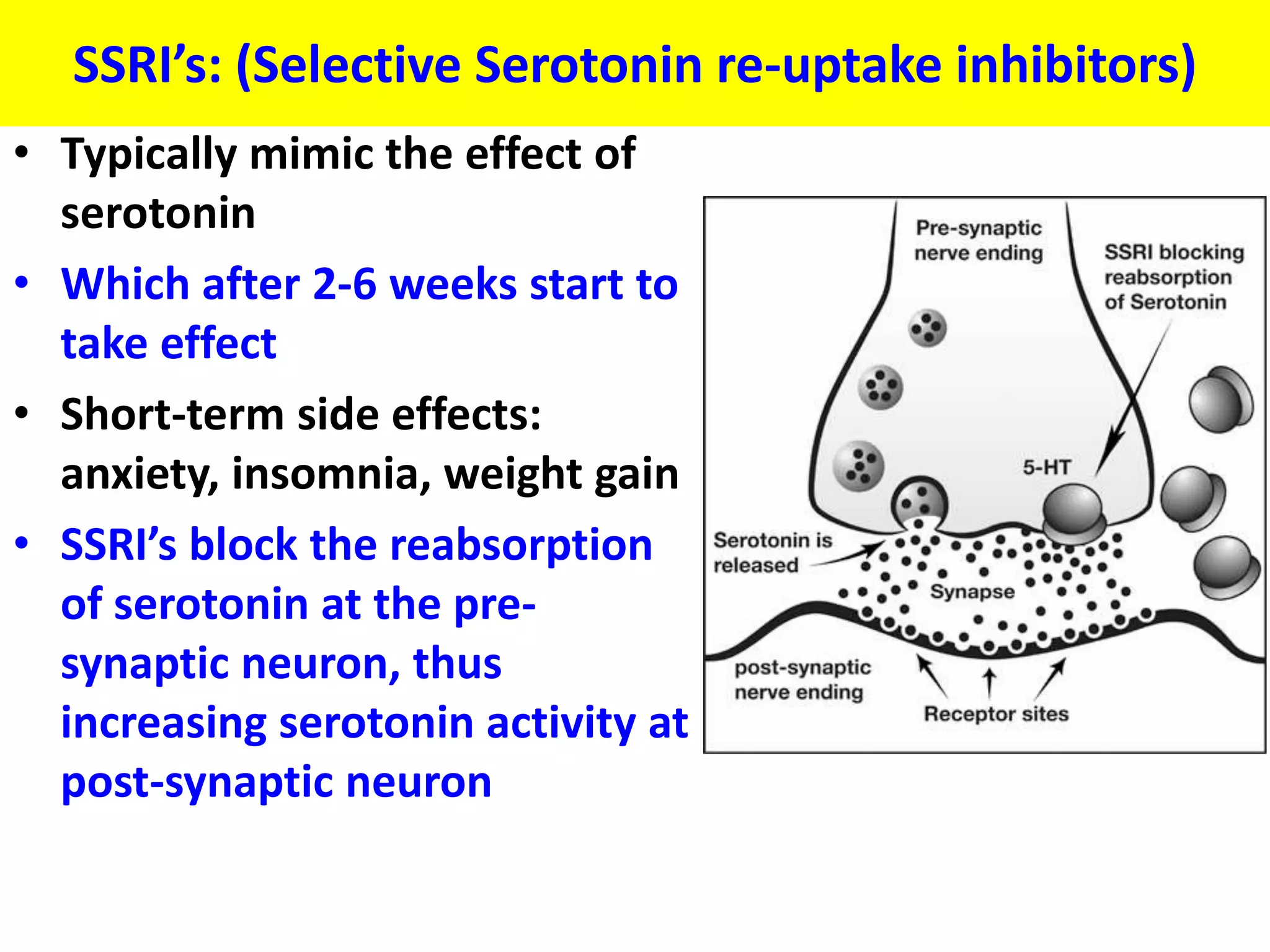
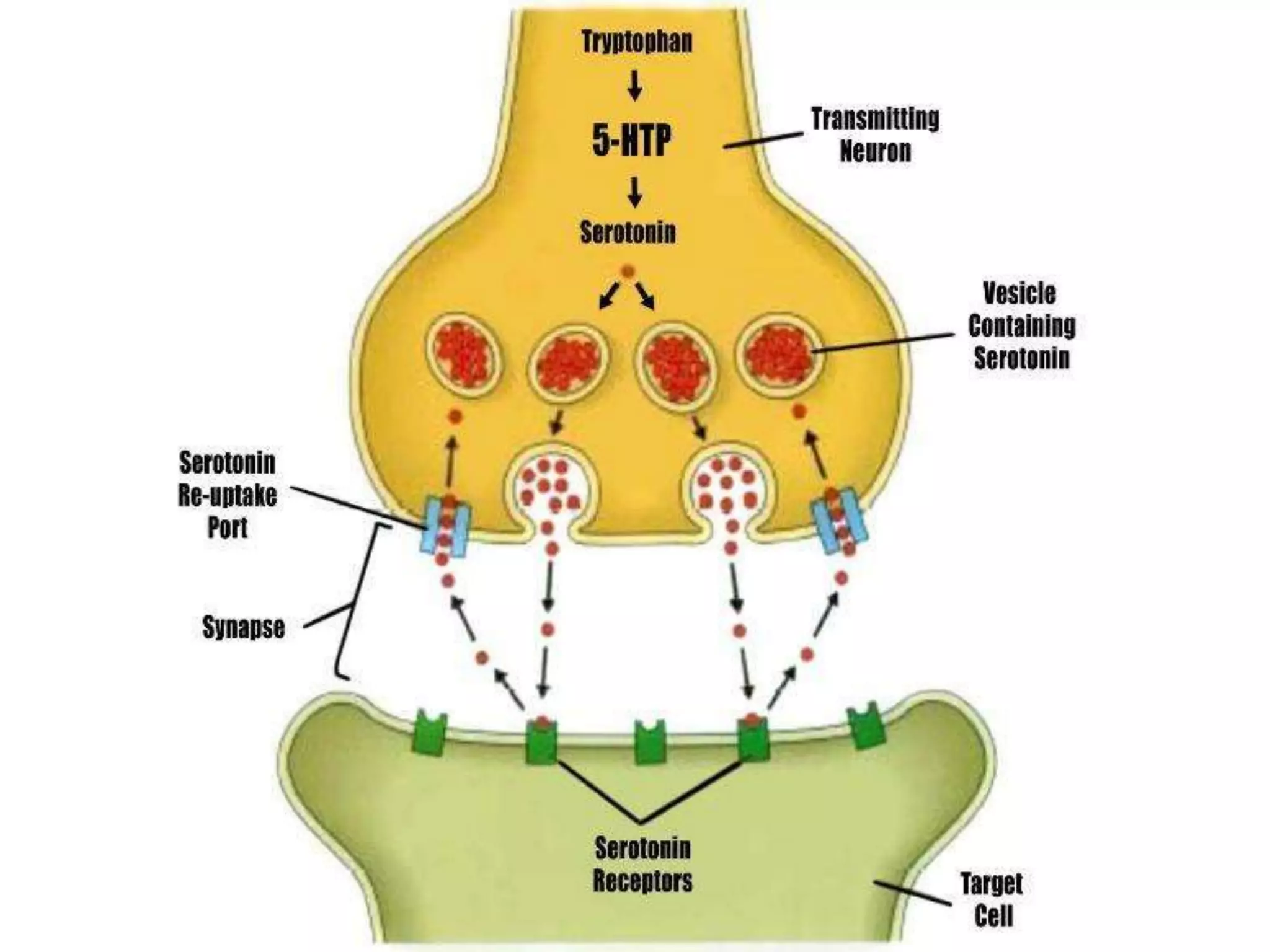
The document outlines the symptoms of depression, including thoughts of suicide, anhedonia, fatigue, and changes in weight and sleep patterns that must persist for at least two weeks. It discusses biological triggers such as genetic factors and neurotransmitter imbalances, particularly low serotonin and norepinephrine levels. Additionally, it describes the use of selective serotonin re-uptake inhibitors (SSRIs) as treatment, including their mechanism and potential short-term side effects.