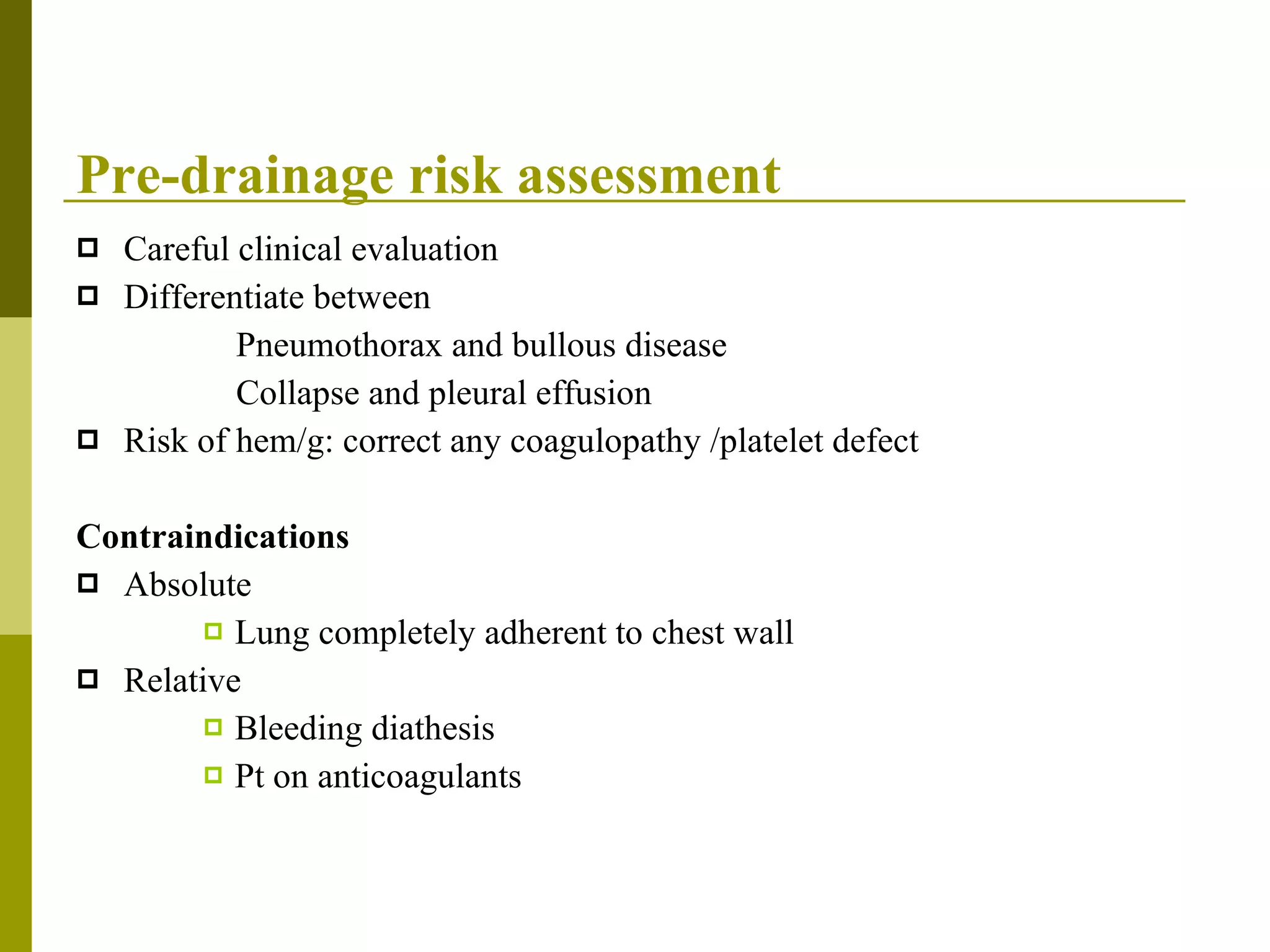
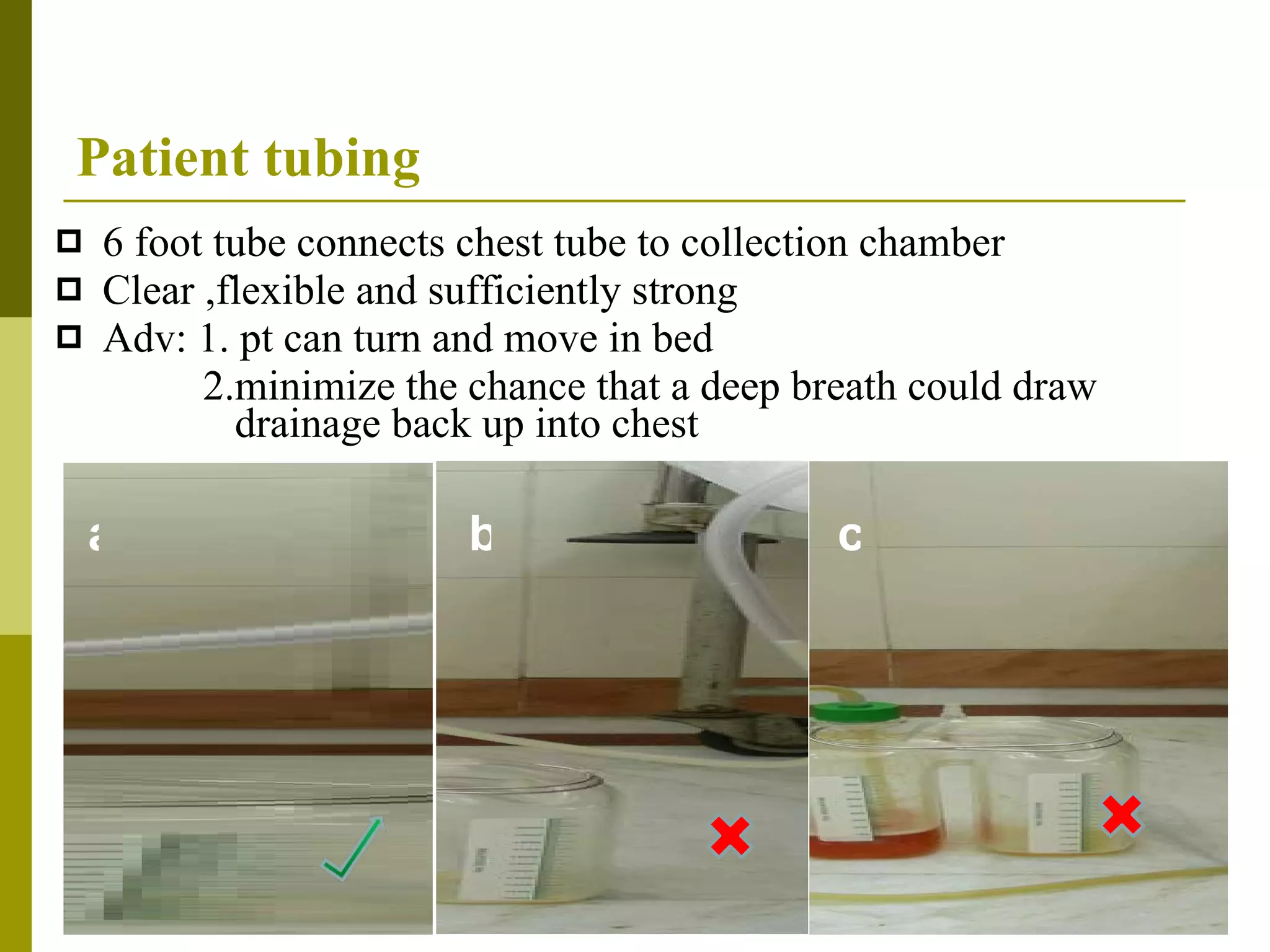
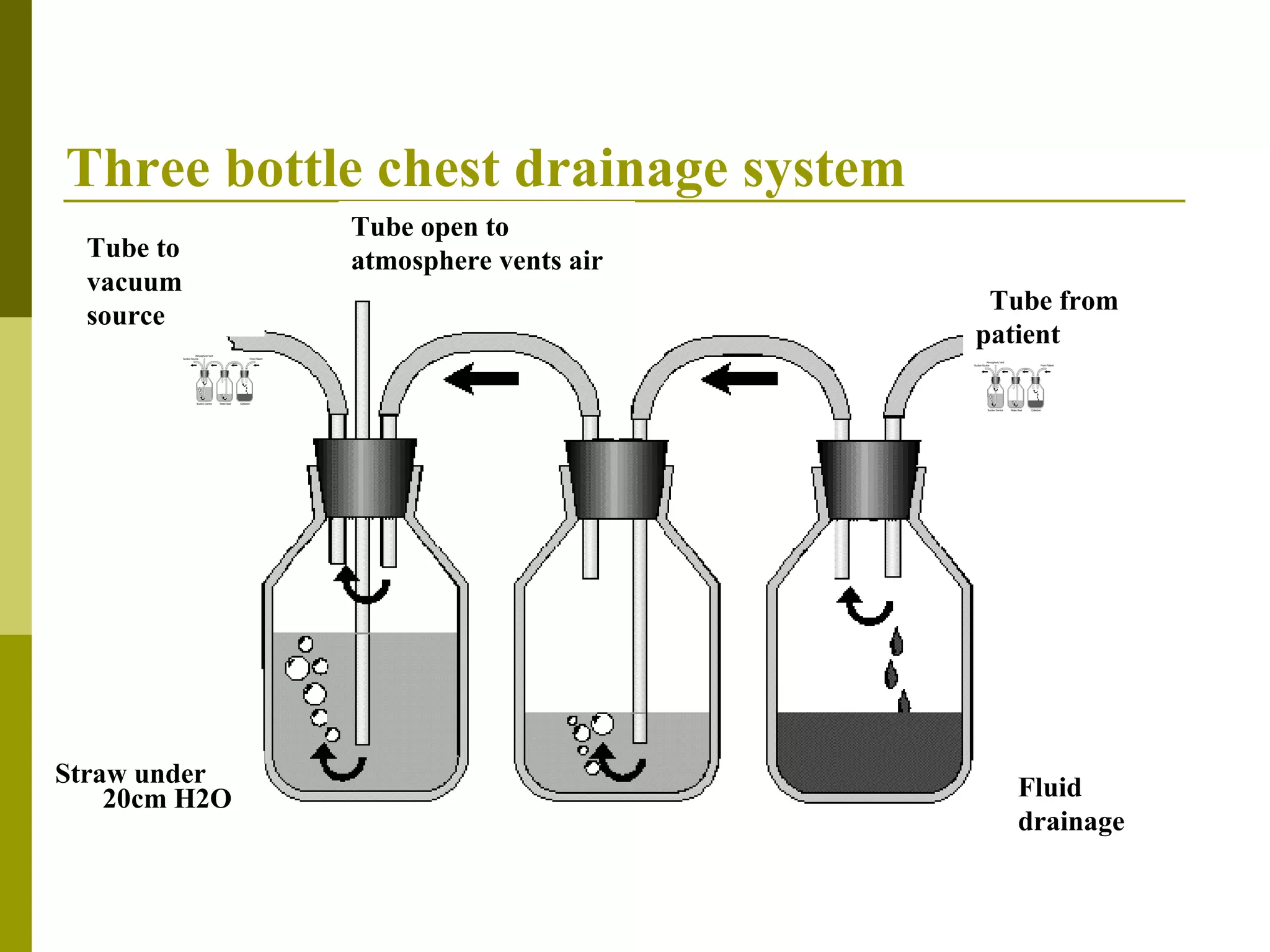
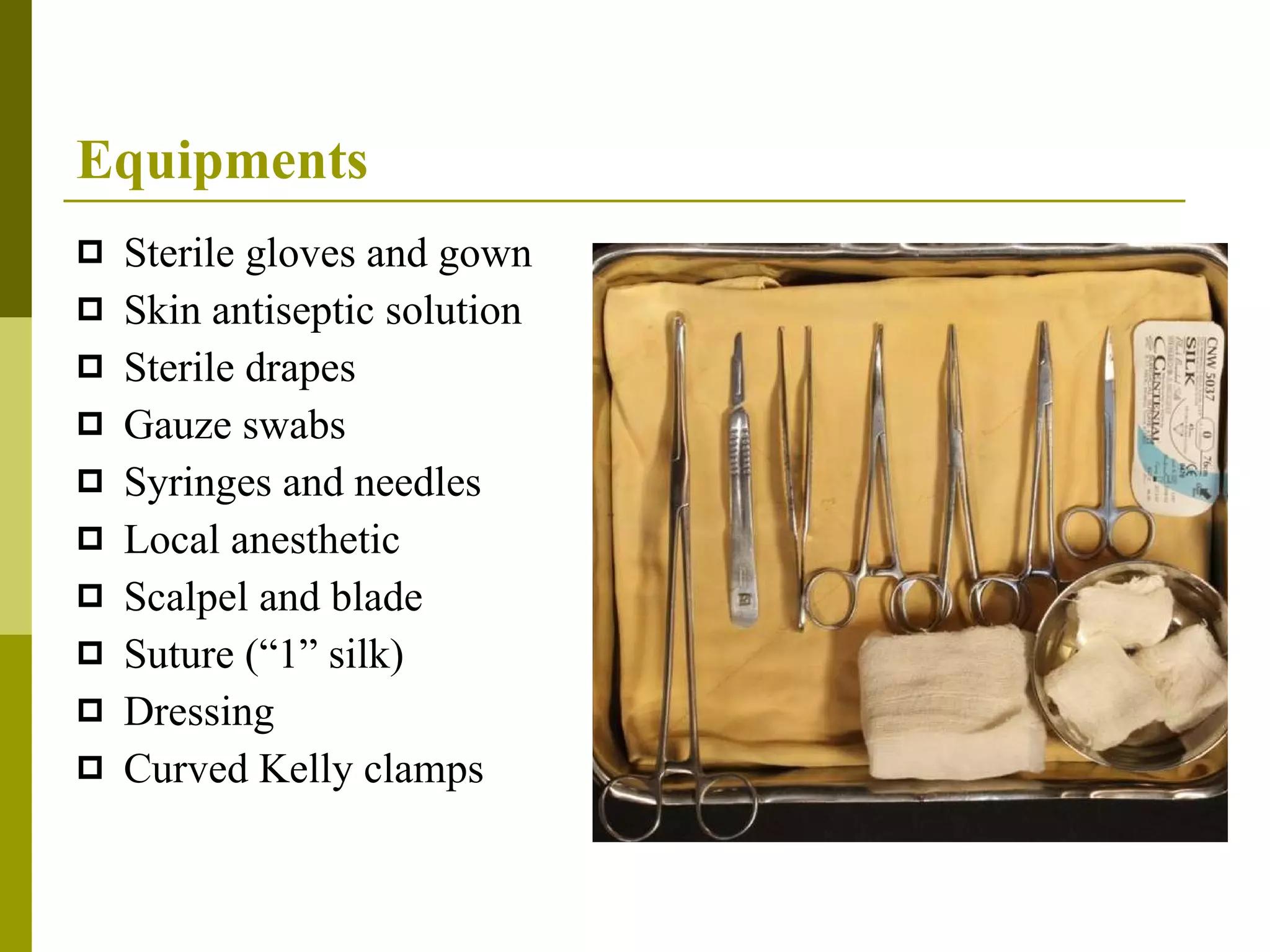
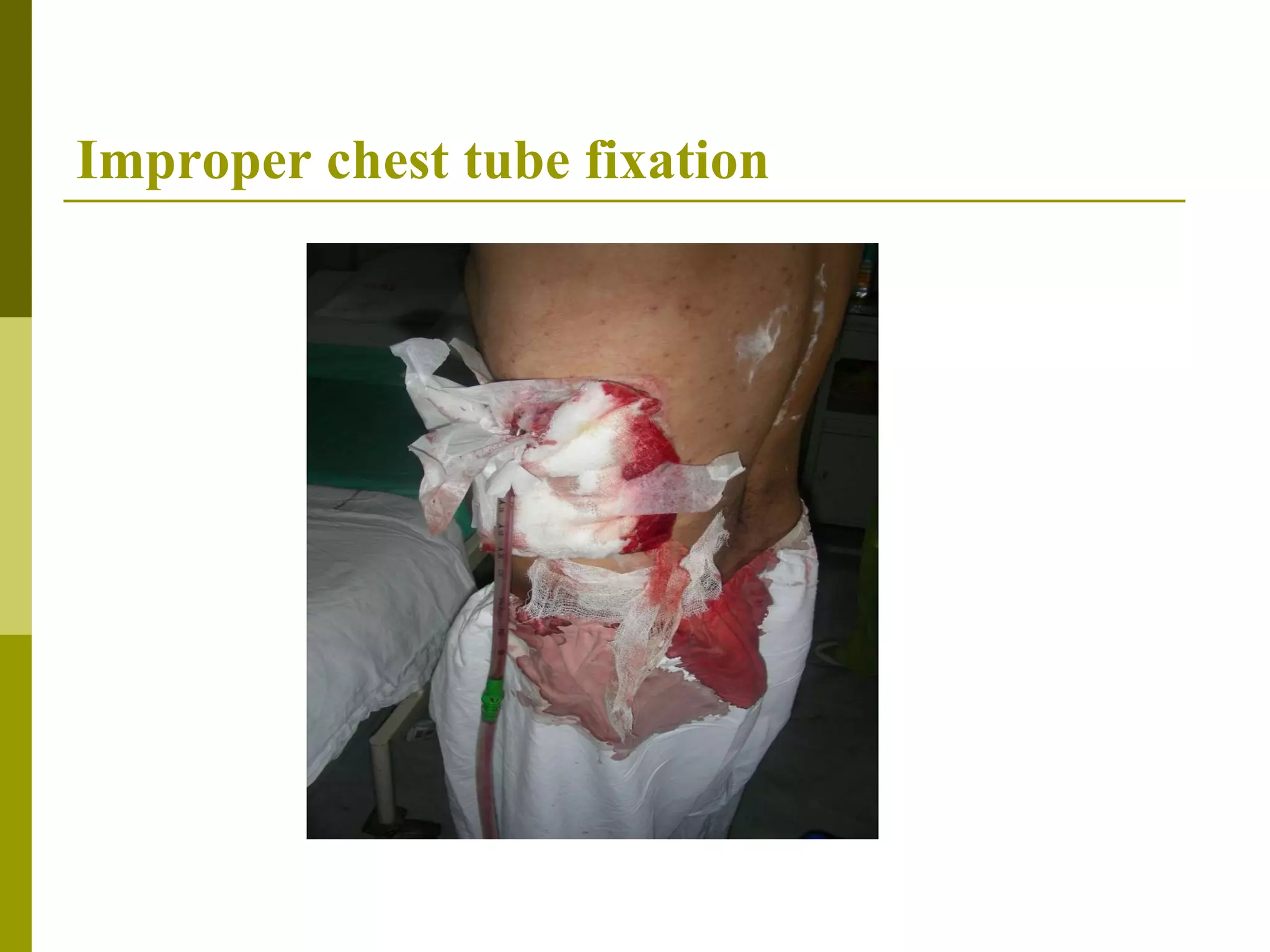
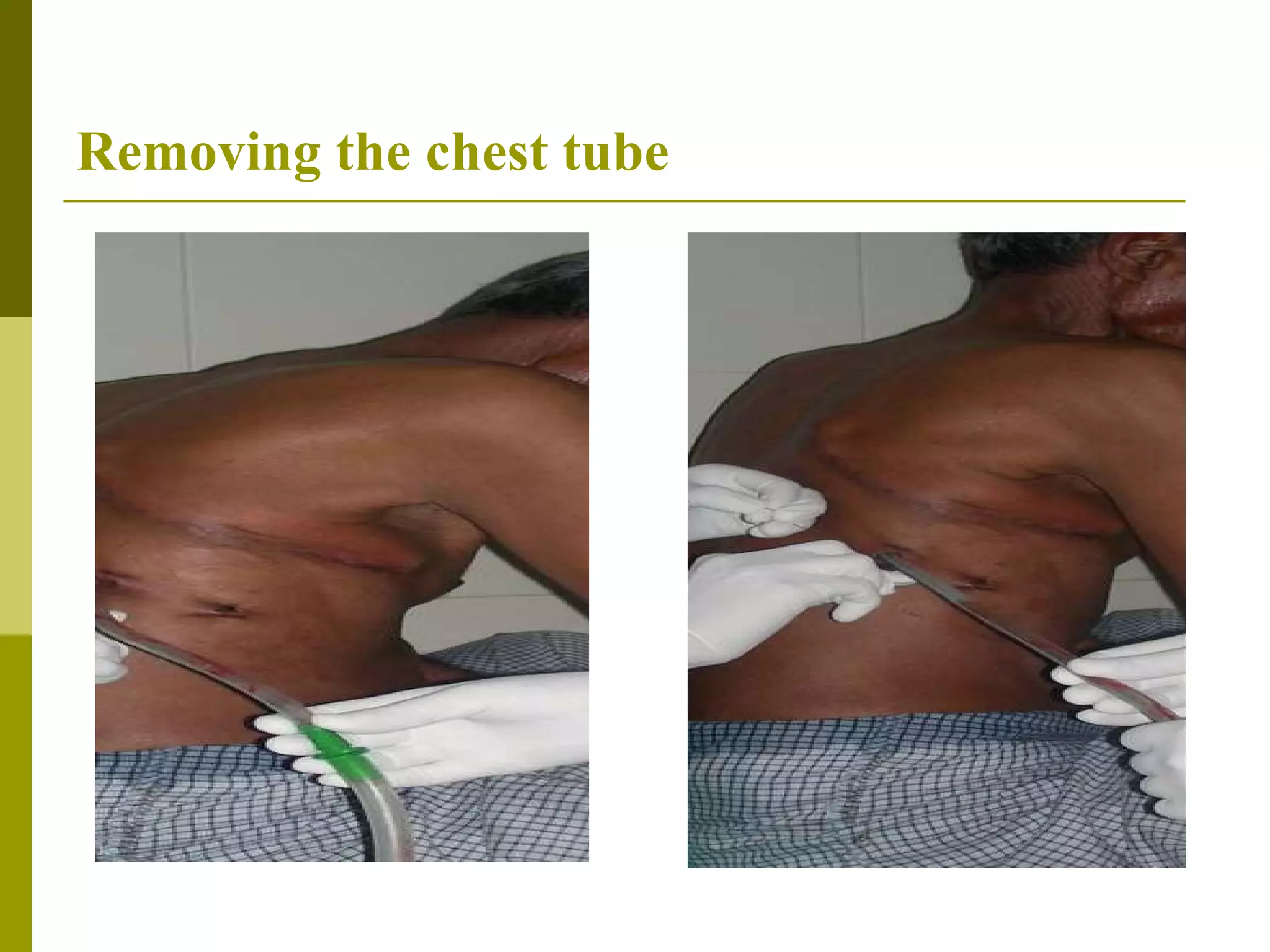
Chest drains are used to drain fluid, air or blood from the pleural space between the lungs and chest wall. Indications include pneumothorax, pleural effusions, and trauma. Proper placement requires sterile technique and imaging guidance. Chest drainage systems use water seals and suction to remove fluid while preventing re-entry of air into the chest. Patient care involves monitoring drainage, lung re-expansion and preventing complications like infection. Tubes are typically removed once drainage decreases and lungs are fully re-expanded.