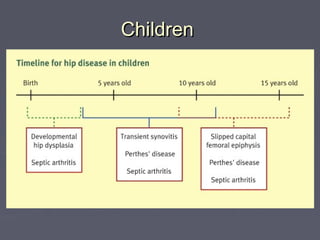
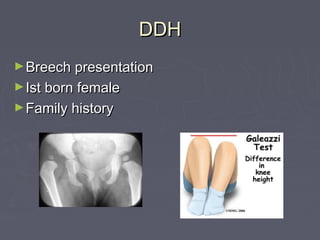
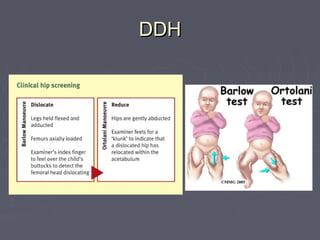
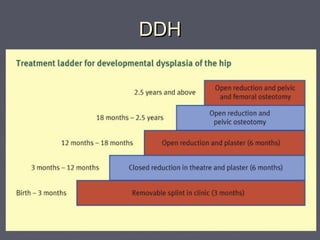
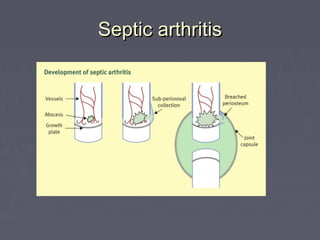
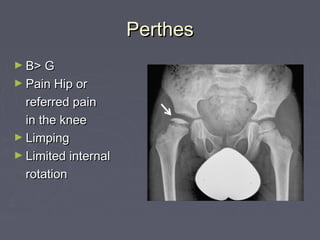
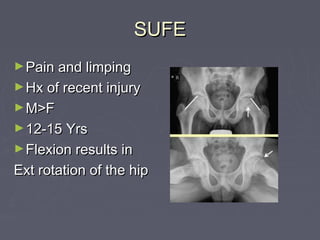
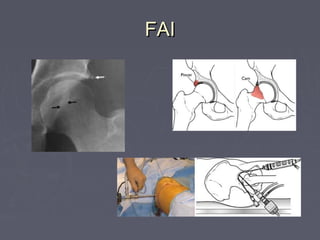
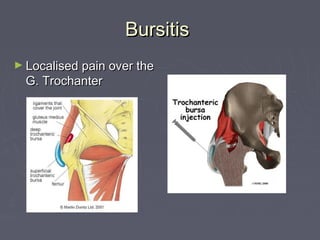
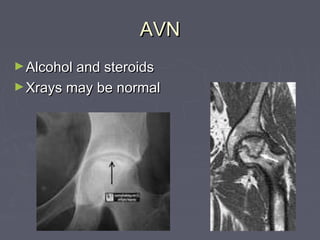
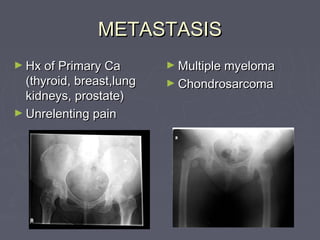
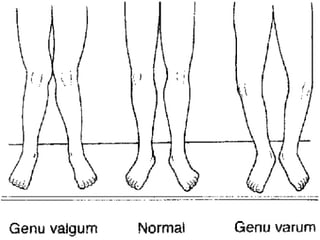
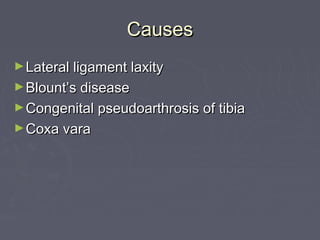
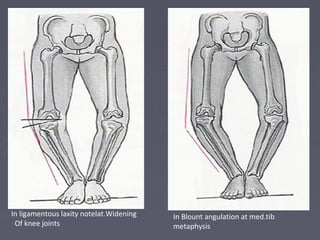
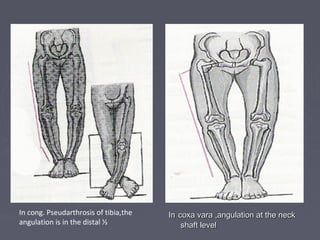
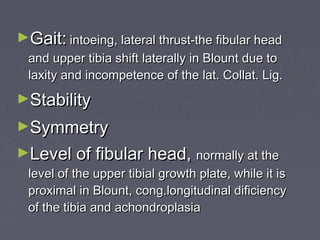
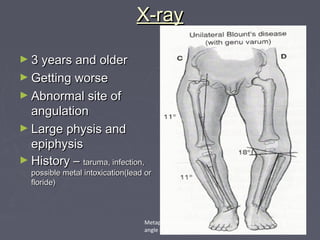
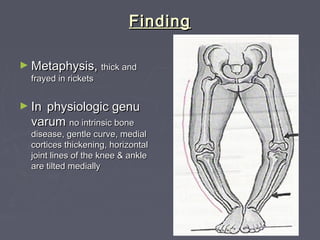
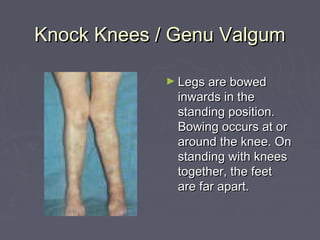
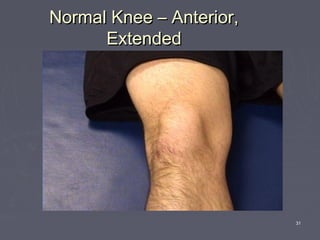
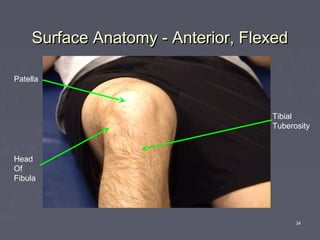
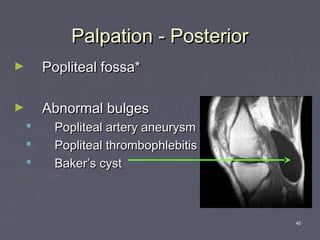
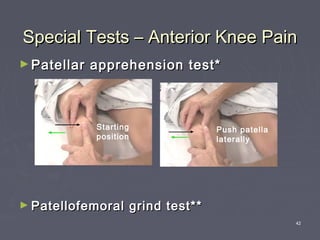
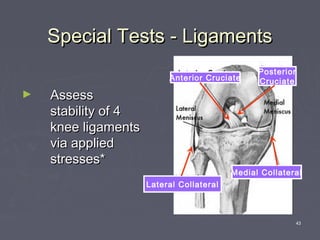
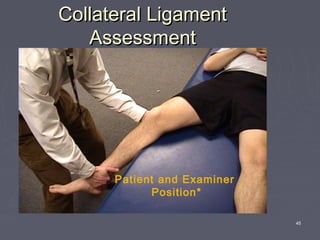
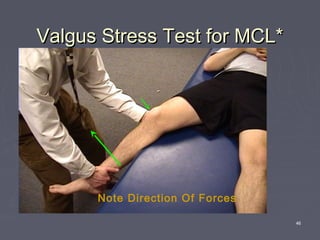
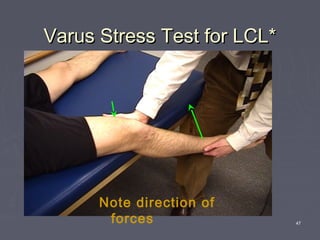
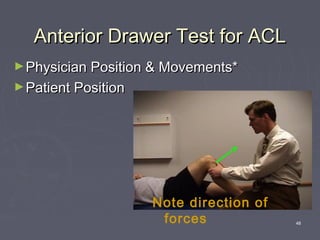
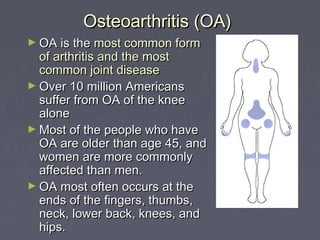
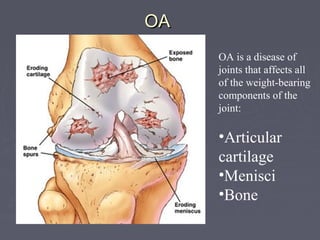
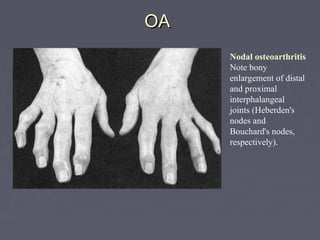
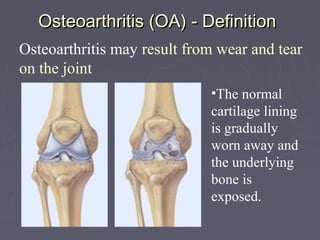
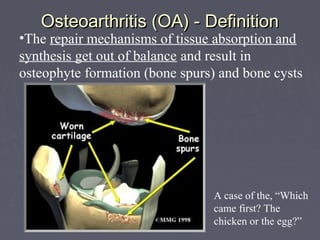
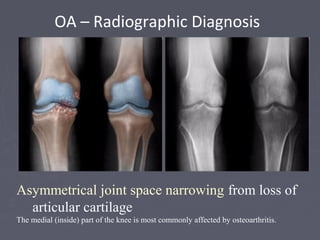
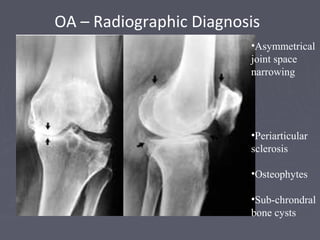
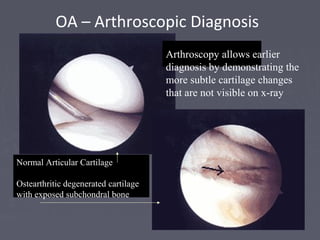
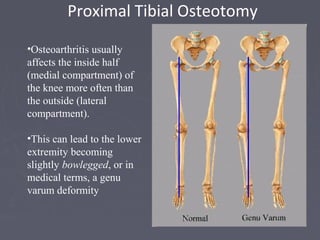
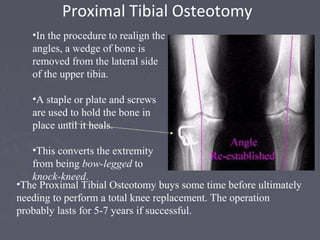
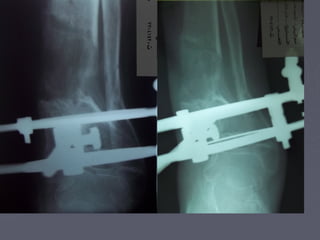
This document discusses disorders of the lower limbs, including causes such as congenital defects, inflammation, degeneration, trauma, and infection. It covers disorders grouped by age and then focuses on specific conditions of the hip and knee. For the hip, it describes diseases such as developmental dysplasia of the hip, Perthes disease, femoroacetabular impingement, bursitis, and osteoarthritis. For the knee, it discusses genu valgum/varum and performs assessments of range of motion, ligaments, and special tests for conditions like osteoarthritis.