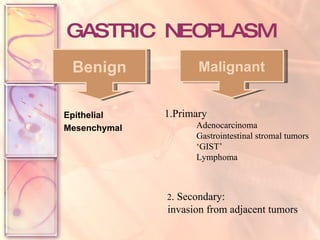
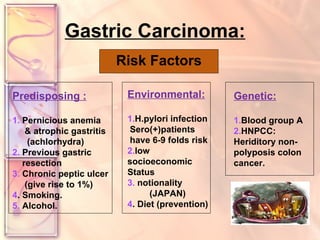
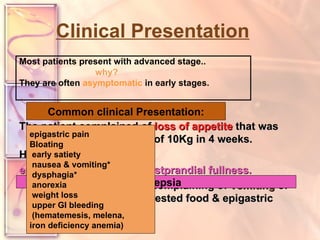
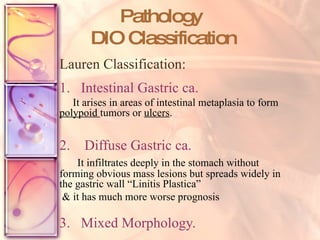
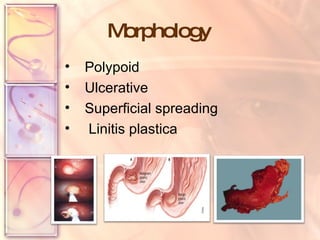
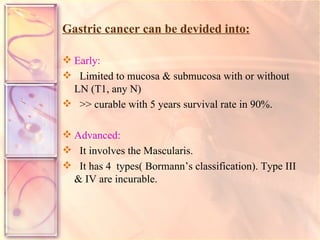
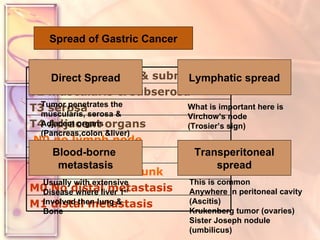
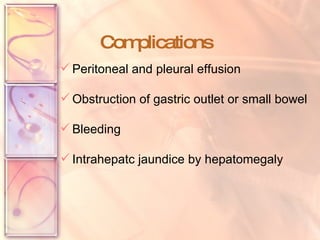
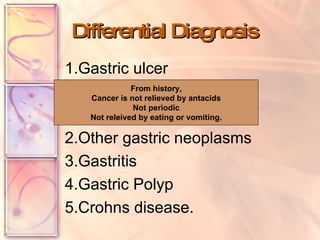
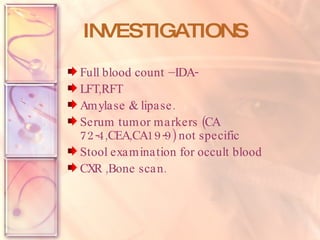
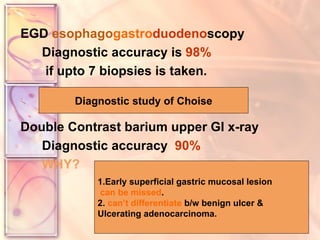
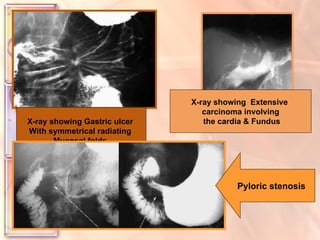
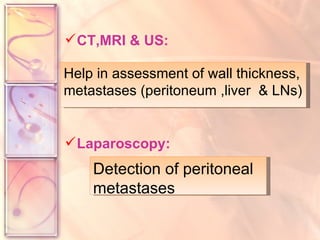
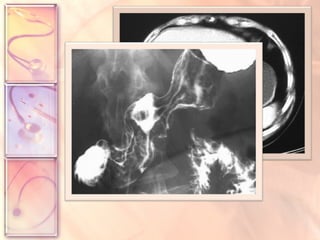
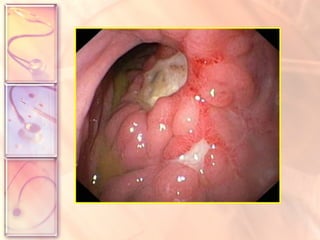
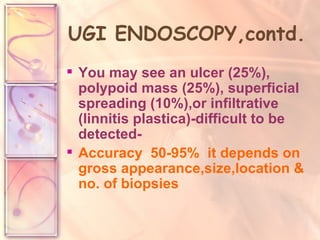
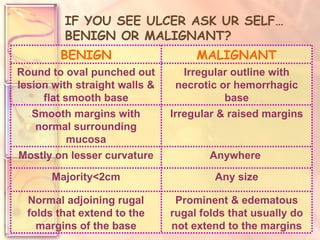
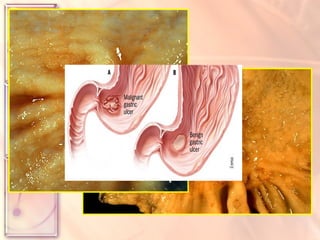
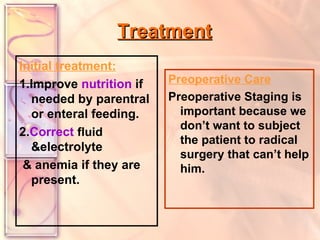
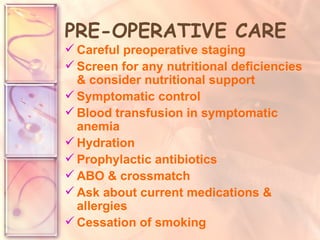
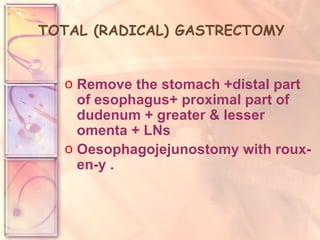
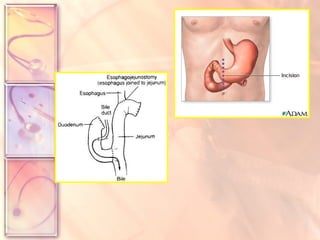
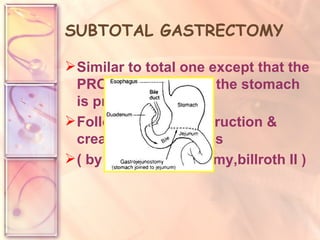
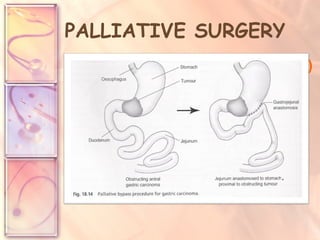
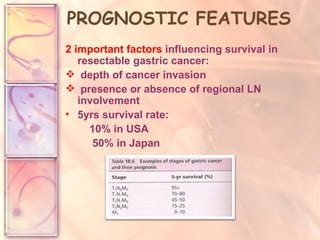
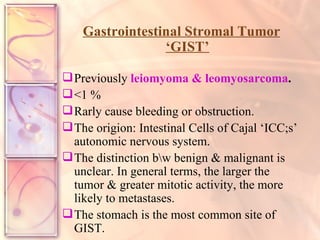
The document discusses gastric carcinoma (stomach cancer). It provides details on risk factors, clinical presentation, diagnostic testing including endoscopy, staging, treatment options including surgery, chemotherapy and radiation, complications, and prognostic factors. The highest rates of gastric cancer are seen in Japan, and it is more common in males and older individuals. Infection with H. pylori is a significant risk factor. Endoscopy with biopsy is the gold standard for diagnosis. Treatment depends on staging but may include surgery such as total or subtotal gastrectomy. Prognosis depends on depth of invasion and lymph node involvement.