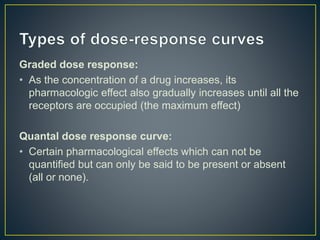
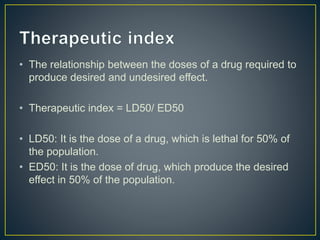
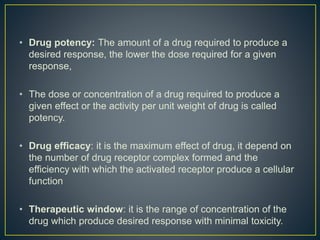
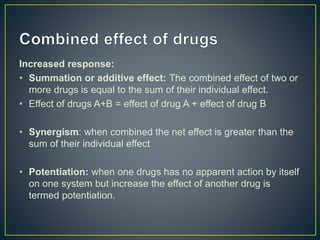
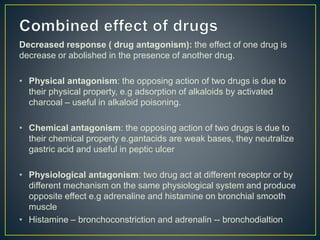
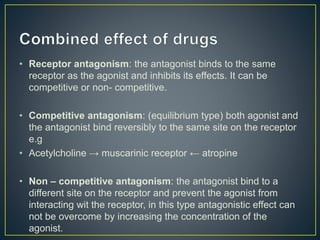
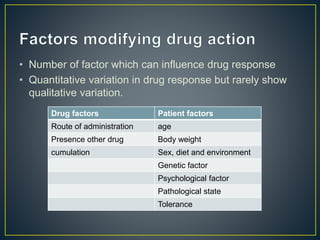
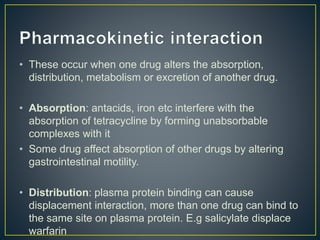
The document discusses various concepts related to pharmacology including dose-response relationships, drug potency and efficacy, therapeutic index, and factors that can influence drug response. It describes the graded and quantal types of dose-response curves and defines potency as the amount of drug required to produce a desired response. Therapeutic index is defined as the ratio of lethal to effective doses. The document also discusses how drug responses can be increased or decreased through summation, synergism, potentiation, and antagonism. Multiple factors are described that can affect drug response including route of administration, presence of other drugs, accumulation, and patient-related factors.