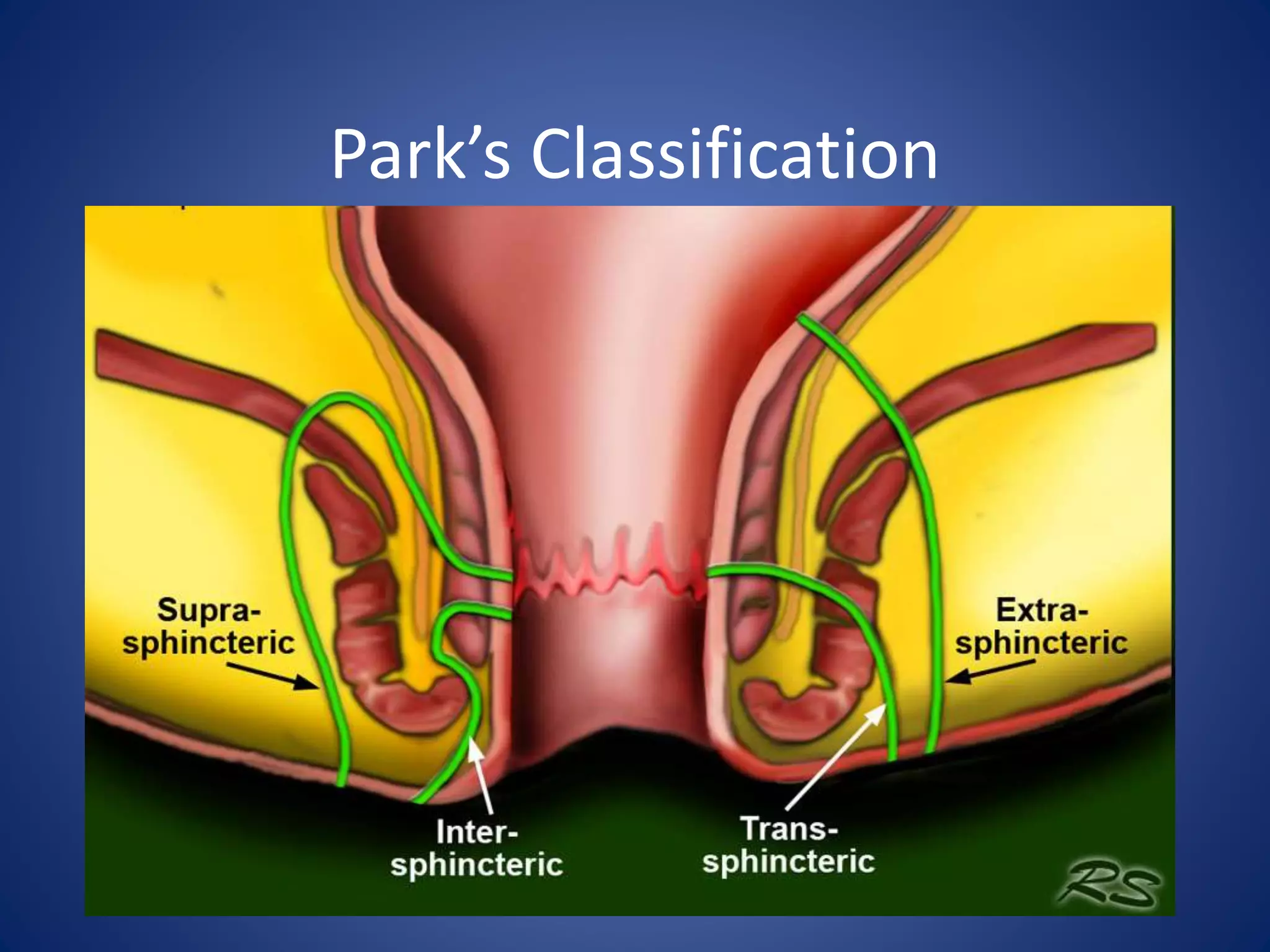
Here are the key steps in the clinical assessment of a fistula-in-ano:
1. Detailed history regarding present illness, bowel habits, abdominal/pelvic surgeries, trauma.
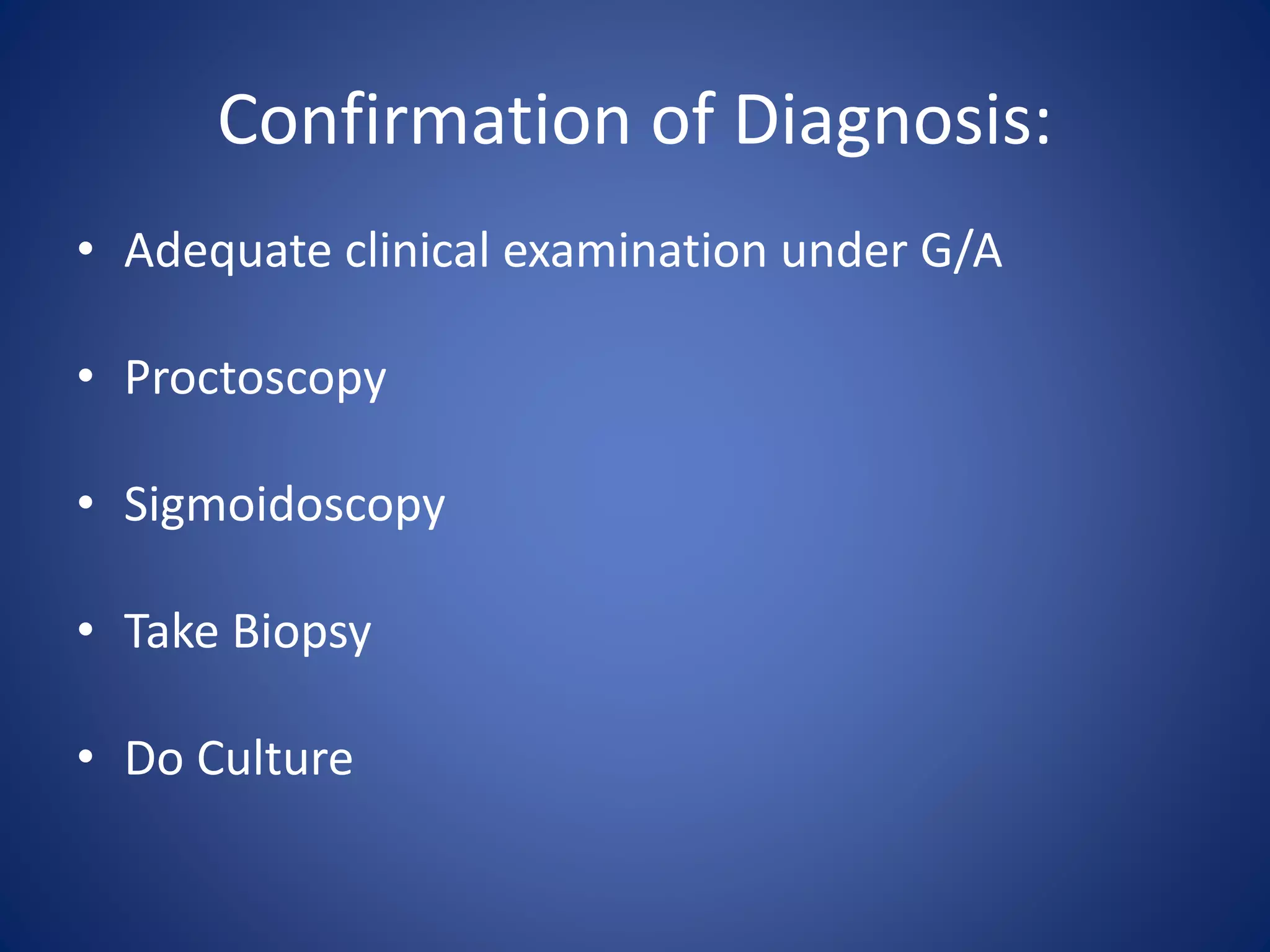
2. Digital rectal examination to identify internal opening and feel tract.
3. Proctoscopy/sigmoidoscopy to directly visualize internal opening.
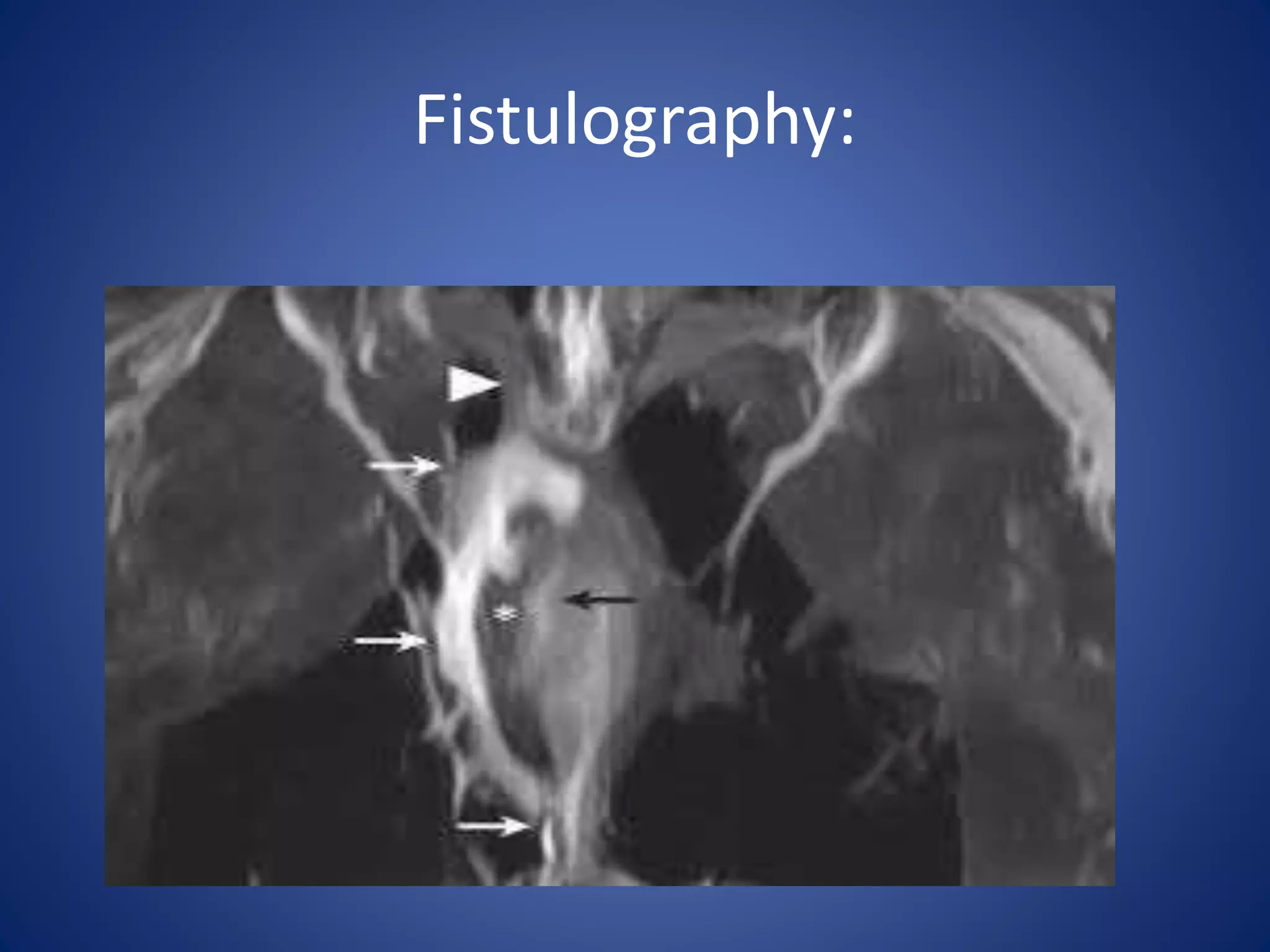
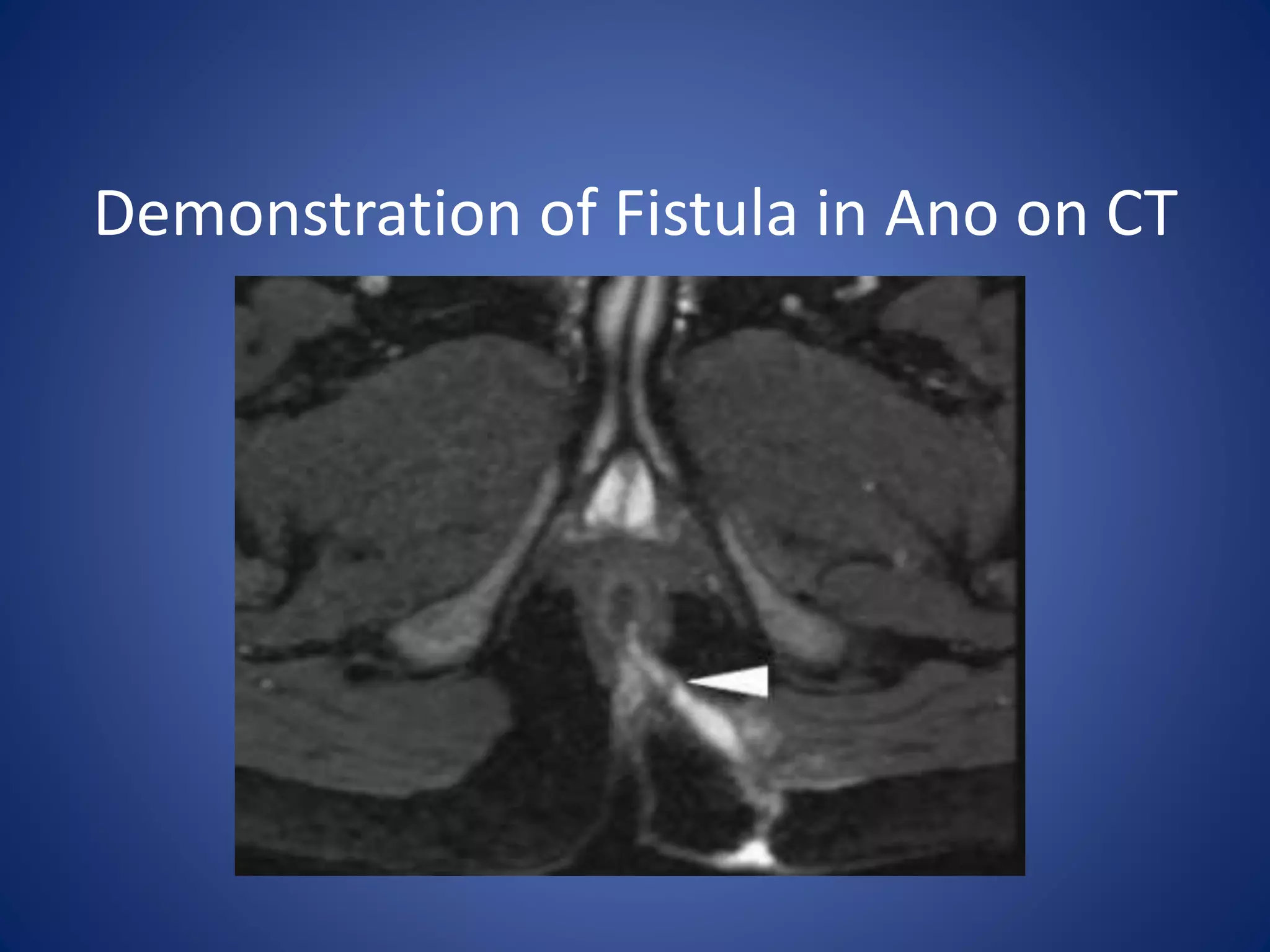
4. Imaging like MRI fistulogram to classify fistula and rule out other pelvic pathology.
5. Anorectal manometry and ultrasound to assess sphincter integrity if surgery is planned.
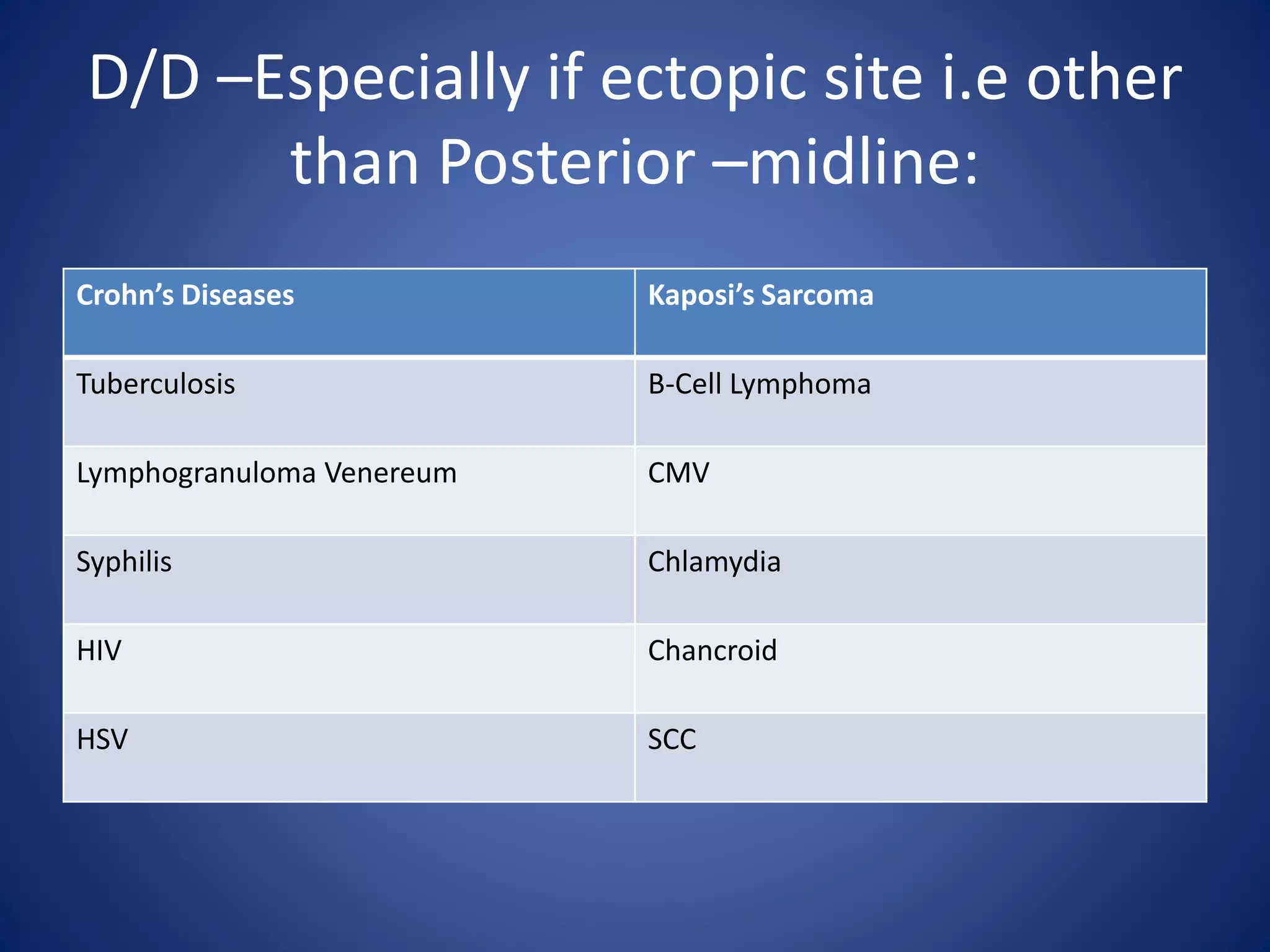
The clinical assessment aims to characterize the fistula anatomy, identify any underlying cause, assess sphincter function, and rule out alternative diagnoses to guide
































































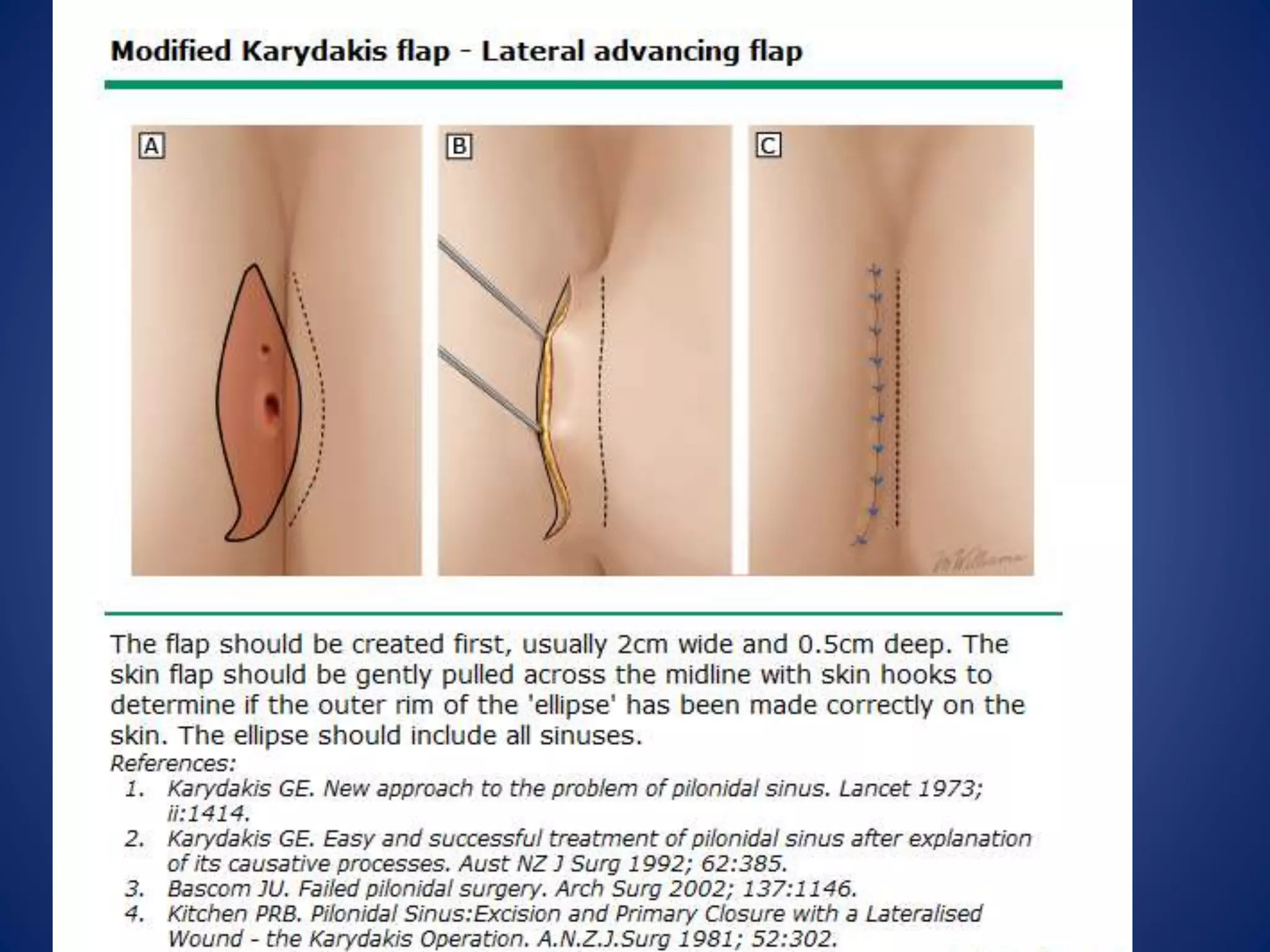


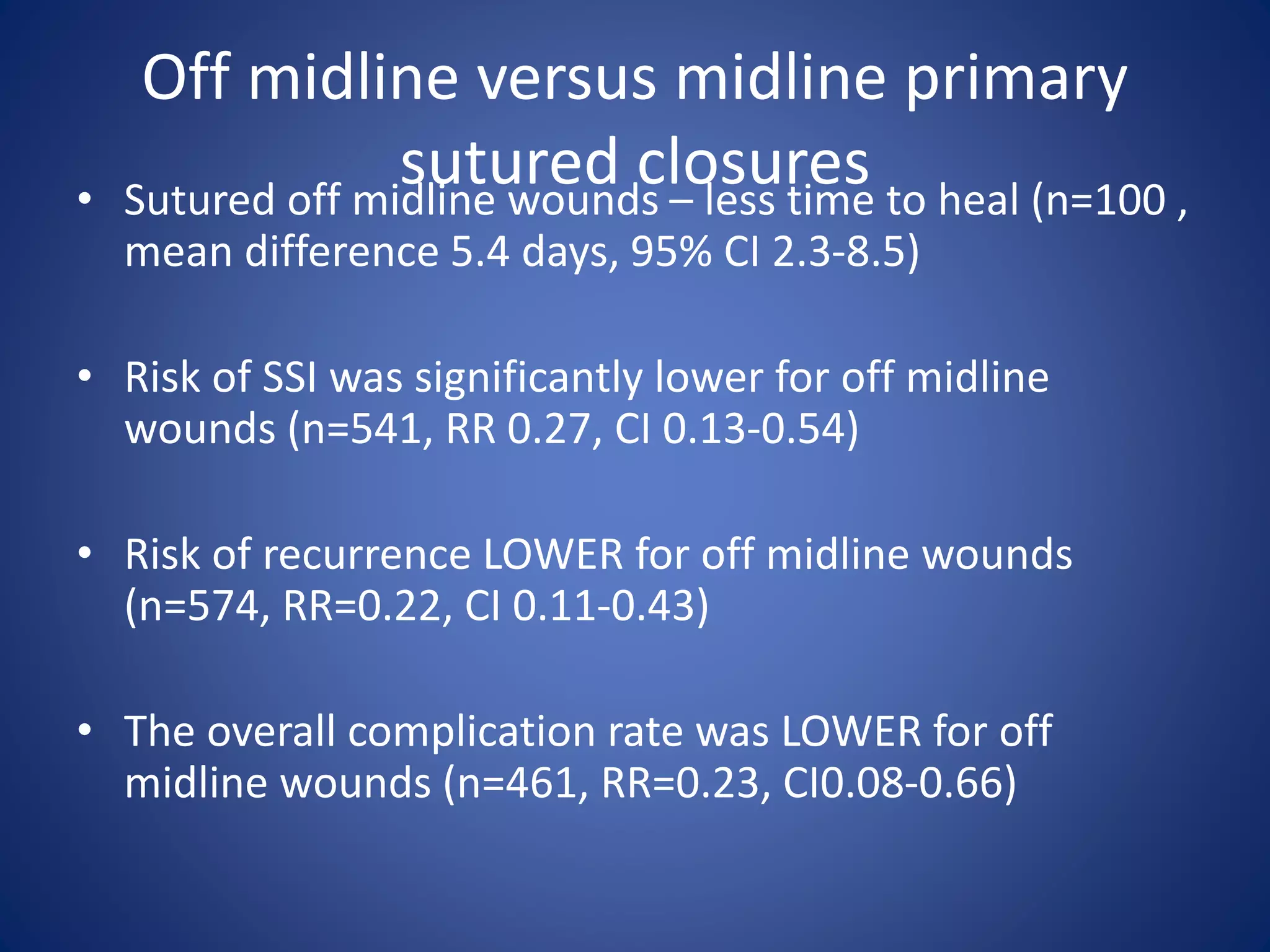
![• Recurrence rates:
- Based on 16 trials including 1666 patients , the
overall recurrence rate was 6.9%.
- Primary wound closure was associated with a
HIGHER recurrence rate compared to delayed
wound closure.
(8.7 versus 5.3 percent, relative risk RR [1.5]
CI1.08-2.17](https://image.slidesharecdn.com/fissureandfistula-171229131206/75/Fissure-and-fistula-110-2048.jpg)