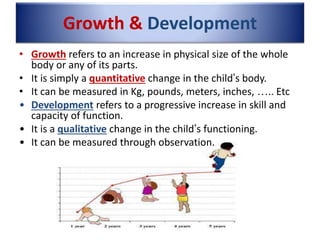
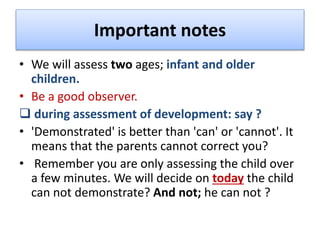
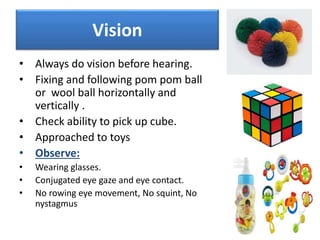
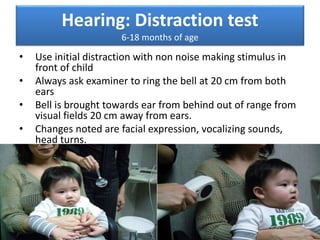
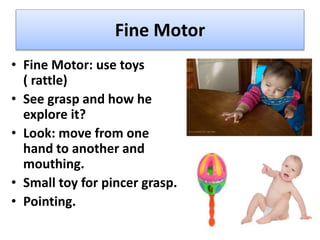
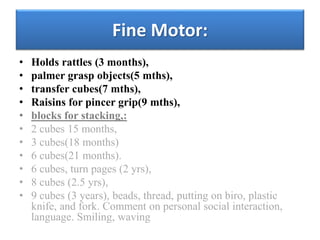
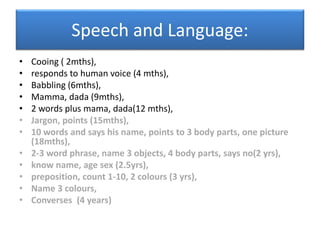
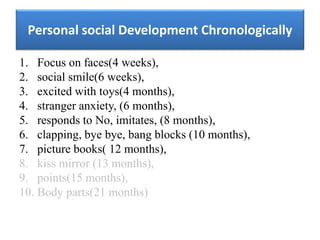
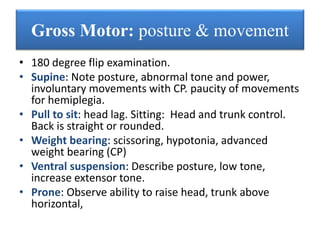
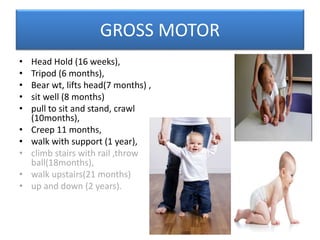
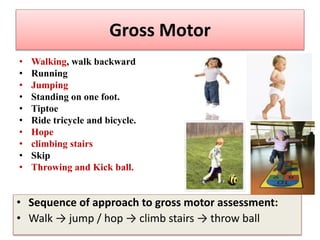
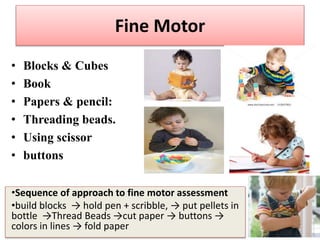
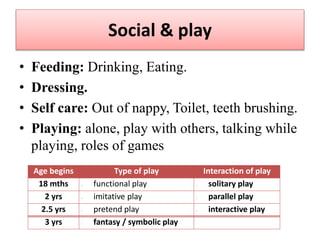
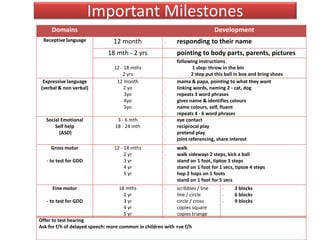
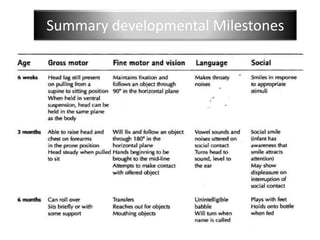
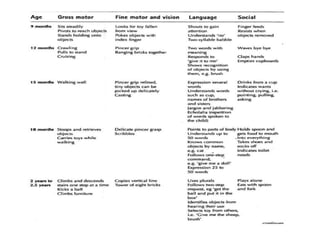
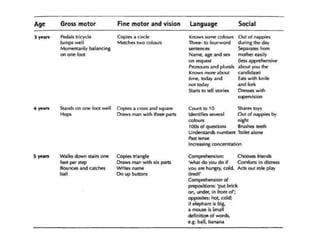
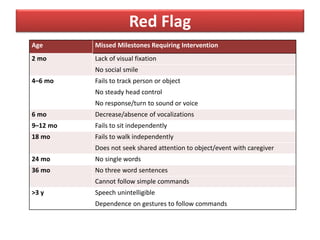
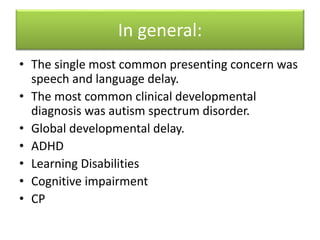
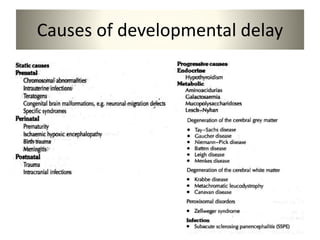
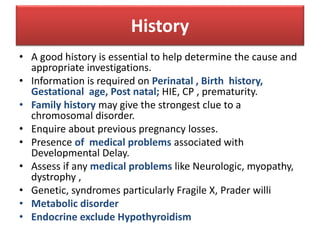
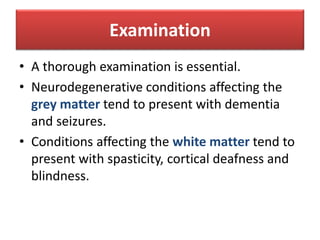
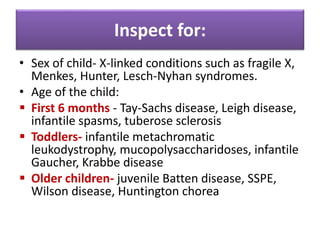
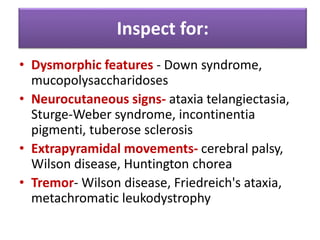
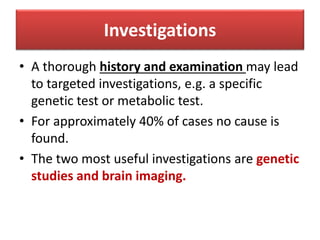
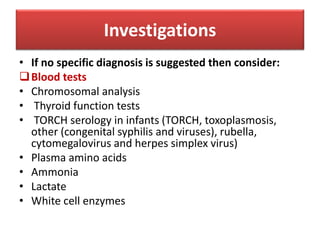
The document discusses growth and development in children. It defines growth as a quantitative increase in size, while development refers to qualitative improvements in skills and abilities. Four developmental domains are identified: gross motor, fine motor, language, and cognitive/social skills. Assessment tools for infants and older children are listed. The summary should assess development in these key areas and note the importance of a thorough history and examination to evaluate causes of developmental delay.