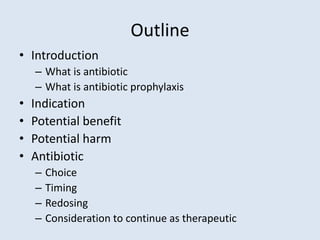
This document outlines the principles of antibiotic prophylaxis for surgery. It defines antibiotics and their prophylactic use to prevent surgical site infections. The potential benefits are listed as preventing infections, related morbidity and mortality, and reducing healthcare costs. Potential harms include allergic reactions and contributing to antibiotic resistance. Guidelines on antibiotic choice, timing, redosing, and considerations for continuing post-operatively are provided for common surgical procedures.