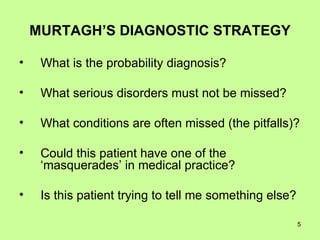
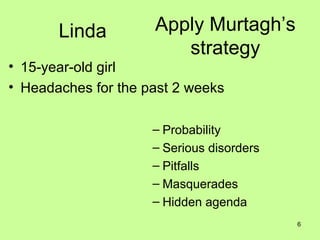
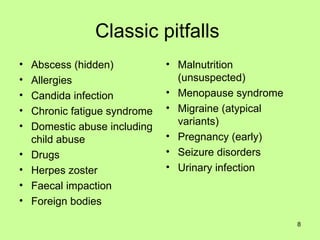
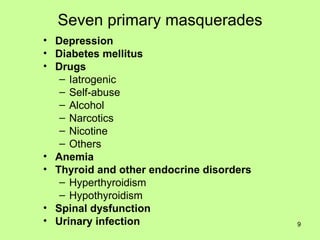
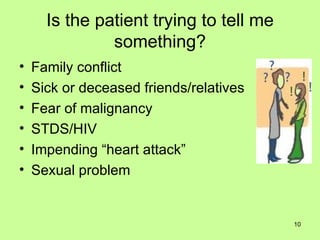
This document outlines Murtagh's diagnostic strategy for primary care physicians. It involves considering: 1) The probability diagnosis based on presenting symptoms, 2) Serious disorders that cannot be missed, 3) Conditions that are often overlooked or misdiagnosed, 4) Whether the patient's symptoms could represent a masquerade of another condition, and 5) If the patient may be indicating something else through their symptoms. It then provides an example of applying this strategy to a 15-year-old girl presenting with headaches.

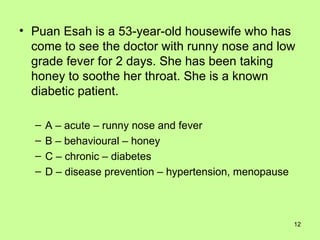
![The exceptional potential in each primary care consultation [Stott & Davis] A ACUTE presenting problems B BEHAVIORAL modification of health seeking behaviours C CHRONIC continuing problems D DISEASE PREVENTION opportunistic health promotion](https://image.slidesharecdn.com/tutbdiagnosticprocess-110526010436-phpapp02/85/Diagnostic-Process-11-320.jpg)