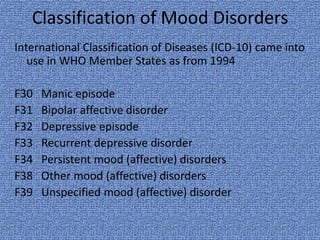
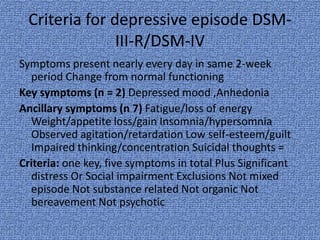
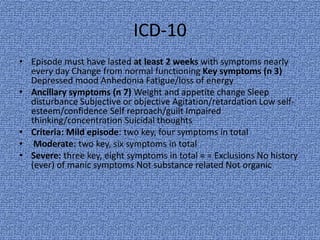
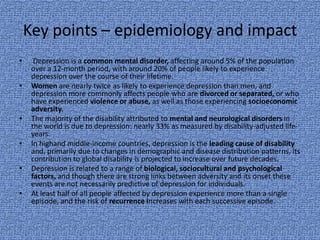
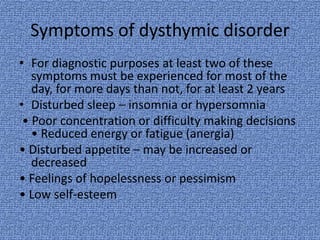
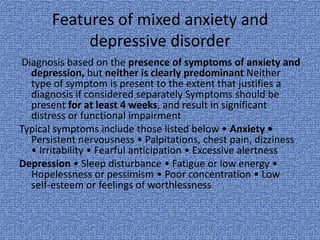
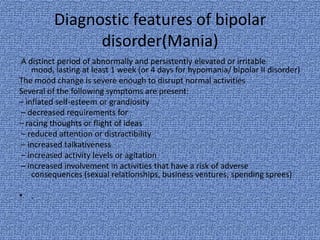
The document summarizes classification systems and diagnostic criteria for various mood disorders according to the ICD-10 and DSM-III-R/DSM-IV, including major depressive disorder, dysthymic disorder, mixed anxiety-depressive disorder, bipolar disorder, and discusses epidemiology, symptoms, and treatment options.