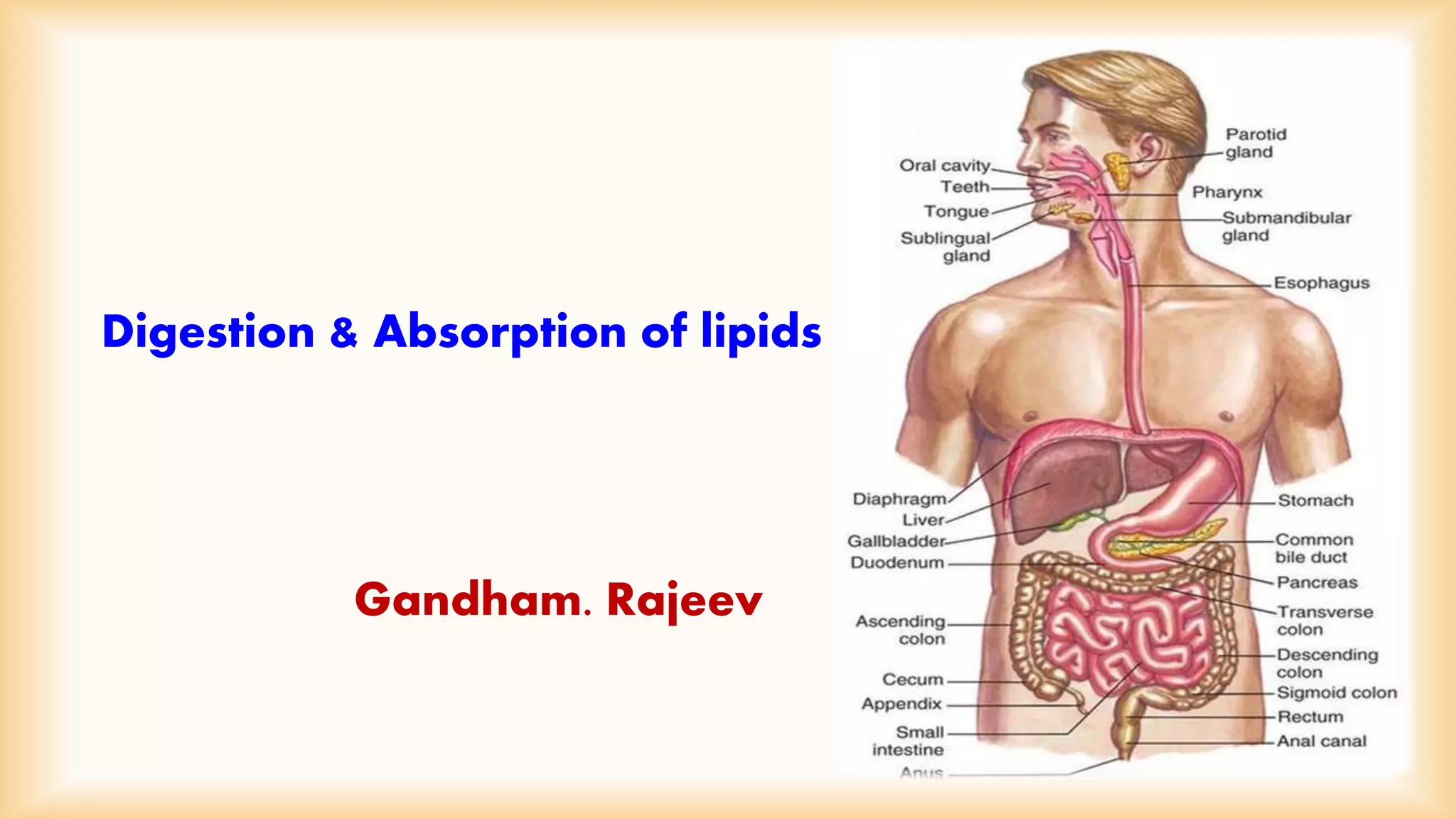
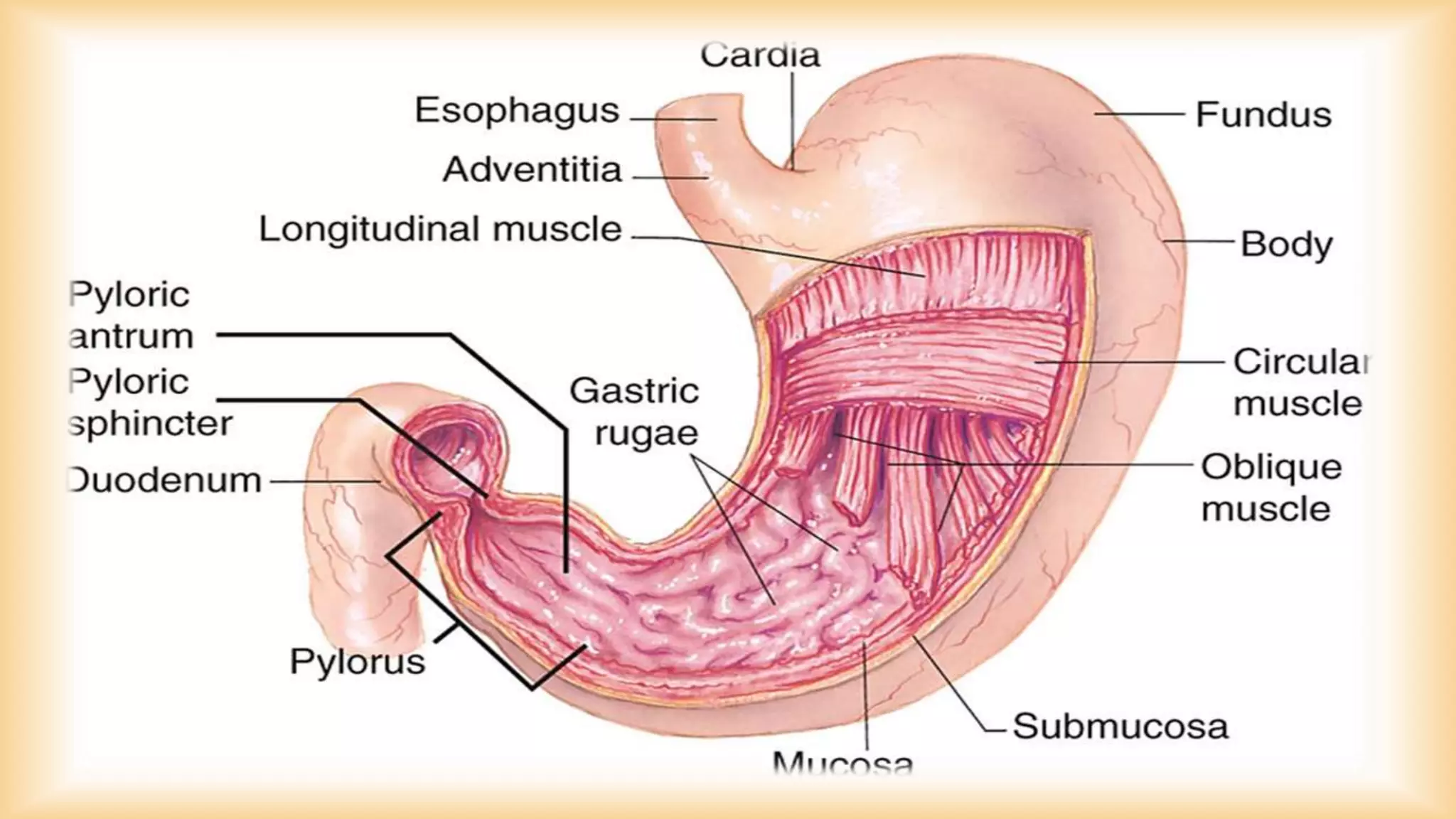
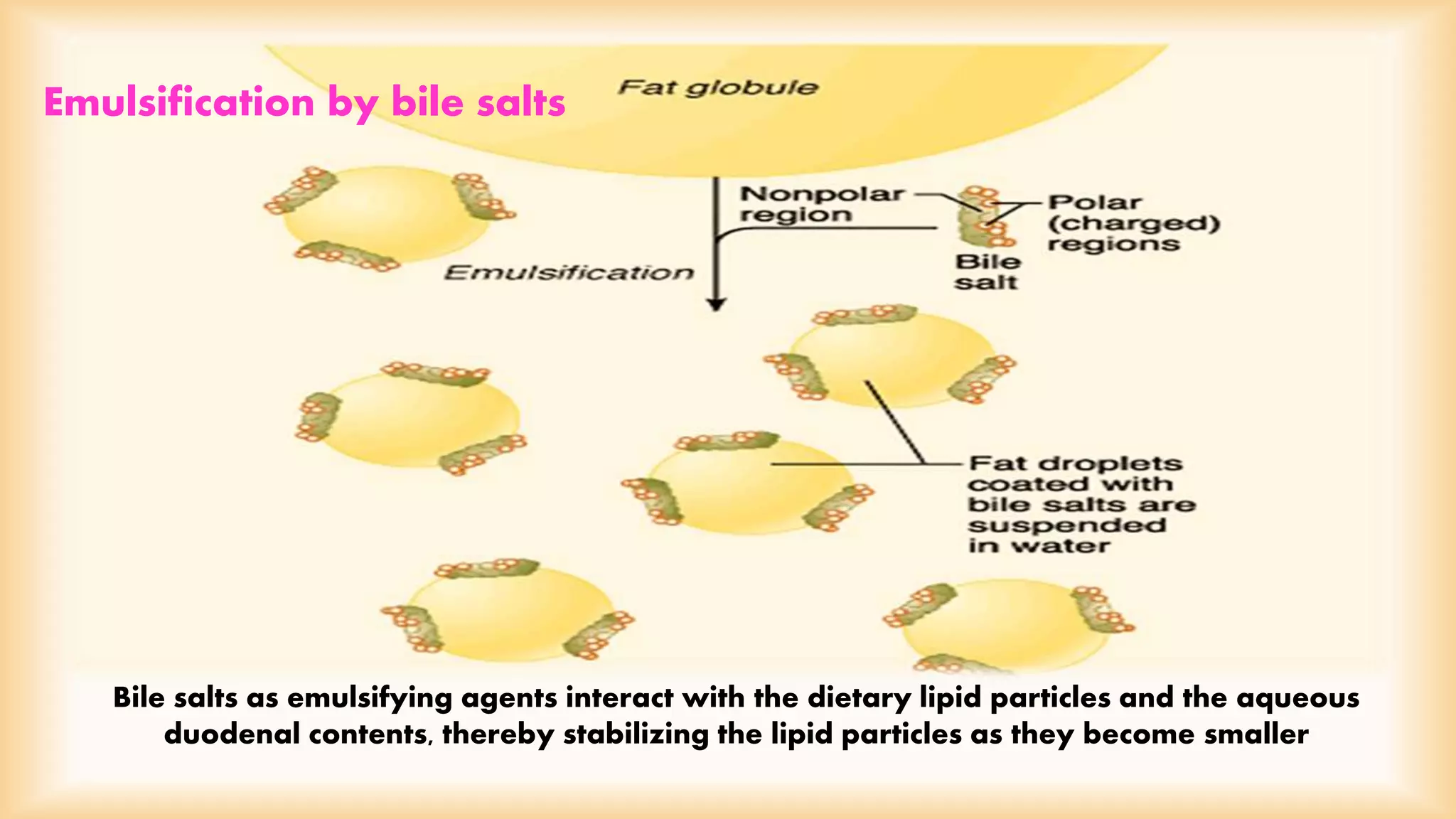
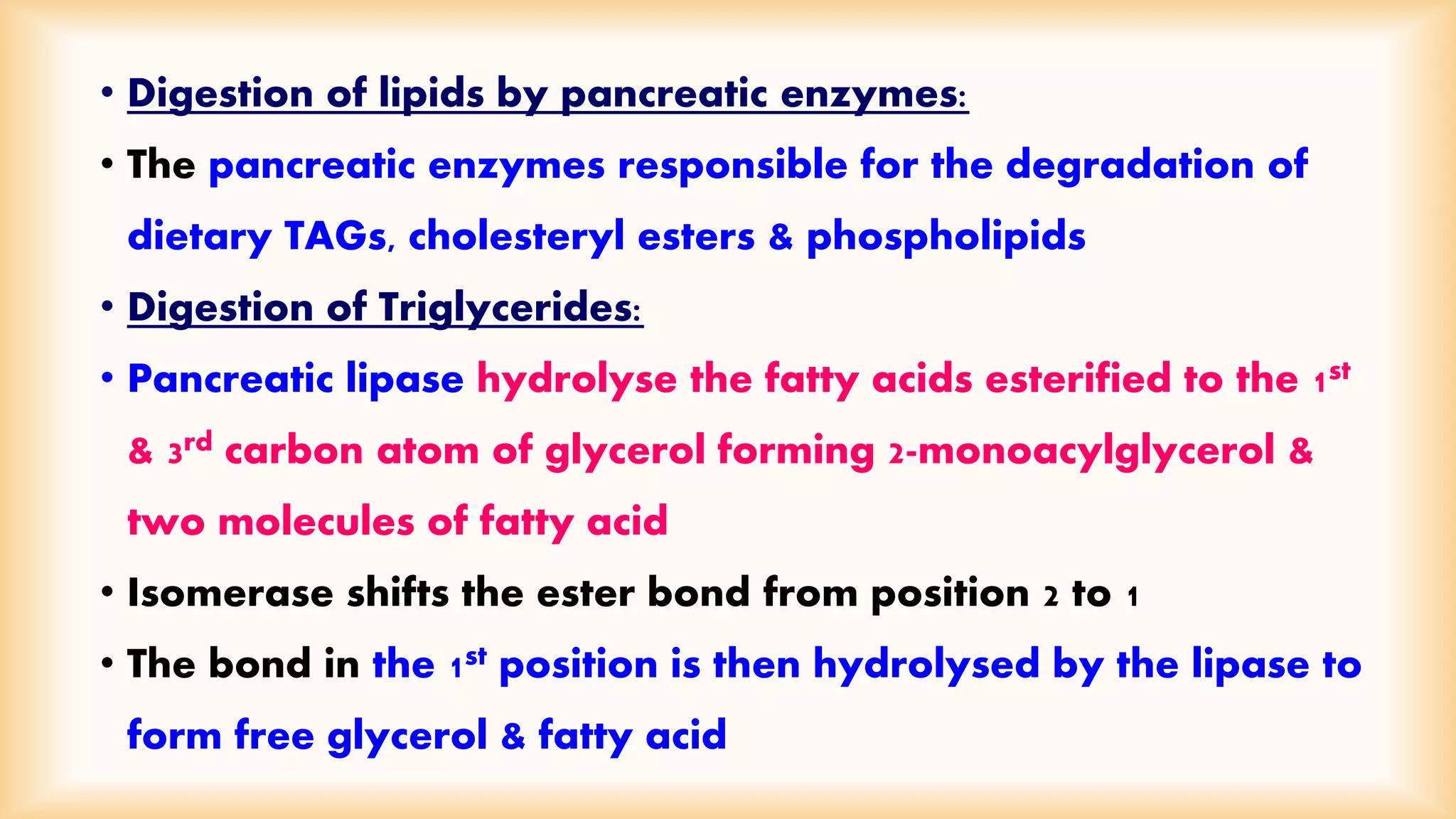
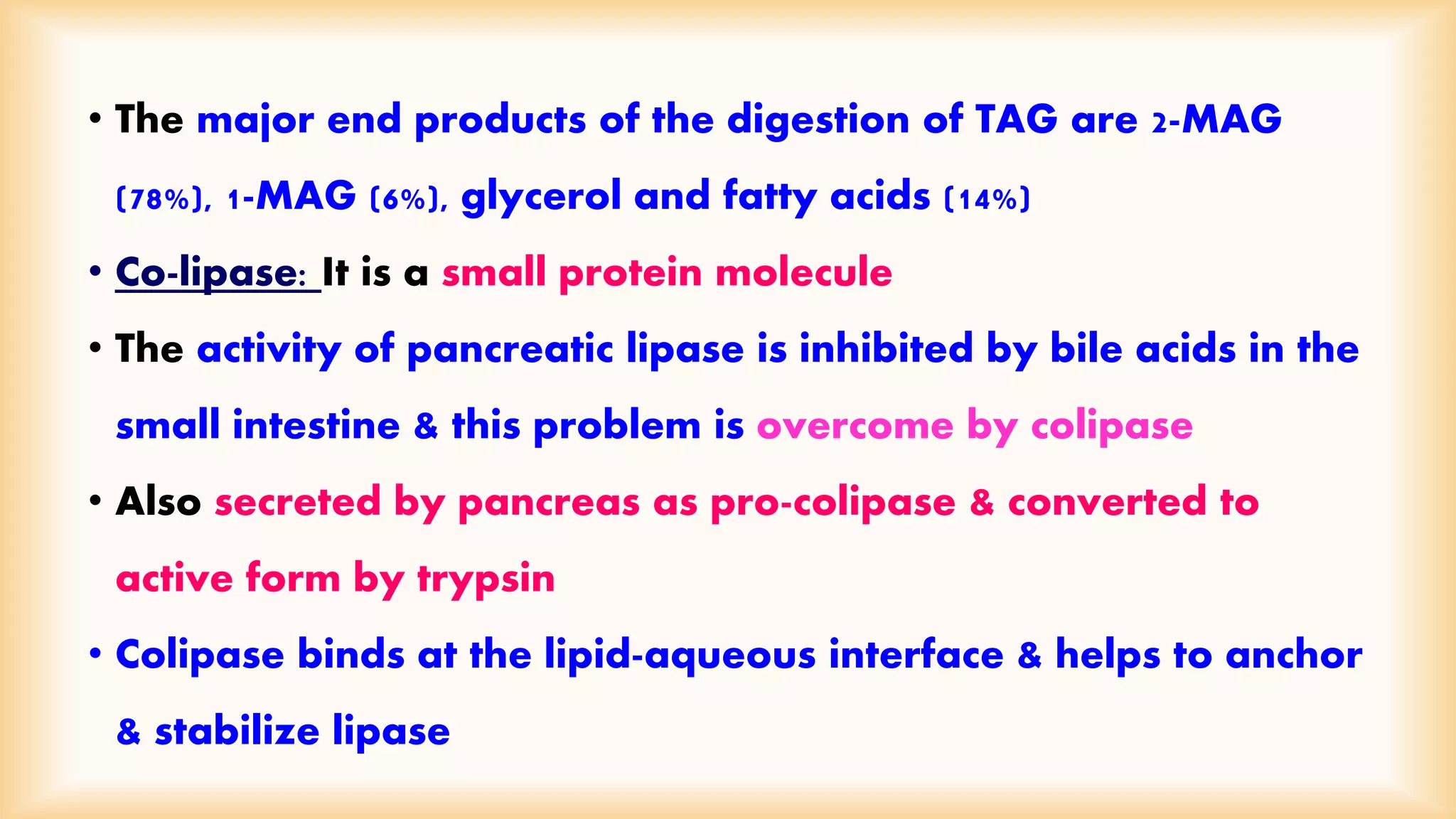
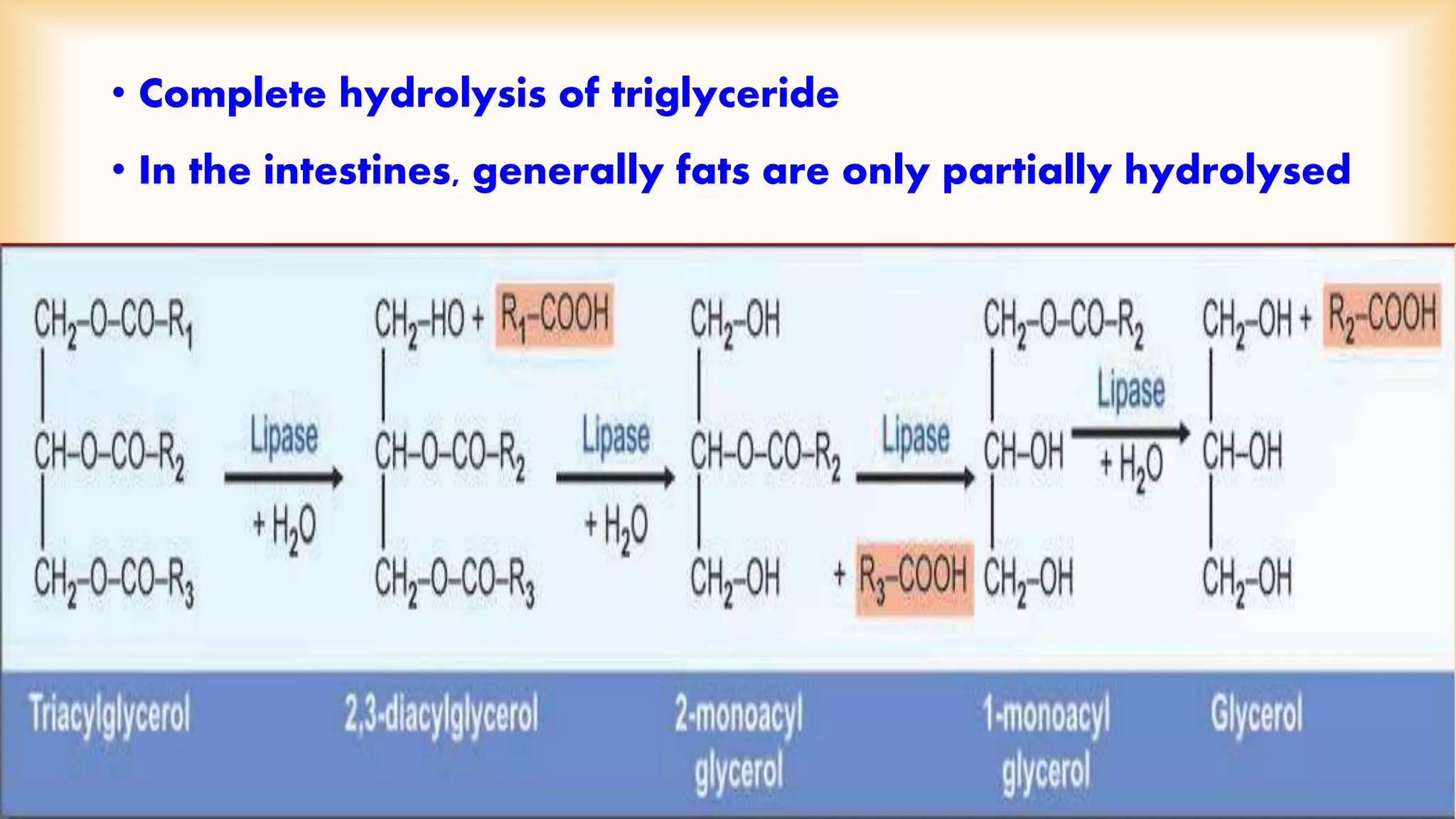
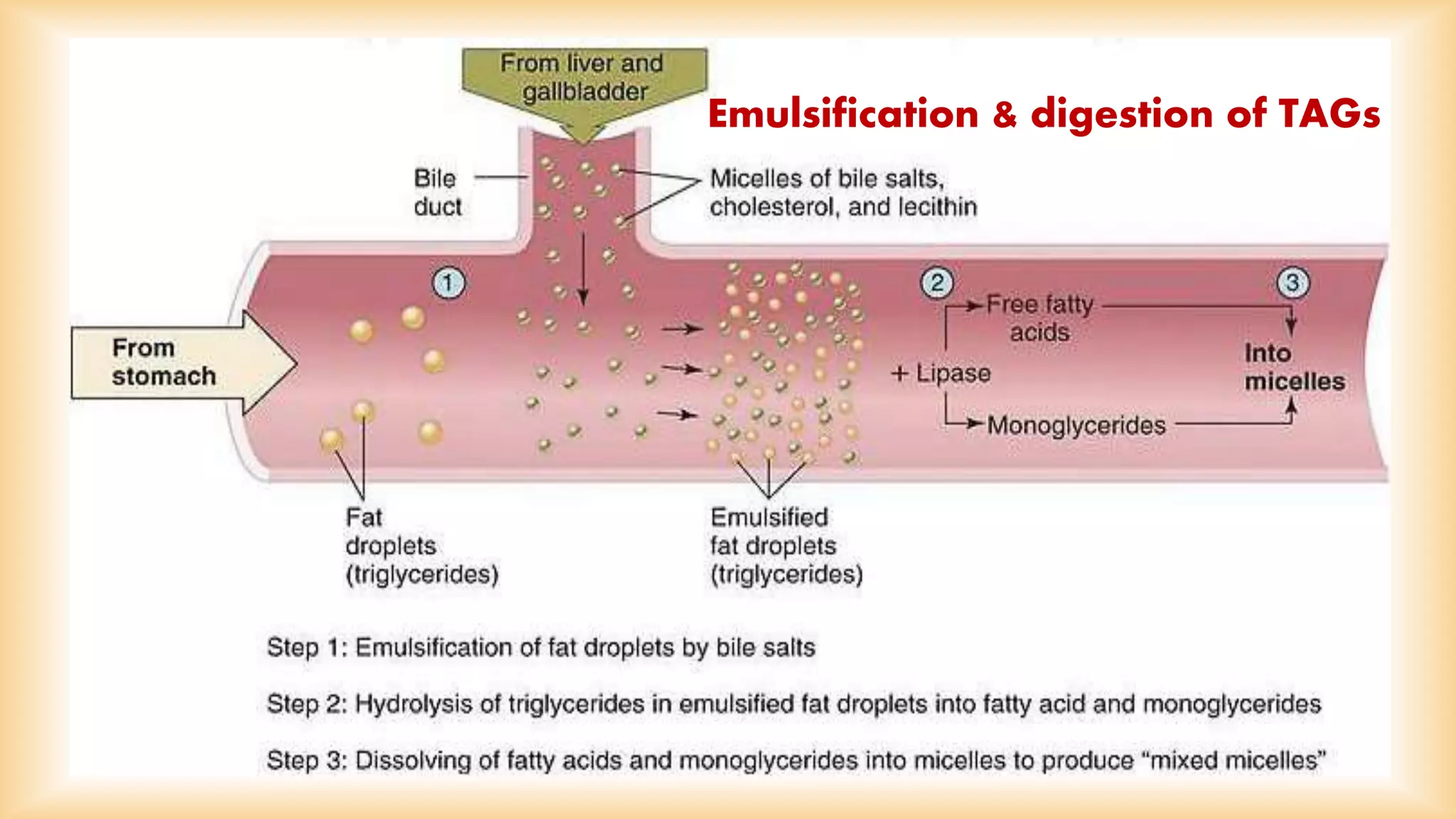
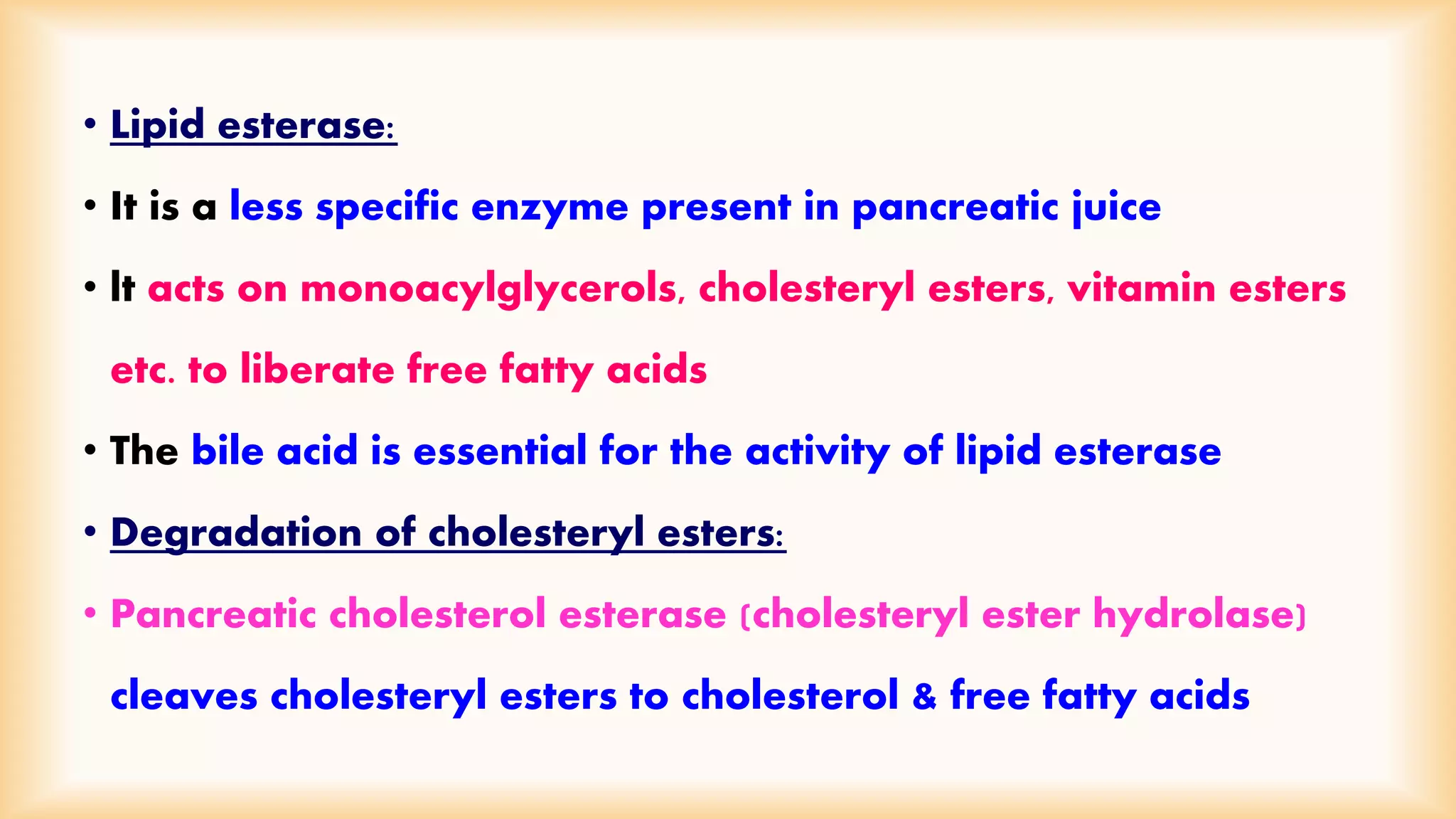
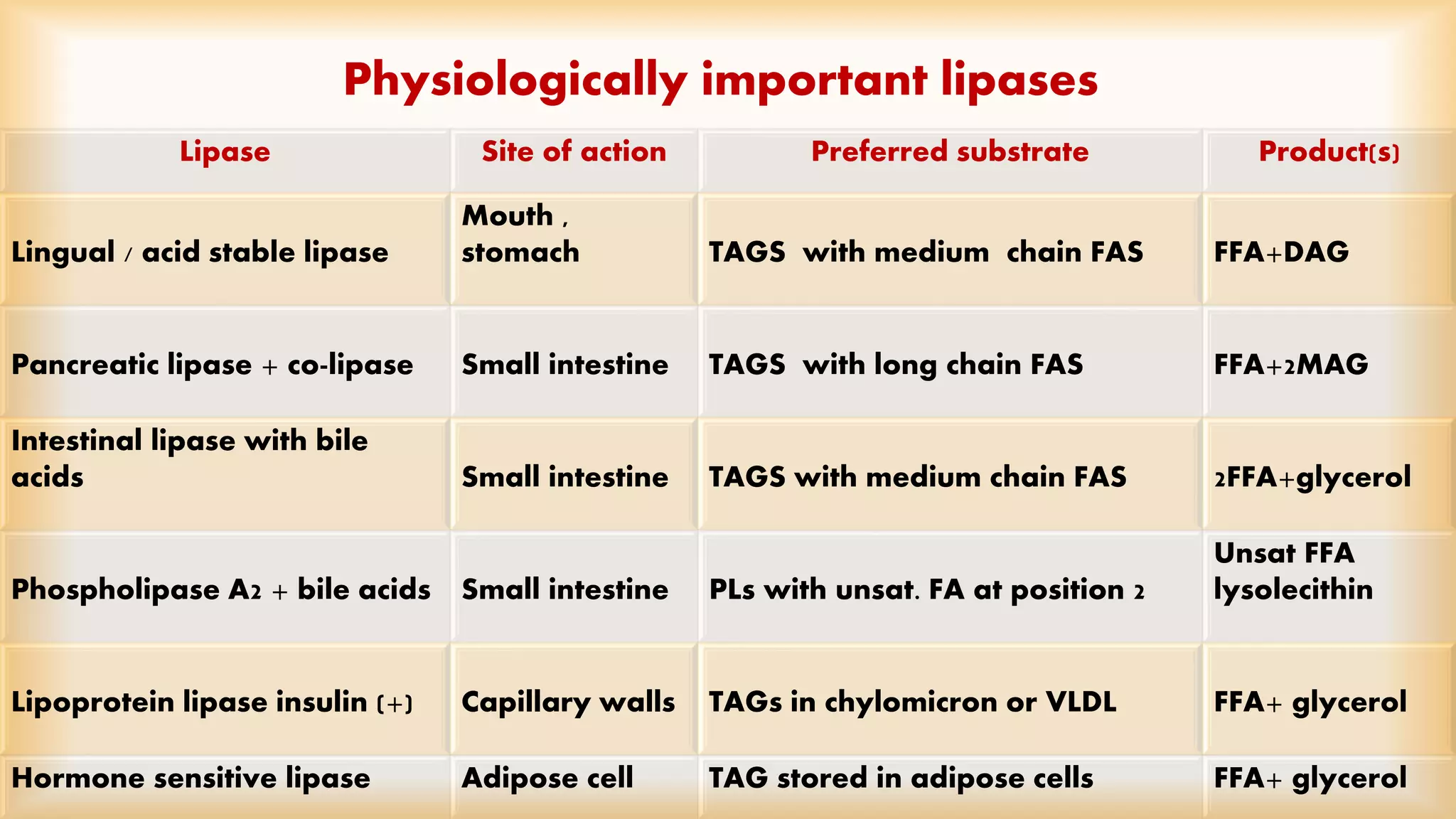
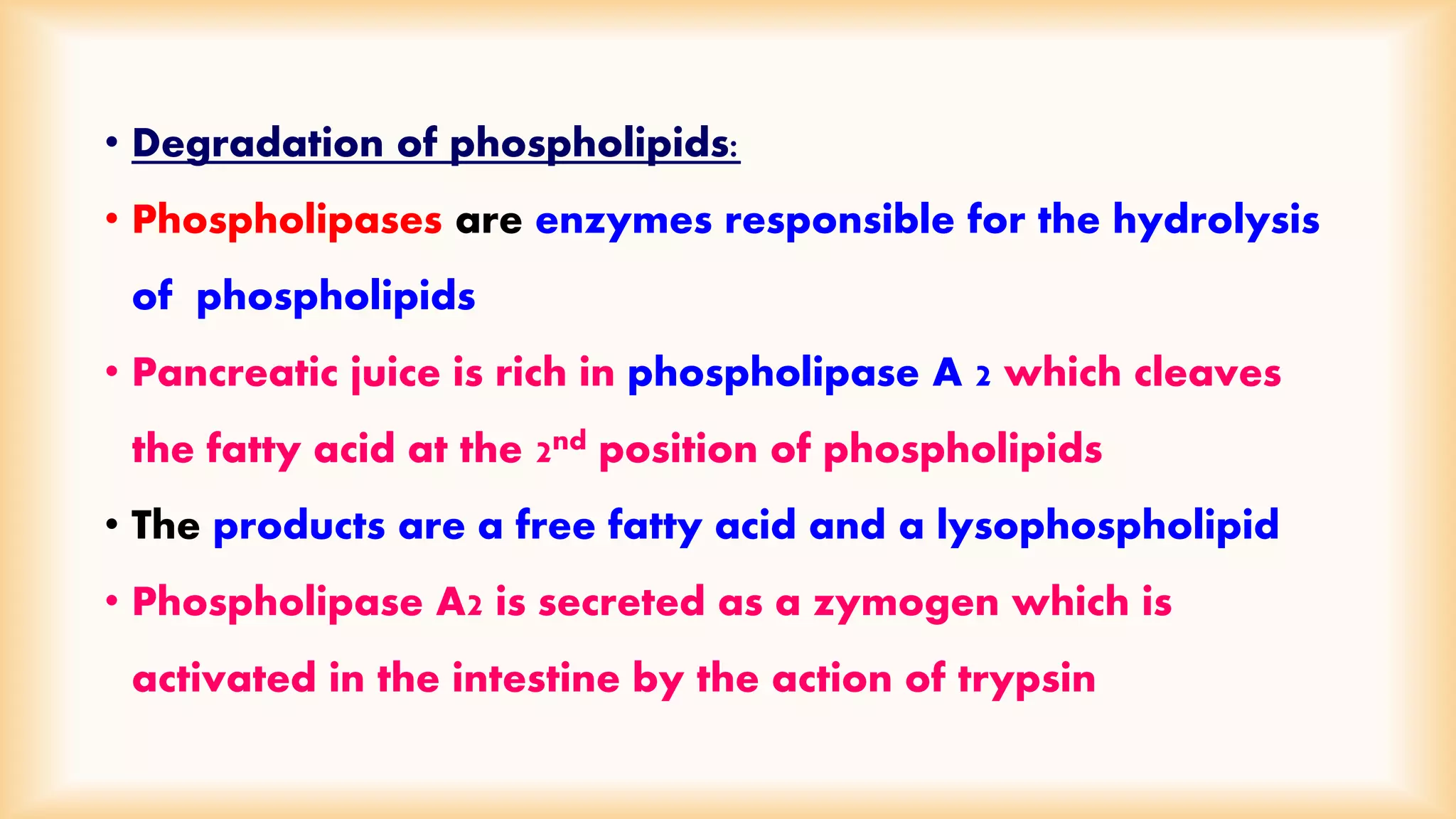
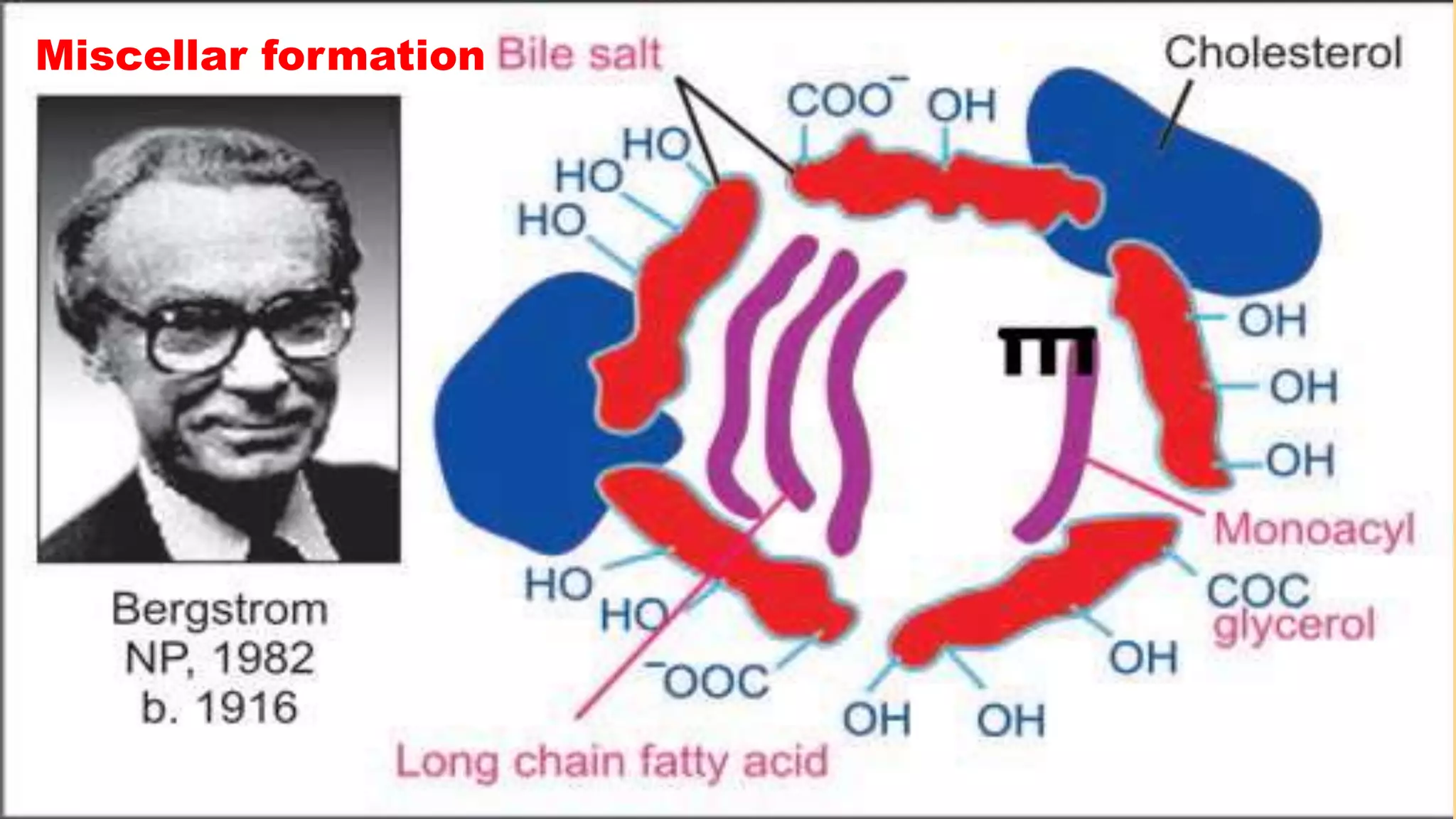
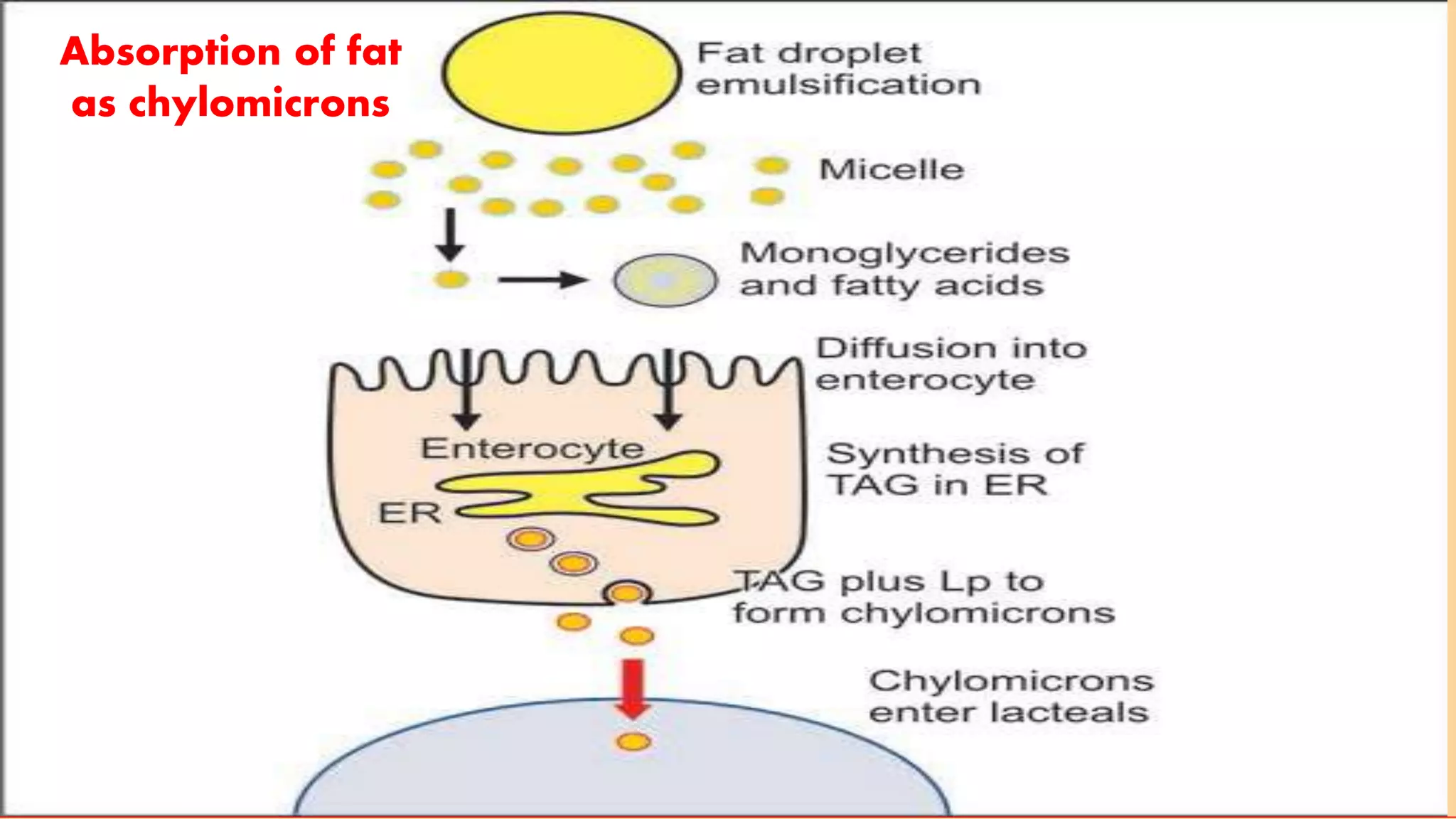
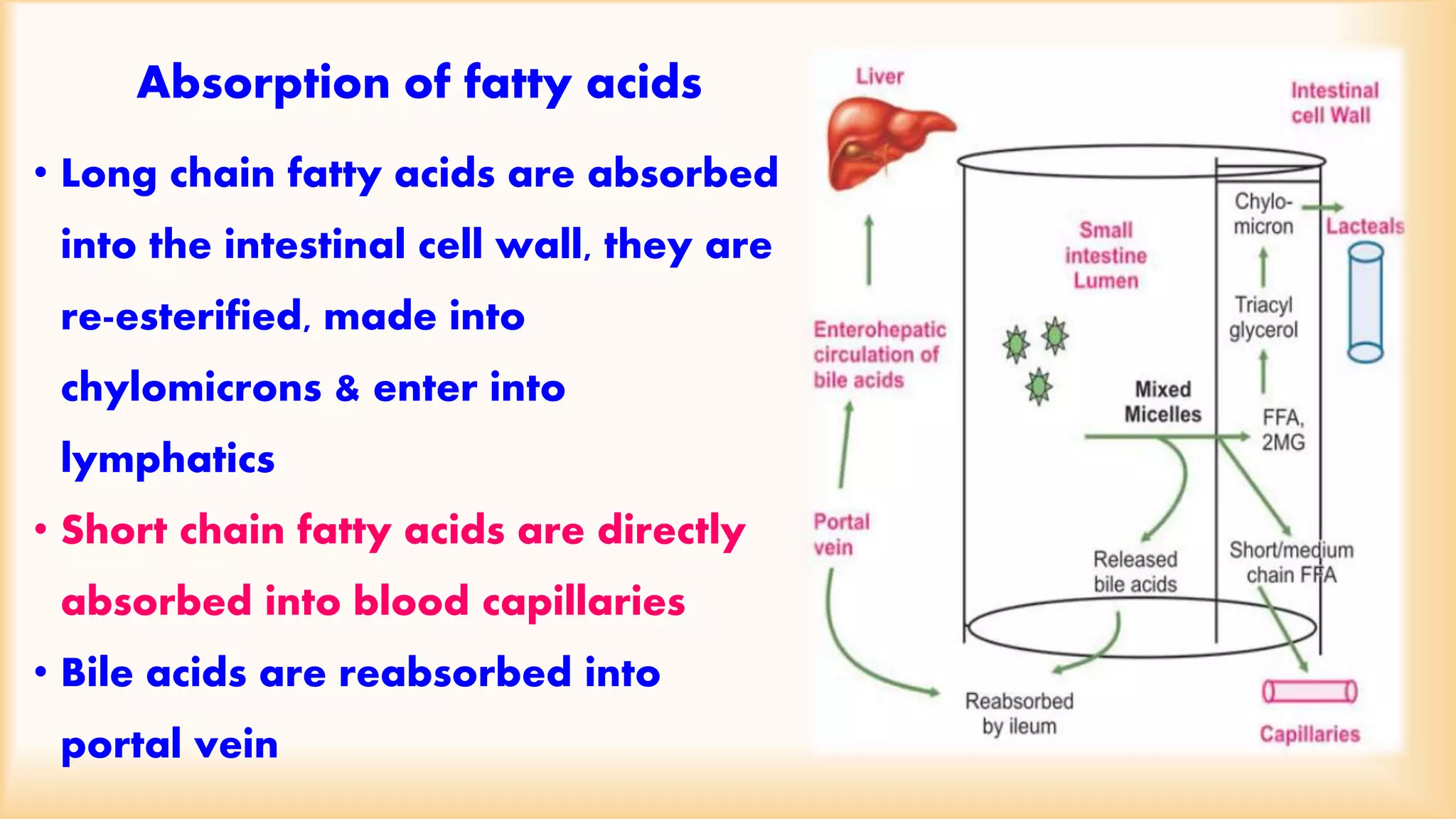
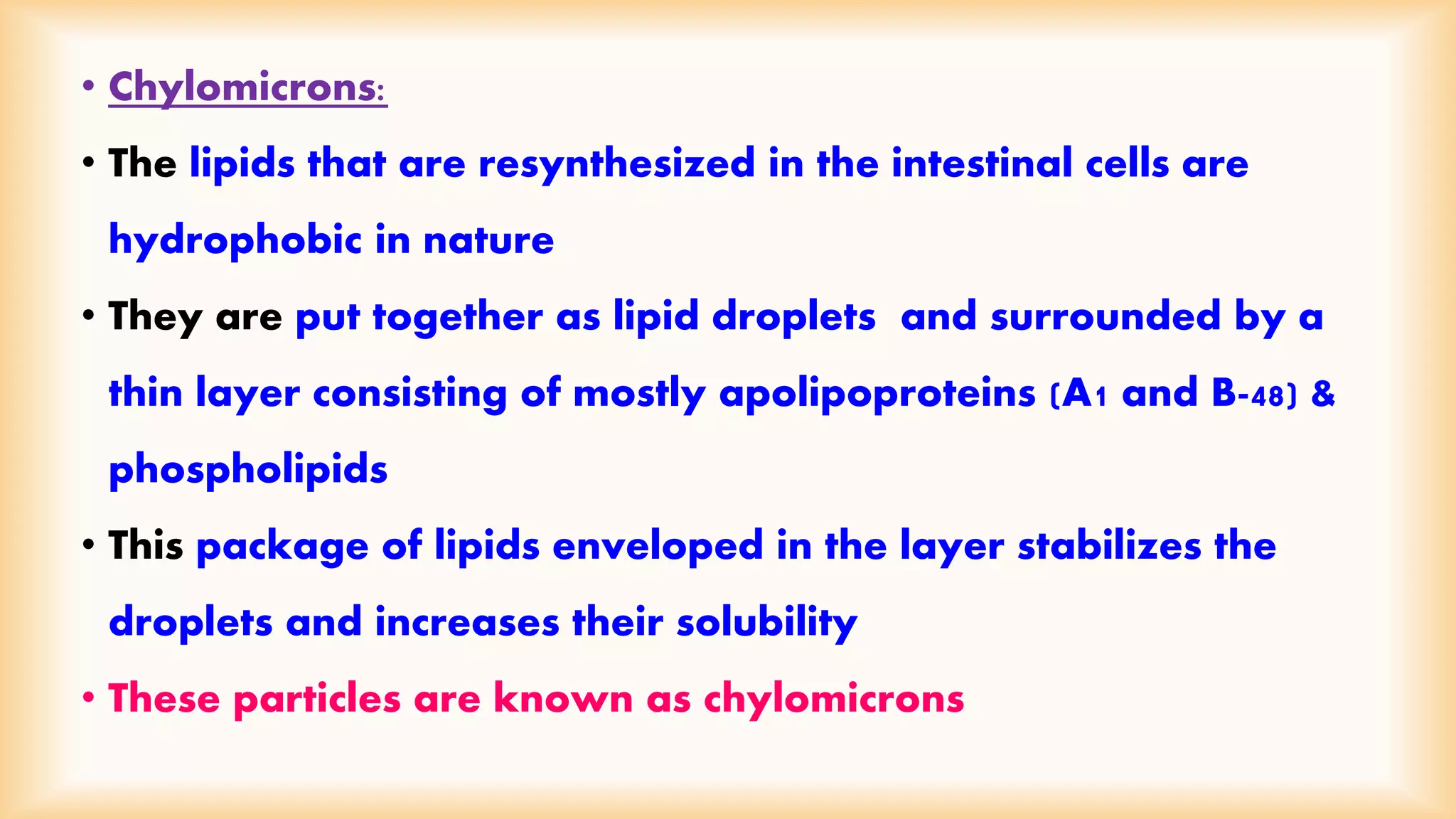
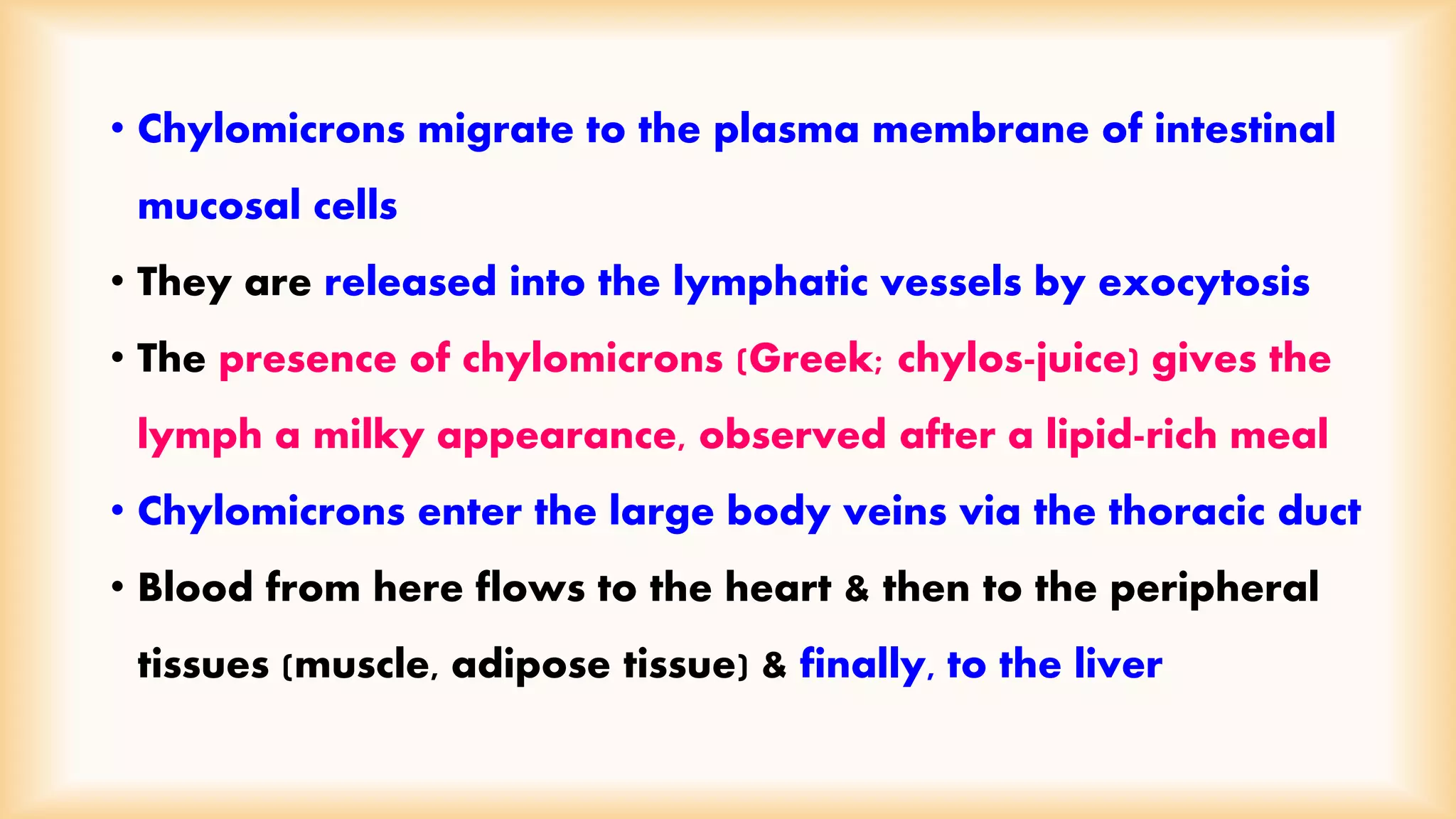
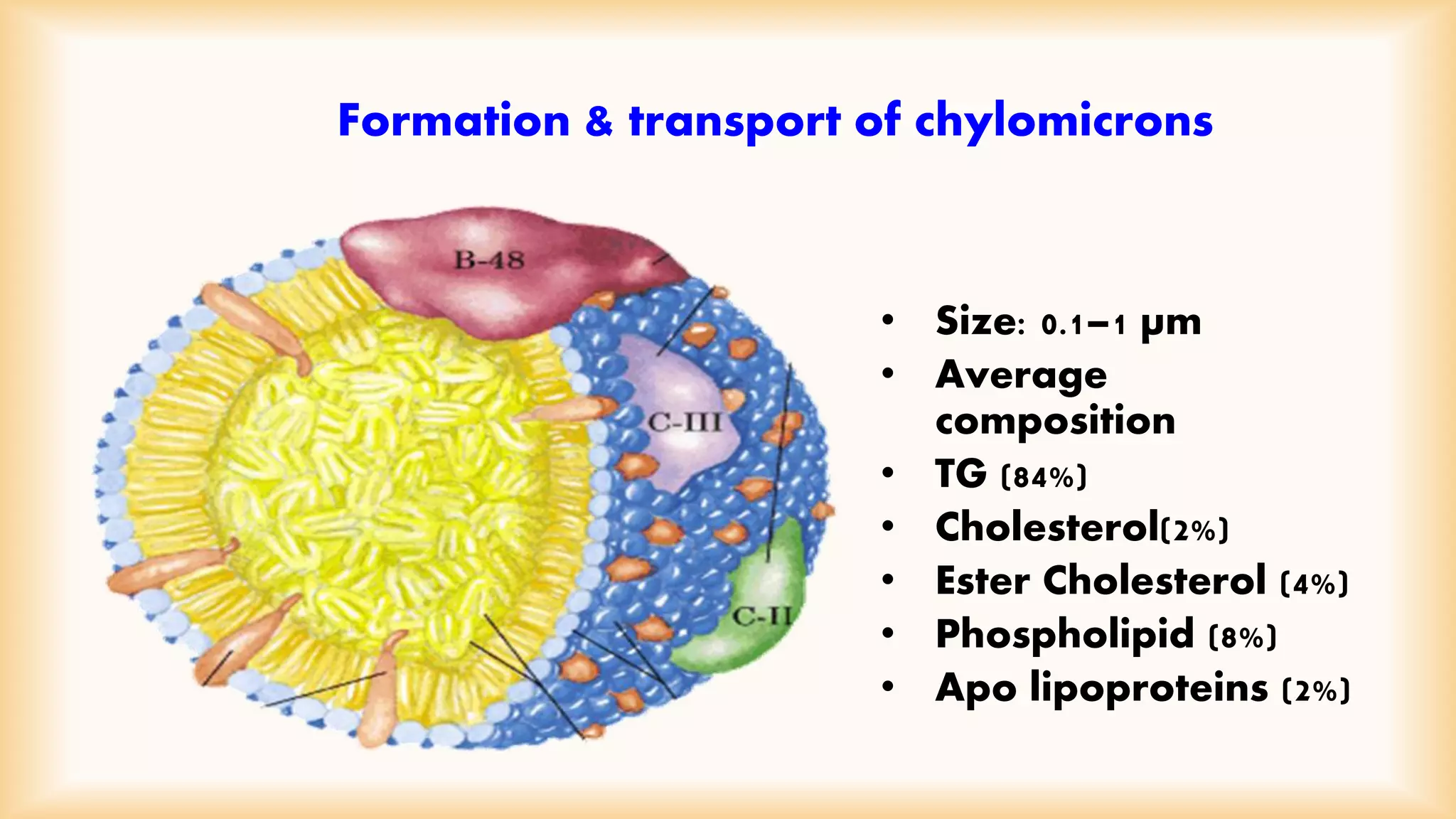
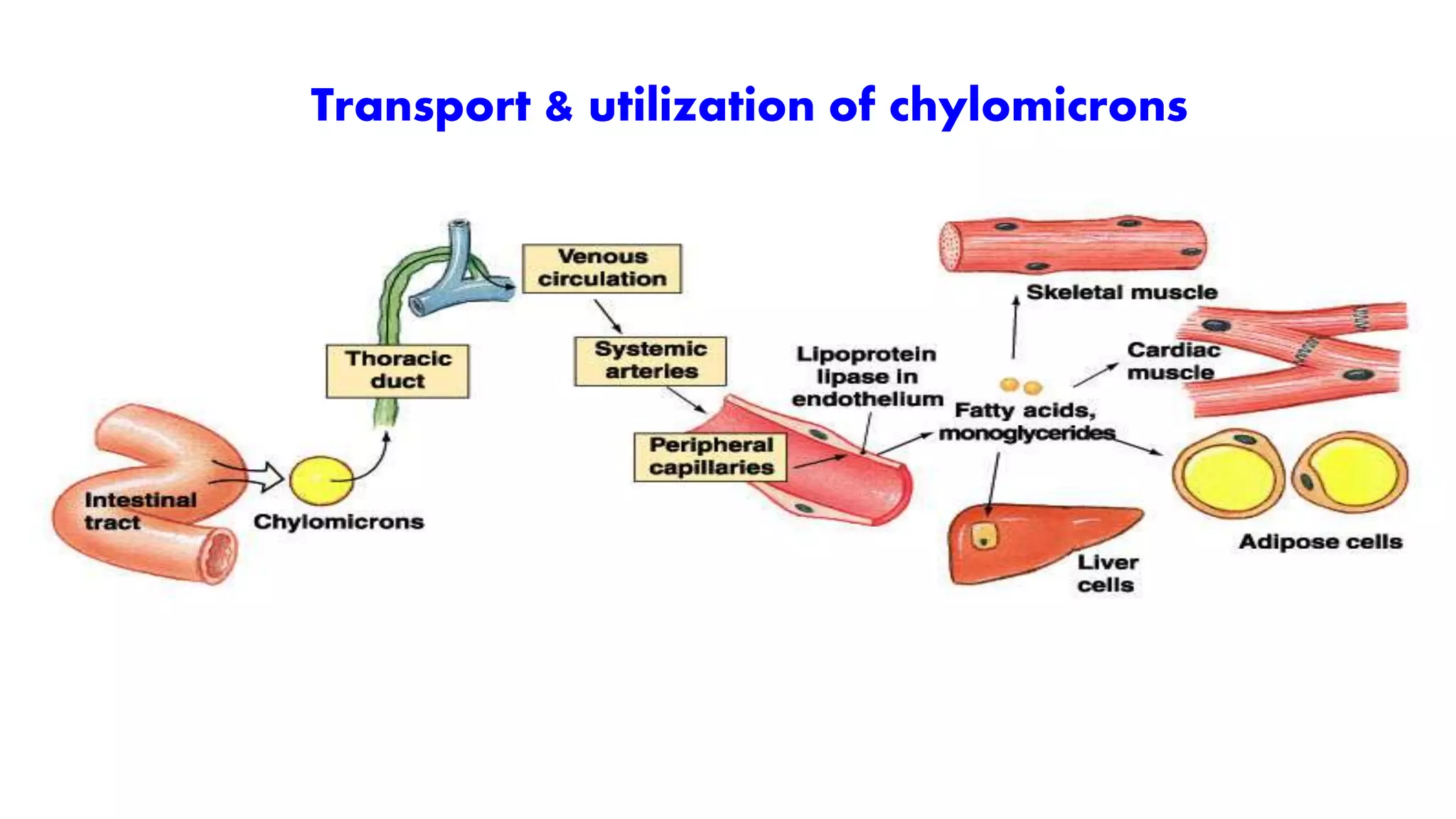
Lipids undergo a multi-step digestion and absorption process in the gastrointestinal tract. Dietary lipids are emulsified and broken down into smaller components like fatty acids and monoacylglycerols by lingual and gastric lipases in the stomach and pancreatic lipase in the small intestine. Bile salts produced by the liver play a key role in emulsification. The products of digestion are incorporated into micelles and absorbed by intestinal cells. Inside cells, fatty acids are reassembled into triglycerides and packaged into chylomicrons that enter the lymphatic system and bloodstream for transport to tissues. Defects in digestion, emulsification, or absorption can impair this process.