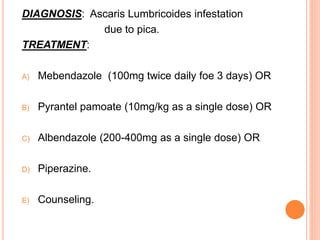
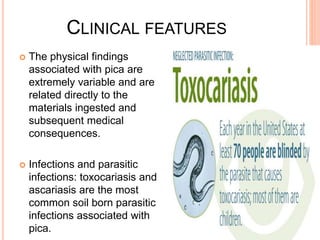
A 5-year-old girl with abdominal pain and eosinophilia was diagnosed with Ascaris lumbricoides infestation due to pica, a condition involving the ingestion of non-nutritive substances like soil. Treatment options include medications such as mebendazole, pyrantel pamoate, and albendazole, along with counseling. Pica can lead to various complications, including nutritional deficiencies and parasitic infections, and is more common in children with developmental issues.